Abstract
Parkinson’s disease is a chronic neurodegenerative movement disorder affecting people mainly beyond their 50s. Geriatric patients with Parkinson’s disease experience a specific profile of comorbidities. Multimorbidity and resulting polypharmacotherapy are frequent at this age. Comorbid diseases, widely spread, involve arterial hypertension, ischemic heart disease, heart failure, atrial fibrillation, polyneuropathy, diabetes mellitus, cerebrovascular disease, sarcopenia, and frailty. Following years of drug development, levodopa is still the most effective drug for the treatment of motor symptoms. However, a wide range of other drugs are available with specific effects, contraindications, and complications. The treatment of geriatric patients with Parkinson’s disease is challenging and requires the cooperation of multidisciplinary teams. A careful assessment of a patient’s Parkinson’s disease symptoms, comorbidities, medication, vital signs, and resources is crucial for an effective and safe therapy. Laboratory tests can assist in the identification of contraindications for specific treatments. Identifying potentially inadequate drugs from prescription lists can lead to a better targeted treatment for geriatric patients with Parkinson’s disease. Future research should help develop a more evidence-based therapy of geriatric patients with Parkinson’s disease. For this purpose, randomized controlled trials of geriatric patients are urgently needed. An international register concerning issues of safer drug application and monitoring could help to implement a better treatment.


Similar content being viewed by others
References
de Lau LML, Breteler MMB. Epidemiology of Parkinson’s disease. Lancet Neurol. 2006;5:525–35.
Nussbaum RL, Ellis CE. Alzheimer’s disease and Parkinson’s disease. N Engl J Med. 2003;348:1356–64.
Politis M, Wu K, Molloy S, Bain PG, Chaudhuri KR, Piccini P. Parkinson’s disease symptoms: the patients perspective. Mov Disord. 2010;25:1646–51.
Forsaa EB, Larsen JP, Wentzel-Larsen T, Herlofson K, Alves G. Predictors and course of health-related quality of life in Parkinson’s disease. Mov Disord. 2008;23:1420–7.
Soh S-E, Morris ME, McGinley JL. Determinants of health-related quality of life in Parkinson’s disease: a systematic review. Parkinsonism Relat Disord. 2011;17:1–9.
Klietz M, Tulke A, Müschen LH, Paracka L, Schrader C, Dressler DW, et al. Impaired quality of life and need for palliative care in a German cohort of advanced Parkinson’s disease patients. Front Neurol. 2018;9:120.
Kempster PA, O’Sullivan SS, Holton JL, Revesz T, Lees AJ. Relationships between age and late progression of Parkinson’s disease: a clinico-pathological study. Brain. 2010;133:1755–62.
Muller-Rebstein S, Trenkwalder C, Oertel WH, Culmsee C, Eckermann G, Höglinger GU. Pharmacotherapy of Parkinson’s disease: aspects of drug safety. Nervenarzt. 2017;88:888–94.
Giugni JC, Okun MS. Treatment of advanced Parkinsonʼs disease. Curr Opin Neurol. 2014;27:450–60.
Lingor P, Csoti I, Koschel J, Schrader C, Winkler C, Wolz M, et al. The geriatric patient with Parkinson’s disease: a neurological challenge. Fortschr Neurol Psychiatry. 2016;84(Suppl. 1):S41–7.
Jakovljevic M, Ostojic L. Comorbidity and multimorbidity in medicine today: challenges and opportunities for bringing separated branches of medicine closer to each other. Psychiatr Danub. 2013;25(Suppl. 1):18–28.
Dodel R. Multimorbidity: concept, epidemiology and treatment. Nervenarzt. 2014;85:401–8.
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43.
Hou JG, Wu LJ, Moore S, Ward C, York M, Atassi F, et al. Assessment of appropriate medication administration for hospitalized patients with Parkinson’s disease. Parkinsonism Relat Disord. 2012;18:377–81.
McLean G, Hindle JV, Guthrie B, Mercer SW. Co-morbidity and polypharmacy in Parkinson’s disease: insights from a large Scottish primary care database. BMC Neurol. 2017;17:126.
Choi J, Ahn A, Kim S, Won CW. Global prevalence of physical frailty by Fried’s criteria in community-dwelling elderly with national population-based surveys. J Am Med Dir Assoc. 2015;16:548–50.
Santos-Eggimann B, Cuenoud P, Spagnoli J, Junod J. Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. J Gerontol A Biol Sci Med Sci. 2009;64:675–81.
Peball M, Mahlknecht P, Werkmann M, Marini K, Murr F, Herzmann H, et al. Prevalence and associated factors of sarcopenia and frailty in Parkinson’s disease: a cross-sectional study. Gerontology. 2018. https://doi.org/10.1159/000492572 (Epub ahead of print).
Riedel O, Dodel R, Deuschl G, Förstl H, Henn F, Heuser I, et al. Dementia and depression determine care dependency in Parkinson’s disease: analysis of 1,449 outpatients receiving nursing care in Germany. Nervenarzt. 2011;82:1012–9.
Riedel O, Dodel R, Deuschl G, Klotsche J, Förstl H, Heuser I, et al. Depression and care-dependency in Parkinson’s disease: results from a nationwide study of 1449 outpatients. Parkinsonism Relat Disord. 2012;18:598–601.
Leibson CL, Maraganore DM, Bower JH, Ransom JE, O’Brien PC, Rocca WA. Comorbid conditions associated with Parkinson’s disease: a population-based study. Mov Disord. 2005;21:446–55.
Tönges L, Bartig D, Muhlack S, Jost W, Gold R, Krogias C. Characteristics and dynamics of inpatient treatment of patients with Parkinson’s disease in Germany: analysis of 1.5 million patient cases from 2010 to 2015. Nervenarzt. 2018;2018(16):552.
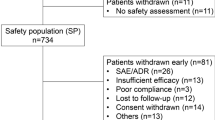
Müller-Rebstein S, Trenkwalder C, Ebentheuer J, Oertel WH, Culmsee C, Höglinger GU. Drug safety analysis in a real-life cohort of Parkinson’s disease patients with polypharmacy. CNS Drugs. 2018;31:1093–102.
Balzer-Geldsetzer M, Ferreira J, Odin P, Bloem BR, Meissner WG, Lorenzl S, et al. Study protocol: Care of Late-Stage Parkinsonism (CLaSP): a longitudinal cohort study. BMC Neurol. 2018;18:185.
Zesiewicz TA, Strom JA, Borenstein AR, Hauser RA, Cimino CR, Fontanet HL, et al. Heart failure in Parkinson’s disease: analysis of the United States Medicare current beneficiary survey. Parkinsonism Relat Disord. 2004;10:417–20.
Santiago JA, Bottero V, Potashkin JA. Biological and clinical implications of comorbidities in Parkinson’s disease. Front Aging Neurosci. 2017;9:394.
Lai S-W, Lin C-L, Liao K-F, Chang-Ou K-C. Increased risk of Parkinson’s disease in cataract patients: a population-based cohort study. Parkinsonism Relat Disord. 2015;21:68–71.
Jellinger KA. Prevalence of cerebrovascular lesions in Parkinson’s disease: a postmortem study. Acta Neuropathol. 2003;105:415–9.
Hong CT, Hu H-H, Chan L, Bai C-H. Prevalent cerebrovascular and cardiovascular disease in people with Parkinson’s disease: a meta-analysis. Clin Epidemiol. 2018;10:1147–54.
Ebersbach G, Sojer M, Muller J, Ransmayr G, Wenning G, Poewe W. Dysequilibrium in idiopathic Parkinson disease: the effect of cerebrovascular comorbidity. Nervenarzt. 2002;73:162–5.
Kotagal V, Albin RL, Muller MLTM, Koeppe RA, Studenski S, Frey KA, et al. Advanced age, cardiovascular risk burden, and Timed Up and Go Test performance in Parkinson disease. J Gerontol A Biol Sci Med Sci. 2014;69:1569–75.
Hu G, Jousilahti P, Bidel S, Antikainen R, Tuomilehto J. Type 2 diabetes and the risk of Parkinson’s disease. Diabetes Care. 2007;30:842–7.
Cereda E, Barichella M, Cassani E, Caccialanza R, Pezzoli G. Clinical features of Parkinson disease when onset of diabetes came first: a case–control study. Neurology. 2012;78:1507–11.
Kotagal V, Albin RL, Müller MLTM, Koeppe RA, Frey KA, Bohnen NI. Diabetes is associated with postural instability and gait difficulty in Parkinson disease. Parkinsonism Relat Disord. 2013;19:522–6.
Bohnen NI, Kotagal V, Müller MLTM, Koeppe RA, Scott PJH, Albin RL, et al. Diabetes mellitus is independently associated with more severe cognitive impairment in Parkinson disease. Parkinsonism Relat Disord. 2014;20:1394–8.
Metta V, Sanchez TC, Padmakumar C. Osteoporosis: a hidden nonmotor face of Parkinson’s disease. Int Rev Neurobiol. 2017;134:877–90.
Deng Q, Zhou X, Chen J, Pan M, Gao H, Zhou J, et al. Lower hemoglobin levels in patients with Parkinson’s disease are associated with disease severity and iron metabolism. Brain Res. 2017;1655:145–51.
Wielinski CL, Erickson-Davis C, Wichmann R, Walde-Douglas M, Parashos SA. Falls and injuries resulting from falls among patients with Parkinson’s disease and other parkinsonian syndromes. Mov Disord. 2005;20:410–5.
Huang Y-F, Cherng Y-G, Hsu SPC, Yeh C-C, Chou Y-C, Wu C-H, et al. Risk and adverse outcomes of fractures in patients with Parkinson’s disease: two nationwide studies. Osteoporos Int. 2015;26:1723–32.
Abbott A. Levodopa: the story so far. Nature. 2010;466:S6–7.
Hornykiewicz O. Dopamine miracle: from brain homogenate to dopamine replacement. Mov Disord. 2002;17:501–8.
Hauser RA. Levodopa: past, present, and future. Eur Neurol. 2009;62:1–8.
Nutt JG, Fellman JH. Pharmacokinetics of levodopa. Clin Neuropharmacol. 1984;7:35–49.
Cedarbaum JM. Clinical pharmacokinetics of anti-parkinsonian drugs. Clin Pharmacokinet. 1987;13:141–78.
Wood LD. Clinical review and treatment of select adverse effects of dopamine receptor agonists in Parkinson’s disease. Drugs Aging. 2010;27:295–310.
Ahlskog JE, Muenter MD. Frequency of levodopa-related dyskinesias and motor fluctuations as estimated from the cumulative literature. Mov Disord. 2001;16:448–58.
Schrag A, Ben-Shlomo Y, Quinn N. How common are complications of Parkinson’s disease? J Neurol. 2002;249:419–23.
Fahn S. Parkinson disease, the effect of levodopa, and the ELLDOPA trial earlier vs later l-DOPA. Arch Neurol. 1999;56:529–35.
Olanow CW, Obeso JA, Stocchi F. Drug insight: continuous dopaminergic stimulation in the treatment of Parkinson’s disease. Nat Clin Pract Neurol. 2006;2:382–92.
Blanchet PJ, Grondin R, Bedard PJ, Shiosaki K, Britton DR. Dopamine D1 receptor desensitization profile in MPTP-lesioned primates. Eur J Pharmacol. 1996;309:13–20.
Olanow CW, Obeso JA, Stocchi F. Continuous dopamine-receptor treatment of Parkinson’s disease: scientific rationale and clinical implications. Lancet Neurol. 2006;5:677–87.
Keber U, Klietz M, Carlsson T, Oertel WH, Weihe E, Schafer MKH, et al. Striatal tyrosine hydroxylase-positive neurons are associated with l-DOPA-induced dyskinesia in hemiparkinsonian mice. Neurosciene. 2015;298:302–17.
Klietz M, Keber U, Carlsson T, Chiu W-H, Höglinger GU, Weihe E, et al. l-DOPA-induced dyskinesia is associated with a deficient numerical downregulation of striatal tyrosine hydroxylase mRNA-expressing neurons. Neuroscience. 2016;331:120–33.
Kadastik-Eerme L, Taba N, Asser T, Taba P. Factors associated with motor complications in Parkinson’s disease. Brain Behav. 2017;7:e00837.
Othman AA, Dutta S. Population pharmacokinetics of levodopa in subjects with advanced Parkinson’s disease: levodopa-carbidopa intestinal gel infusion vs. oral tablets. Br J Clin Pharmacol. 2014;78:94–105.
Stocchi F, Vacca L, Stirpe P, Torti M. Pharmacokinetic drug evaluation of CVT-301 for the treatment of Parkinson’s disease. Expert Opin Drug Metab Toxicol. 2018;14:1189–95.
Stampanoni Bassi M, Sancesario A, Morace R, Centonze D, Iezzi E. Cannabinoids in Parkinson’s disease. Cannabis Cannabinoid Res. 2017;2:21–9.
Weintraub D, Chiang C, Kim HM, Wilkinson J, Marras C, Stanislawski B, et al. Association of antipsychotic use with mortality risk in patients with Parkinson disease. JAMA Neurol. 2016;73:535–41.
Weintraub D, Chiang C, Kim HM, Wilkinson J, Marras C, Stanislawski B, et al. Antipsychotic use and physical morbidity in Parkinson disease. Am J Geriatr Psychiatry. 2017;25:697–705.
Divac N, Prostran M, Jakovcevski I, Cerovac N. Second-generation antipsychotics and extrapyramidal adverse effects. BioMed Res Int. 2014;2014:656370.
Fredericks D, Norton JC, Atchison C, Schoenhaus R, Pill MW. Parkinson’s disease and Parkinsons disease psychosis: a perspective on the challenges, treatments, and economic burden. Am J Manag Care. 2017;23:S83–92.
Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA. 2005;294:1934–43.
Meltzer HY, Mills R, Revell S, Williams H, Johnson A, Bahr D, et al. Pimavanserin, a serotonin(2A) receptor inverse agonist, for the treatment of Parkinson’s disease psychosis. Neuropsychopharmacology. 2010;35:881–92.
Riederer P, Laux G. MAO-inhibitors in Parkinson’s disease. Exp Neurobiol. 2011;20:1–17.
Schapira AHV. Monoamine oxidase B inhibitors for the treatment of Parkinson’s disease: a review of symptomatic and potential disease-modifying effects. CNS Drugs. 2011;25:1061–71.
Cereda E, Cilia R, Canesi M, Tesei S, Mariani CB, Zecchinelli AL, et al. Efficacy of rasagiline and selegiline in Parkinson’s disease: a head-to-head 3-year retrospective case–control study. J Neurol. 2017;264:1254–63.
Kumagai T, Nagayama H, Ota T, Nishiyama Y, Mishina M, Ueda M. Sex differences in the pharmacokinetics of levodopa in elderly patients with Parkinson disease. Clin Neuropharmacol. 2014;37:173–6.
Nagayama H, Ueda M, Kumagai T, Tsukamoto K, Nishiyama Y, Nishimura S, et al. Influence of ageing on the pharmacokinetics of levodopa in elderly patients with Parkinson’s disease. Parkinsonism Relat Disord. 2011;17:150–2.
Kanis JA, Cooper C, Rizzoli R, Reginster J-Y. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2019;30:3–44.
van den Bos F, Speelman AD, Samson M, Munneke M, Bloem BR, Verhaar HJJ. Parkinson’s disease and osteoporosis. Age Ageing. 2013;42:156–62.
Yasui K, Nakaso K, Kowa H, Takeshima T, Nakashima K. Levodopa-induced hyperhomocysteinaemia in Parkinson’s disease. Acta Neurol Scand. 2003;108:66–7.
Ganguly P, Alam SF. Role of homocysteine in the development of cardiovascular disease. Nutr J. 2015;14:6.
Szadejko K, Dziewiatowski K, Szabat K, Robowski P, Schinwelski M, Sitek E, et al. Polyneuropathy in levodopa-treated Parkinson’s patients. J Neurol Sci. 2016;371:36–41.
Loens S, Chorbadzhieva E, Kleimann A, Dressler D, Schrader C. Effects of levodopa/carbidopa intestinal gel versus oral levodopa/carbidopa on B vitamin levels and neuropathy. Brain Behav. 2017;7:e00698.
Velseboer DC, de Haan RJ, Wieling W, Goldstein DS, de Bie RMA. Prevalence of orthostatic hypotension in Parkinson’s disease: a systematic review and meta-analysis. Parkinsonism Relat Disord. 2011;17:724–9.
Ferrer-Gila T, Rizea C. Orthostatic hypotension in the elderly. Rev Neurol. 2013;56:337–43.
Jost WH, Augustis S. Severity of orthostatic hypotension in the course of Parkinson’s disease: no correlation with the duration of the disease. Parkinsonism Relat Disord. 2015;21:314–6.
Noack C, Schroeder C, Heusser K, Lipp A. Cardiovascular effects of levodopa in Parkinson’s disease. Parkinsonism Relat Disord. 2014;20:815–8.
Kondo M, Ueda Y, Makino M, Nakajima K. Worsened orthostatic hypotension due to levodopa administration in a case of Parkinson’s disease. Nihon Ronen Igakkai Zasshi. 2000;37:255–8.
Merola A, Sawyer RP, Artusi CA, Suri R, Berndt Z, Lopez-Castellanos JR, et al. Orthostatic hypotension in Parkinson disease: impact on health care utilization. Parkinsonism Relat Disord. 2018;47:45–9.
Pfeiffer RF. Gastrointestinal dysfunction in Parkinson’s disease. Curr Treat Options Neurol. 2018;20:54.
Doi H, Sakakibara R, Sato M, Masaka T, Kishi M, Tateno A, et al. Plasma levodopa peak delay and impaired gastric emptying in Parkinson’s disease. J Neurol Sci. 2012;319:86–8.
Muller T, Erdmann C, Bremen D, Schmidt WE, Muhlack S, Woitalla D, et al. Impact of gastric emptying on levodopa pharmacokinetics in Parkinson disease patients. Clin Neuropharmacol. 2006;29:61–7.
Heetun ZS, Quigley EMM. Gastroparesis and Parkinson’s disease: a systematic review. Parkinsonism Relat Disord. 2012;18:433–40.
Greene RJ, Hall AD, Hider RC. The interaction of orally administered iron with levodopa and methyldopa therapy. J Pharm Pharmacol. 1990;42:502–4.
Campbell NR, Hasinoff B. Ferrous sulfate reduces levodopa bioavailability: chelation as a possible mechanism. Clin Pharmacol Ther. 1989;45:220–5.
Deleu D, Jacob P, Chand P, Sarre S, Colwell A. Effects of caffeine on levodopa pharmacokinetics and pharmacodynamics in Parkinson disease. Neurology. 2006;67:897–9.
Robertson DR, Higginson I, Macklin BS, Renwick AG, Waller DG, George CF. The influence of protein containing meals on the pharmacokinetics of levodopa in healthy volunteers. Br J Clin Pharmacol. 1991;31:413–7.
Simon N, Gantcheva R, Bruguerolle B, Viallet F. The effects of a normal protein diet on levodopa plasma kinetics in advanced Parkinson’s disease. Parkinsonism Relat Disord. 2004;10:137–42.
Hubble JP. Long-term studies of dopamine agonists. Neurology. 2002;58:S42–50.
Jenner P. Pharmacology of dopamine agonists in the treatment of Parkinson’s disease. Neurology. 2002;58(4 Suppl. 1):S1–8.
Piercey MF. Pharmacology of pramipexole, a dopamine D3-preferring agonist useful in treating Parkinson’s disease. Clin Neuropharmacol. 1998;21:141–51.
Chen JJ, Swope DM, Dashtipour K, Lyons KE. Transdermal rotigotine: a clinically innovative dopamine-receptor agonist for the management of Parkinson’s disease. Pharmacotherapy. 2009;29:1452–67.
Tulloch IF. Pharmacologic profile of ropinirole: a nonergoline dopamine agonist. Neurology. 1997;49(1 Suppl. 1):S58–62.
Hagell P, Odin P. Apomorphine in the treatment of Parkinson’s disease. J Neurosci Nurs. 2001;33(21–34):37–8.
Stacy M, Silver D. Apomorphine for the acute treatment of “off” episodes in Parkinson’s disease. Parkinsonism Relat Disord. 2008;14:85–92.
Kulisevsky J, Pagonabarraga J. Tolerability and safety of ropinirole versus other dopamine agonists and levodopa in the treatment of Parkinson’s disease: meta-analysis of randomized controlled trials. Drug Saf. 2010;33:147–61.
Voon V, Hassan K, Zurowski M, Duff-Canning S, de Souza M, Fox S, et al. Prospective prevalence of pathologic gambling and medication association in Parkinson disease. Neurology. 2006;66:1750–2.
Voon V, Hassan K, Zurowski M, de Souza M, Thomsen T, Fox S, et al. Prevalence of repetitive and reward-seeking behaviors in Parkinson disease. Neurology. 2006;67:1254–7.
Weintraub D, Siderowf AD, Potenza MN, Goveas J, Morales KH, Duda JE, et al. Association of dopamine agonist use with impulse control disorders in Parkinson disease. Arch Neurol. 2006;63:969–73.
Bienfait KL, Menza M, Mark MH, Dobkin RD. Impulsive smoking in a patient with Parkinson’s disease treated with dopamine agonists. J Clin Neurosci. 2010;17:539–40.
Ceravolo R, Frosini D, Rossi C, Bonuccelli U. Impulse control disorders in Parkinson’s disease: definition, epidemiology, risk factors, neurobiology and management. Parkinsonism Relat Disord. 2009;15(Suppl. 4):S111–5.
Miyasaki JM. Evidence-based initiation of dopaminergic therapy in Parkinson’s disease. J Neurol. 2010;257(Suppl. 2):S309–13.
Antonini A, Chaudhuri KR, Boroojerdi B, Asgharnejad M, Bauer L, Grieger F, et al. Impulse control disorder related behaviours during long-term rotigotine treatment: a post hoc analysis. Eur J Neurol. 2016;23:1556–65.
Moller JC, Eggert KM, Unger M, Odin P, Chaudhuri KR, Oertel WH. Clinical risk-benefit assessment of dopamine agonists. Eur J Neurol. 2008;15(Suppl. 2):15–23.
Paus S, Brecht HM, Koster J, Seeger G, Klockgether T, Wullner U. Sleep attacks, daytime sleepiness, and dopamine agonists in Parkinson’s disease. Mov Disord. 2003;18:659–67.
Etminan M, Gill S, Samii A. Comparison of the risk of adverse events with pramipexole and ropinirole in patients with Parkinson’s disease: a meta-analysis. Drug Saf. 2003;26:439–44.
Abbott RD, Petrovitch H, White LR, Masaki KH, Tanner CM, Curb JD, et al. Frequency of bowel movements and the future risk of Parkinson’s disease. Neurology. 2001;57:456–62.
Gao X, Chen H, Schwarzschild MA, Ascherio A. A prospective study of bowel movement frequency and risk of Parkinson’s disease. Am J Epidemiol. 2011;174:546–51.
Zhou C-Q, Zhang J-W, Wang M, Peng G-G. Meta-analysis of the efficacy and safety of long-acting non-ergot dopamine agonists in Parkinson’s disease. J Clin Neurosci. 2014;21:1094–101.
Tan EK, Jankovic J. Choosing dopamine agonists in Parkinson’s disease. Clin Neuropharmacol. 2001;24:247–53.
Chaudhuri KR, Pal S, Brefel-Courbon C. ‘Sleep attacks’ or “unintended sleep episodes” occur with dopamine agonists: is this a class effect? Drug Saf. 2002;25:473–83.
Razmy A, Lang AE, Shapiro CM. Predictors of impaired daytime sleep and wakefulness in patients with Parkinson disease treated with older (ergot) vs newer (nonergot) dopamine agonists. Arch. Neurol. 2004;61:97–102.
Sprenger FS, Seppi K, Poewe W. Drug safety evaluation of rotigotine. Expert Opin Drug Saf. 2012;11:503–12.
Ishiguro N, Saito A, Yokoyama K, Morikawa M, Igarashi T, Tamai I. Transport of the dopamine D2 agonist pramipexole by rat organic cation transporters OCT1 and OCT2 in kidney. Drug Metab Dispos. 2005;33:495–9.
Knop J, Hoier E, Ebner T, Fromm MF, Muller F. Renal tubular secretion of pramipexole. Eur J Pharm Sci. 2015;79:73–8.
Wu MJ, Ing TS, Soung LS, Daugirdas JT, Hano JE, Gandhi VC. Amantadine hydrochloride pharmacokinetics in patients with impaired renal function. Clin Nephrol. 1982;17:19–23.
Kaye CM, Nicholls B. Clinical pharmacokinetics of ropinirole. Clin Pharmacokinet. 2000;39:243–54.
Bloomer JC, Clarke SE, Chenery RJ. In vitro identification of the P450 enzymes responsible for the metabolism of ropinirole. Drug Metab Dispos. 1997;25:840–4.
Girndt M, Trocchi P, Scheidt-Nave C, Markau S, Stang A. The prevalence of renal failure: results from the German Health Interview and Examination Survey for Adults, 2008–2011 (DEGS1). Dtsch Arztebl Int. 2016;113:85–91.
Schaeffner ES, Ebert N, Delanaye P, Frei U, Gaedeke J, Jakob O, et al. Two novel equations to estimate kidney function in persons aged 70 years or older. Ann Intern Med. 2012;157:471–81.
Pellecchia MT, Vitale C, Sabatini M, Longo K, Amboni M, Bonavita V, et al. Ropinirole as a treatment of restless legs syndrome in patients on chronic hemodialysis: an open randomized crossover trial versus levodopa sustained release. Clin Neuropharmacol. 2004;27:178–81.
Cawello W, Ahrweiler S, Sulowicz W, Szymczakiewicz-Multanowska A, Braun M. Single dose pharmacokinetics of the transdermal rotigotine patch in patients with impaired renal function. Br J Clin Pharmacol. 2012;73:46–54.
Cieslak KP, Baur O, Verheij J, Bennink RJ, van Gulik TM. Liver function declines with increased age. HPB (Oxford). 2016;18:691–6.
Cawello W, Fichtner A, Boekens H, Braun M. Influence of hepatic impairment on the pharmacokinetics of the dopamine agonist rotigotine. Eur J Drug Metab Pharmacokinet. 2014;39:155–63.
Navacerrada F, Gonzalez-Alonso MR, Alonso-Navarro H, Pilo-de-la-Fuente B, Plaza-Nieto JF, Jimenez-Jimenez FJ. Liver toxicity possibly related with ropinirole use in the treatment of restless legs syndrome. Eur J Neurol. 2011;18:e65.
Dewey RBJ, Hutton JT, LeWitt PA, Factor SA. A randomized, double-blind, placebo-controlled trial of subcutaneously injected apomorphine for parkinsonian off-state events. Arch Neurol. 2001;58:1385–92.
Stibe CM, Lees AJ, Kempster PA, Stern GM. Subcutaneous apomorphine in parkinsonian on-off oscillations. Lancet. 1988;1:403–6.
Humphrey SJ, Turman CN, Curry JT, Wheeler GJ. Cardiovascular and electrocardiographic effects of the dopamine receptor agonists ropinirole, apomorphine, and PNU-142774E in conscious beagle dogs. J Cardiovasc Pharmacol. 2006;47:337–47.
Stocchi F, De Pandis MF, Delfino FA, Anselmo T, Frongillo D. Transient atrial fibrillation after subcutaneous apomorphine bolus. Mov Disord. 1996;11:584–5.
Kaminioti AN, Nikitas GT, Terlis AK, Manolis AG, Thomaides T, Panousopoulou AN. Ventricular bigeminy after subcutaneous administration of apomorphine in a patient with refractory Parkinson’s disease: a case report. J Mov Disord. 2013;6:9–12.
Sartori M, Pratt CM, Young JB. Torsade de Pointe. Malignant cardiac arrhythmia induced by amantadine poisoning. Am J Med. 1984;77:388–91.
Schwartz M, Patel M, Kazzi Z, Morgan B. Cardiotoxicity after massive amantadine overdose. J Med Toxicol. 2008;4:173–9.
De Ponti F, Poluzzi E, Cavalli A, Recanatini M, Montanaro N. Safety of non-antiarrhythmic drugs that prolong the QT interval or induce torsade de pointes: an overview. Drug Saf. 2002;25:263–86.
Watanabe Y, Nakamura Y, Cao X, Ohara H, Yamazaki Y, Murayama N, et al. Intravenous administration of apomorphine does NOT induce long QT syndrome: experimental evidence from in vivo canine models. Basic Clin Pharmacol Toxicol. 2015;116:468–75.
Halvorsen KA, Martensen-Larsen O. Apomorphine revived: fortified, prolonged, and improved therapeutical effect. Int J Addict. 1978;13:475–84.
Auffret M, Drapier S, Verin M. The many faces of apomorphine: lessons from the past and challenges for the future. Drugs R D. 2018;18:91–107.
Rausten DS, Ochs MA. Apomorphine-naloxone controlled rapid emesis. J Am Coll Emerg Phys. 1973;2:44–5.
Björklund A, Dunnett SB. Dopamine neuron systems in the brain: an update. Trends Neurosci. 2007;30:194–202.
Muller T. Catechol-O-methyltransferase inhibitors in Parkinson’s disease. Drugs. 2015;75:157–74.
Axelrod J, Tomchick R. Enzymatic O-methylation of epinephrine and other catechols. J Biol Chem. 1958;233:702–5.
Guldberg HC, Marsden CA. Catechol-O-methyl transferase: pharmacological aspects and physiological role. Pharmacol Rev. 1975;27:135–206.
Napolitano A, Del Dotto P, Petrozzi L, Dell’Agnello G, Bellini G, Gambaccini G, et al. Pharmacokinetics and pharmacodynamics of l-Dopa after acute and 6-week tolcapone administration in patients with Parkinson’s disease. Clin Neuropharmacol. 1999;22:24–9.
Ruottinen HM, Rinne UK. A double-blind pharmacokinetic and clinical dose-response study of entacapone as an adjuvant to levodopa therapy in advanced Parkinson’s disease. Clin Neuropharmacol. 1996;19:283–96.
Ferreira JJ, Lees A, Rocha J-F, Poewe W, Rascol O, Soares-da-Silva P. Opicapone as an adjunct to levodopa in patients with Parkinson’s disease and end-of-dose motor fluctuations: a randomised, double-blind, controlled trial. Lancet Neurol. 2016;15:154–65.
Factor SA, Molho ES, Feustel PJ, Brown DL, Evans SM. Long-term comparative experience with tolcapone and entacapone in advanced Parkinson’s disease. Clin Neuropharmacol. 2001;24:295–9.
Rocha J-F, Almeida L, Falcao A, Palma PN, Loureiro AI, Pinto R, et al. Opicapone: a short lived and very long acting novel catechol-O-methyltransferase inhibitor following multiple dose administration in healthy subjects. Br J Clin Pharmacol. 2013;76:763–75.
Davis TL, Roznoski M, Burns RS. Effects of tolcapone in Parkinson’s patients taking l-dihydroxyphenylalanine/carbidopa and selegiline. Mov Disord. 1995;10:349–51.
Kuoppamaki M, Leinonen M, Poewe W. Efficacy and safety of entacapone in levodopa/carbidopa versus levodopa/benserazide treated Parkinson’s disease patients with wearing-off. J Neural Transm (Vienna). 2015;122:1709–14.
Rodrigues FB, Ferreira JJ. Opicapone for the treatment of Parkinson’s disease. Expert Opin Pharmacother. 2017;18:445–53.
Antonini A, Abbruzzese G, Barone P, Bonuccelli U, Lopiano L, Onofrj M, et al. COMT inhibition with tolcapone in the treatment algorithm of patients with Parkinson’s disease (PD): relevance for motor and non-motor features. Neuropsychiatr Dis Treat. 2008;4:1–9.
Suchowersky O, Bailey P, Pourcher E, Bulger L, Facciponte G. Comparison of two dosages of tolcapone added to levodopa in nonfluctuating patients with PD. Clin Neuropharmacol. 2001;24:214–20.
Olanow CW, Watkins PB. Tolcapone: an efficacy and safety review (2007). Clin Neuropharmacol. 2007;30:287–94.
Lees AJ, Ratziu V, Tolosa E, Oertel WH. Safety and tolerability of adjunctive tolcapone treatment in patients with early Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2007;78:944–8.
Unger MM, Reese JP, Oertel WH, Eggert KM. Real-life evaluations of compliance with mandatory drug safety monitoring exemplified with tolcapone in Parkinson’s disease. Eur Neurol. 2008;60:122–6.
Heranval A, Lefaucheur R, Fetter D, Rouille A, Le Goff F, Maltete D. Drugs with potential cardiac adverse effects: retrospective study in a large cohort of parkinsonian patients. Rev Neurol (Paris). 2016;172:318–23.
Van Booven D, Marsh S, McLeod H, Carrillo MW, Sangkuhl K, Klein TE, et al. Cytochrome P450 2C9-CYP2C9. Pharmacogenet Genomics. 2010;20:277–81.
Dingemanse J, Meyerhoff C, Schadrack J. Effect of the catechol-O-methyltransferase inhibitor entacapone on the steady-state pharmacokinetics and pharmacodynamics of warfarin. Br J Clin Pharmacol. 2002;53:485–91.
European Medicines Agency. Ongentys: EMA assessment report. London, UK: European Medicines Agency; 2016. p. 1–140.
Shitara Y, Maeda K, Ikejiri K, Yoshida K, Horie T, Sugiyama Y. Clinical significance of organic anion transporting polypeptides (OATPs) in drug disposition: their roles in hepatic clearance and intestinal absorption. Biopharm Drug Dispos. 2013;34:45–78.
Yu J, Zhou Z, Tay-Sontheimer J, Levy RH, Ragueneau-Majlessi I. Intestinal drug interactions mediated by OATPs: a systematic review of preclinical and clinical findings. J Pharm Sci. 2017;106:2312–25.
Kalgutkar AS, Dalvie DK, Castagnoli NJ, Taylor TJ. Interactions of nitrogen-containing xenobiotics with monoamine oxidase (MAO) isozymes A and B: SAR studies on MAO substrates and inhibitors. Chem Res Toxicol. 2001;14:1139–62.
Fernandez HH, Chen JJ. Monoamine oxidase-B inhibition in the treatment of Parkinson’s disease. Pharmacotherapy. 2007;27:174S–85S.
Chang Y, Wang L-B, Li D, Lei K, Liu S-Y. Efficacy of rasagiline for the treatment of Parkinson’s disease: an updated meta-analysis. Ann Med. 2017;49:421–34.
Dashtipour K, Chen JJ, Kani C, Bahjri K, Ghamsary M. Clinical outcomes in patients with Parkinson’s disease treated with a monoamine oxidase type-B inhibitor: a cross-sectional, cohort study. Pharmacotherapy. 2015;35:681–6.
Dezsi L, Vecsei L. Monoamine oxidase B inhibitors in Parkinson’s disease. CNS Neurol Disord Drug Targets. 2017;16:425–39.
Riederer P, Lachenmayer L. Selegiline’s neuroprotective capacity revisited. J Neural Transm (Vienna). 2003;110:1273–8.
Olanow CW, Rascol O, Hauser R, Feigin PD, Jankovic J, Lang A, et al. A double-blind, delayed-start trial of rasagiline in Parkinson’s disease. N Engl J Med. 2009;361:1268–78.
Sadeghian M, Mullali G, Pocock JM, Piers T, Roach A, Smith KJ. Neuroprotection by safinamide in the 6-hydroxydopamine model of Parkinson’s disease. Neuropathol Appl Neurobiol. 2016;42:423–35.
Hauser RA, Abler V, Eyal E, Eliaz RE. Efficacy of rasagiline in early Parkinson’s disease: a meta-analysis of data from the TEMPO and ADAGIO studies. Int J Neurosci. 2016;126:942–6.
Jenner P, Langston JW. Explaining ADAGIO: a critical review of the biological basis for the clinical effects of rasagiline. Mov Disord. 2011;26:2316–23.
Romberg RW, Needleman SB, Snyder JJ, Greedan A. Methamphetamine and amphetamine derived from the metabolism of selegiline. J Forensic Sci. 1995;40:1100–2.
Stocchi F, Torti M. Adjuvant therapies for Parkinson’s disease: critical evaluation of safinamide. Drug Des Dev Ther. 2016;10:609–18.
Parkinson Study Group. A controlled trial of rasagiline in early Parkinson disease: the TEMPO Study. Arch Neurol. 2002;59:1937–43.
Elmer L, Schwid S, Eberly S, Goetz C, Fahn S, Kieburtz K, et al. Rasagiline-associated motor improvement in PD occurs without worsening of cognitive and behavioral symptoms. J Neurol Sci. 2006;248:78–83.
Parkinson Study Group. Effects of tocopherol and deprenyl on the progression of disability in early Parkinson’s disease. N Engl J Med. 1993;328:176–83.
Hauser RA, Silver D, Choudhry A, Eyal E, Isaacson S. Randomized, controlled trial of rasagiline as an add-on to dopamine agonists in Parkinson’s disease. Mov Disord. 2014;29:1028–34.
Richard IH, Kurlan R, Tanner C, Factor S, Hubble J, Suchowersky O, et al. Serotonin syndrome and the combined use of deprenyl and an antidepressant in Parkinson’s disease in Parkinson Study Group. Neurology. 1997;48:1070–7.
Panisset M, Chen JJ, Rhyee SH, Conner J, Mathena J. Serotonin toxicity association with concomitant antidepressants and rasagiline treatment: retrospective study (STACCATO). Pharmacotherapy. 2014;34:1250–8.
Aboukarr A, Giudice M. Interaction between monoamine oxidase B inhibitors and selective serotonin reuptake inhibitors. Can J Hosp Pharm. 2018;71:196–207.
Taylor JJ, Wilson JW, Estes LL. Linezolid and serotonergic drug interactions: a retrospective survey. Clin Infect Dis. 2006;43:180–7.
Chen JJ, Swope DM. Clinical pharmacology of rasagiline: a novel, second-generation propargylamine for the treatment of Parkinson disease. J Clin Pharmacol. 2005;45:878–94.
Churchyard A, Mathias CJ, Boonkongchuen P, Lees AJ. Autonomic effects of selegiline: possible cardiovascular toxicity in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 1997;63:228–34.
Laine K, Anttila M, Helminen A, Karnani H, Huupponen R. Dose linearity study of selegiline pharmacokinetics after oral administration: evidence for strong drug interaction with female sex steroids. Br J Clin Pharmacol. 1999;47:249–54.
Palovaara S, Anttila M, Nyman L, Laine K. Effect of concomitant hormone replacement therapy containing estradiol and levonorgestrel on the pharmacokinetics of selegiline. Eur J Clin Pharmacol. 2002;58:259–63.
Cruz MP. Xadago (Safinamide): a monoamine oxidase B inhibitor for the adjunct treatment of motor symptoms in Parkinson’s disease. P T. 2017;42:622–37.
Finberg JPM. Pharmacology of rasagiline, a new MAO-B inhibitor drug for the treatment of Parkinson’s disease with neuroprotective potential. Rambam Maimonides Med J. 2010;1:e0003.
Chen JJ, Wilkinson JR. The monoamine oxidase type B inhibitor rasagiline in the treatment of Parkinson disease: is tyramine a challenge? J Clin Pharmacol. 2012;52:620–8.
Marquet A, Kupas K, Johne A, Astruc B, Patat A, Krosser S, et al. The effect of safinamide, a novel drug for Parkinson’s disease, on pressor response to oral tyramine: a randomized, double-blind, clinical trial. Clin Pharmacol Ther. 2012;92:450–7.
Anttila M, Sotaniemi EA, Pelkonen O, Rautio A. Marked effect of liver and kidney function on the pharmacokinetics of selegiline. Clin Pharmacol Ther. 2005;77:54–62.
Rudolph JL, Salow MJ, Angelini MC, McGlinchey RE. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med. 2008;168:508–13.
Aizenberg D, Sigler M, Weizman A, Barak Y. Anticholinergic burden and the risk of falls among elderly psychiatric inpatients: a 4-year case–control study. Int Psychogeriatr. 2002;14:307–10.
Ehrt U, Broich K, Larsen JP, Ballard C, Aarsland D. Use of drugs with anticholinergic effect and impact on cognition in Parkinson’s disease: a cohort study. J Neurol Neurosurg Psychiatry. 2010;81:160–5.
Crispo JAG, Willis AW, Thibault DP, Fortin Y, Hays HD, McNair DS, et al. Associations between anticholinergic burden and adverse health outcomes in Parkinson disease. PLoS One. 2016;11:e0150621.
Vezina P, Mohr E, Grimes D. Deprenyl in Parkinson’s disease: mechanisms, neuroprotective effect, indications and adverse effects. Can J Neurol Sci. 1992;19:142–6.
Glavin GB, Dugani AM, Pinsky C. L-deprenyl attenuates stress ulcer formation in rats. Neurosci Lett. 1986;70:379–81.
Geyer M, Stamenic I, Buhler H, Bertschinger P. Epidemiology of gastrointestinal bleeding in the elderly. Praxis (Bern 1994). 2006;95:757–65.
Kyaw MH, Chan FKL. Pharmacologic options in the management of upper gastrointestinal bleeding: focus on the elderly. Drugs Aging. 2014;31:349–61.
Moriyoshi K, Masu M, Ishii T, Shigemoto R, Mizuno N, Nakanishi S. Molecular cloning and characterization of the rat NMDA receptor. Nature. 1991;354:31–7.
Faulkner MA. Safety overview of FDA-approved medications for the treatment of the motor symptoms ofParkinson's disease. Expert Opin Drug Saf. 2014;13(8):1055–69. https://doi.org/10.1517/14740338.2014.931369.
Hubsher G, Haider M, Okun MS. Amantadine: the journey from fighting flu to treating Parkinson disease. Neurology. 2012;78:1096–9.
Schwab RS, England ACJ, Poskanzer DC, Young RR. Amantadine in the treatment of Parkinson’s disease. JAMA. 1969;208:1168–70.
Mizoguchi K, Yokoo H, Yoshida M, Tanaka T, Tanaka M. Amantadine increases the extracellular dopamine levels in the striatum by re-uptake inhibition and by N-methyl-d-aspartate antagonism. Brain Res. 1994;662:255–8.
Pahwa R, Tanner CM, Hauser RA, Isaacson SH, Nausieda PA, Truong DD, et al. ADS-5102 (amantadine) extended-release capsules for levodopa-induced dyskinesia in Parkinson disease (EASE LID Study): a randomized clinical trial. JAMA Neurol. 2017;74:941–9.
Oertel W, Eggert K, Pahwa R, Tanner CM, Hauser RA, Trenkwalder C, et al. Randomized, placebo-controlled trial of ADS-5102 (amantadine) extended-release capsules for levodopa-induced dyskinesia in Parkinson’s disease (EASE LID 3). Mov Disord. 2017;32:1701–9.
Hiraoka M, Hirano Y, Kawano S, Fan Z, Sawanobori T. Amantadine-induced afterpotentials and automaticity in guinea pig ventricular myocytes. Circ Res. 1989;65:880–93.
Manini AF, Raspberry D, Hoffman RS, Nelson LS. QT prolongation and torsades de pointes following overdose of ziprasidone and amantadine. J Med Toxicol. 2007;3:178–81.
Wilson TW, Rajput AH. Amantadine-dyazide interaction. Can Med Assoc J. 1983;129:974–5.
Akturk IF, Erol MK. Bradyarrhythmias and pacemaker indications in elderly patients. Turk Kardiyol Dern Ars. 2017;45:71–4.
Dandamudi S, Slusser J, Mahoney DW, Redfield MM, Rodeheffer RJ, Chen HH. The prevalence of diabetic cardiomyopathy: a population-based study in Olmsted County, Minnesota. J Card Fail. 2014;20:304–9.
Nakata M, Ito S, Shirai W, Hattori T. Severe reversible neurological complications following amantadine treatment in three elderly patients with renal insufficiency. Eur Neurol. 2006;56:59–61.
Bleidner WE, Harmon JB, Hewes WE, Lynes TE, Hermann EC. Absorption, distribution and excretion of amantadine hydrochloride. J Pharmacol Exp Ther. 1965;150:484–90.
Ing TS, Rahn AC, Armbruster KF, Oyama JH, Klawans HL. Letter: accumulation of amantadine hydrochloride in renal insufficiency. N Engl J Med. 1974;291:1257.
Stoof JC, Booij J, Drukarch B, Wolters EC. The anti-parkinsonian drug amantadine inhibits the N-methyl-d-aspartic acid-evoked release of acetylcholine from rat neostriatum in a non-competitive way. Eur J Pharmacol. 1992;213:439–43.
Lupp A, Lucking CH, Koch R, Jackisch R, Feuerstein TJ. Inhibitory effects of the antiparkinsonian drugs memantine and amantadine on N-methyl-d-aspartate-evoked acetylcholine release in the rabbit caudate nucleus in vitro. J Pharmacol Exp Ther. 1992;263:717–24.
Oh ES, Fong TG, Hshieh TT, Inouye SK. Delirium in older persons: advances in diagnosis and treatment. JAMA. 2017;318:1161–74.
Neagoe AD. Delirium with manic and psychotic features associated with amantadine. Gen Hosp Psychiatry. 2013;35(680):e7–8.
Postma JU, Van Tilburg W. Visual hallucinations and delirium during treatment with amantadine (Symmetrel). J Am Geriatr Soc. 1975;23:212–5.
Flaherty JA, Bellur SN. Mental side effects of amantadine therapy: its spectrum and characteristics in a normal population. J Clin Psychiatry. 1981;42:344–5.
Scott JL, Walls RM. QT interval prolongation. J Emerg Med. 1985;3:221–5.
Moreno O, Garcia PT, Sanchez D, Sancho T, Lecumberri B. Cognitive impairment and severe hypocalcemia in a patient with hypoparathyroidism and systemic sclerosis: report of a case. Endocrinol Nutr. 2015;62:356–8.
Fujioka S, Fukae J, Ogura H, Mishima T, Yanamoto S, Higuchi M-A, et al. Hospital-based study on emergency admission of patients with Parkinson’s disease. eNeurologicalSci. 2016;4:19–21.
Guneysel O, Onultan O, Onur O. Parkinson’s disease and the frequent reasons for emergency admission. Neuropsychiatr Dis Treat. 2008;4:711–4.
Braga M, Pederzoli M, Antonini A, Beretta F, Crespi V. Reasons for hospitalization in Parkinson’s disease: a case–control study. Parkinsonism Relat Disord. 2014;20:488–92.
Begg DP. Disturbances of thirst and fluid balance associated with aging. Physiol Behav. 2017;178:28–34.
Hindle JV. The practical management of cognitive impairment and psychosis in the older Parkinson’s disease patient. J Neural Transm (Vienna). 2013;120:649–53.
Parkers JD, Marsden CD, Price P. Amantadine-induced heart-failure. Lancet. 1977;1:904.
Mokhles MM, Trifiro G, Dieleman JP, Haag MD, van Soest EM, Verhamme KMC, et al. The risk of new onset heart failure associated with dopamine agonist use in Parkinson’s disease. Pharmacol Res. 2012;65:358–64.
Hasenfuss G, Kasper W, Meinertz T, Busch W, Lehmann M, Krause T, et al. Evaluation of long-term oral levodopa therapy in chronic congestive heart failure. Klin Wochenschr. 1987;65:1087–94.
Montastruc JL, Rascol O, Montastruc P. Naloxone or haloperidol but not yohimbine reverse apomorphine-induced respiratory depression. Clin Neuropharmacol. 1992;15:404–7.
Srinivasan M, Lagercrantz H, Yamamoto Y. A possible dopaminergic pathway mediating hypoxic depression in neonatal rabbits. J Appl Physiol. 1985;1989(67):1271–6.
Gibbons CH, Simon DK, Huang M, Tilley B, Aminoff MJ, Bainbridge JL, et al. Autonomic and electrocardiographic findings in Parkinson’s disease. Auton Neurosci. 2017;205:93–8.
Kannankeril PJ, Roden DM. Drug-induced long QT and torsade de pointes: recent advances. Curr Opin Cardiol. 2007;22:39–43.
Roden DM. Predicting drug-induced QT prolongation and torsades de pointes. J Physiol. 2016;594:2459–68.
Jahn K, Kressig RW, Bridenbaugh SA, Brandt T, Schniepp R. Dizziness and unstable gait in old age: etiology, diagnosis and treatment. Dtsch Arztebl Int. 2015;112:387–93.
Hanewinckel R, van Oijen M, Ikram MA, van Doorn PA. The epidemiology and risk factors of chronic polyneuropathy. Eur J Epidemiol. 2016;31:5–20.
Nyholm D, Nilsson Remahl AIM, Dizdar N, Constantinescu R, Holmberg B, Jansson R, et al. Duodenal levodopa infusion monotherapy vs oral polypharmacy in advanced Parkinson disease. Neurology. 2005;64:216–23.
Swanson PD. Drug treatment of Parkinson’s disease: is ‘polypharmacy’ best? J. Neurol Neurosurg Psychiatry. 1994;57:401–3.
Krause O, Wiese B, Doyle I-M, Kirsch C, Thürmann P, Wilm S, et al. Multidisciplinary intervention to improve medication safety in nursing home residents: protocol of a cluster randomised controlled trial (HIOPP-3-iTBX study). BMC Geriatr. 2019;19:24.
Lange R, Erbguth F. Parkinson’s disease in the elderly. Z Gerontol Geriatr. 2017;50:547–59.
Yildirim AB, Kilinc AY. Polypharmacy and drug interactions in elderly patients. Turk Kardiyol Dern Ars. 2017;45:17–21.
Moriarty F, Hardy C, Bennett K, Smith SM, Fahey T. Trends and interaction of polypharmacy and potentially inappropriate prescribing in primary care over 15 years in Ireland: a repeated cross-sectional study. BMJ Open. 2015;5:e008656.
Muhic N, Mrhar A, Brvar M. Comparative analysis of three drug–drug interaction screening systems against probable clinically relevant drug–drug interactions: a prospective cohort study. Eur J Clin Pharmacol. 2017;73:875–82.
Somogyi-Vegh A, Nyaka B, Vida RG, Lovasz A, Botz L. Comprehensive evaluation of drug interaction screening programs: discrepancies and concordances. Orv Hetil. 2015;156:720–30.
Kheshti R, Aalipour M, Namazi S. A comparison of five common drug–drug interaction software programs regarding accuracy and comprehensiveness. J Res Pharm Pract. 2016;5:257–63.
Moura CS, Prado NM, Belo NO, Acurcio FA. Evaluation of drug–drug interaction screening software combined with pharmacist intervention. Int J Clin Pharm. 2012;34:547–52.
Pazan F, Weiss C, Wehling M. The FORTA (Fit fOR The Aged) List 2015: update of a validated clinical tool for improved pharmacotherapy in the elderly. Drugs Aging. 2016;33:447–9.
Kuhn-Thiel AM, Weiss C, Wehling M. Consensus validation of the FORTA (Fit fOR The Aged) List: a clinical tool for increasing the appropriateness of pharmacotherapy in the elderly. Drugs Aging. 2014;31:131–40.
Brown JD, Hutchison LC, Li C, Painter JT, Martin BC. Predictive validity of the Beers and Screening Tool of Older Persons’ Potentially Inappropriate Prescriptions (STOPP) criteria to detect adverse drug events, hospitalizations, and emergency department visits in the United States. J Am Geriatr Soc. 2016;64:22–30.
Hamilton H, Gallagher P, Ryan C, Byrne S, O’Mahony D. Potentially inappropriate medications defined by STOPP criteria and the risk of adverse drug events in older hospitalized patients. Arch Intern Med. 2011;171:1013–9.
Siebert S, Elkeles B, Hempel G, Kruse J, Smollich M. The PRISCUS list in clinical routine: practicability and comparison to international PIM lists. Z Gerontol Geriatr. 2013;46:35–47.
Cooper JA, Cadogan CA, Patterson SM, Kerse N, Bradley MC, Ryan C, et al. Interventions to improve the appropriate use of polypharmacy in older people: a Cochrane systematic review. BMJ Open. 2015;5:e009235.
Kim J, Parish AL. Polypharmacy and medication management in older adults. Nurs Clin North Am. 2017;52:457–68.
O’Mahony D, O’Ullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44:213–8.
Salbu RL, Feuer J. A closer look at the 2015 Beers criteria. J Pharm Pract. 2017;30:419–24.
Antimisiaris D, Cutler T. Managing polypharmacy in the 15-minute office visit. Prim Care. 2017;44:413–28.
Jansen J, Naganathan V, Carter SM, McLachlan AJ, Nickel B, Irwig L, et al. Too much medicine in older people? Deprescribing through shared decision making. BMJ. 2016;353:i2893.
Scott IA, Hilmer SN, Reeve E, Potter K, Le Couteur D, Rigby D, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175:827–34.
Loffler C, Drewelow E, Paschka SD, Frankenstein M, Eger J, Jatsch L, et al. Optimizing polypharmacy among elderly hospital patients with chronic diseases: study protocol of the cluster randomized controlled POLITE-RCT trial. Implement Sci. 2014;9:151.
Acknowledgements
The authors thank the many collaborators and patients for vital and challenging discussions on the pharmacotherapy of Parkinson’s disease.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were received for the preparation of this article.
Conflict of interest
Martin Klietz, Stephan Greten, Florian Wegner, and Günter U. Höglinger have no conflicts of interest that are directly relevant to the content of this article.
Rights and permissions
About this article
Cite this article
Klietz, M., Greten, S., Wegner, F. et al. Safety and Tolerability of Pharmacotherapies for Parkinson’s Disease in Geriatric Patients. Drugs Aging 36, 511–530 (2019). https://doi.org/10.1007/s40266-019-00654-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-019-00654-z