Abstract
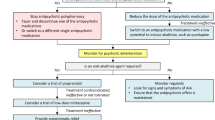
Akathisia is one of the most prevalent and distressing adverse effects associated with antipsychotic drug treatment. Propranolol, a non-selective beta-adrenergic receptor antagonist, is currently considered a first-line treatment for antipsychotic-induced akathisia (AIA). Surprisingly, the evidence for its anti-akathisia effect is modest. Propranolol’s side effects (e.g. orthostatic hypotension, bradycardia), contraindications (e.g. asthma) and increased complexity in titration schedules limit its use in some patients. Anticholinergic agents and benzodiazepines merely provide symptomatic relief in patients with AIA. Effective and well-tolerated treatment remains a major unmet need in akathisia and warrants a search for new anti-akathisia agents. Accumulating evidence during the last two decades indicates that agents with marked postsynaptic serotonin 5-HT2a receptor antagonism (ritanserin, cyproheptadine, trazodone, mianserin, mirtazapine) may represent a new class of potential anti-akathisia remedies. Among these agents, low-dose mirtazapine (7.5 mg or 15 mg once daily) has demonstrated the most compelling evidence for therapeutic efficacy. In this narrative review we highlight the clinical significance of AIA, outline major approaches for its management and propose a practical algorithm for its treatment.

Similar content being viewed by others
References
Kane JM, Fleischhacker WW, Hansen L, Perlis R, Pikalov A 3rd, Assunção-Talbott S. Akathisia: an updated review focusing on second-generation antipsychotics. J Clin Psychiatry. 2009;70:627–43.
Poyurovsky M, Weizman A. Serotonin-based pharmacotherapy for acute neuroleptic-induced akathisia: a new approach to an old problem. Br J Psychiatry. 2001;179:4–8.
Lohr JB, Eidt CA, Abdulrazzaq Alfaraj A, Soliman MA. The clinical challenges of akathisia. CNS Spectr. 2015;20(Suppl 1):1–14.
Salem H, Nagpal C, Pigott T, Teixeira AL. Revisiting antipsychotic-induced akathisia: current issues and prospective challenges. Curr Neuropharmacol. 2017;15:789–98.
Barnes TR, Braude WM. Akathisia variants and tardive dyskinesia. Arch Gen Psychiatry. 1985;42(9):874–8.
Weiden PJ, Mann JJ, Haas GL, et al. Clinical non-recognition of antipsychotic-induced movement disorders: a cautionary study. Am J Psychiatry. 1987;144:1148–53.
Tachere RO, Modirrousta M. Beyond anxiety and agitation: a clinical approach to akathisia. Aust Fam Phys. 2017;46:296–8.
Correll CU. Assessing and maximizing the safety and tolerability of antipsychotics used in the treatment of children and adolescents. J Clin Psychiatry. 2008;69(suppl 4):26–36.
Musco S, Ruekert L, Myers J, Anderson D, Welling M, Cunningham EA. Characteristics of patients experiencing extrapyramidal symptoms or other movement disorders related to dopamine receptor blocking agent therapy. J Clin Psychopharmacol. 2019;39:336–43.
Stegmayer K, Walther S, van Harten P. Tardive dyskinesia associated with atypical antipsychotics: prevalence, mechanism and management strategies. CNS Drugs. 2018;32:135–47.
Savitt D, Jankovic J. Tardive syndromes. J Neurol Sci. 2018;389:35–42.
Kurlawala Z, Vatsalya V. Heavy alcohol drinking associated akathisia and management with quetiapine XR in alcohol dependent patients. J Addict. 2016. https://doi.org/10.1155/2016/6028971.
Gattera, et al. A retrospective study of risk factors of akathisia in terminally ill patients. J Pain Symptom Manag. 1994;9:454–61.
Hansen L. A critical review of akathisia, and its possible association with suicidal behaviour. Hum Psychopharmacol. 2001;16:495–505.
Poyurovsky M, Weizman A. Treatment of antipsychotic-related akathisia revisited: the role of serotonin 2A receptor antagonists. J Clin Psychopharmacol. 2015;35(6):711–4.
Berna F, Misdrahi D, Boyer L, Aouizerate B, Brunel L, Capdevielle D, FACE-SZ (Fonda Mental Academic Centers of Expertise for Schizophrenia) group, et al. Akathisia: prevalence and risk factors in a community-dwelling sample of patients with schizophrenia. Results from the FACE-SZ dataset. Schizophr Res. 2015;169:255–61.
Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, Keefe RS, Davis SM, Davis CE, Lebowitz BD, Severe J, Hsiao JK, Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353:1209–23.
Barnes TR. The Barnes Akathisia Rating Scale revisited. J Psychopharmacol. 2003;17:365–70.
Miller D, Caroff SN, Davis SM, Rosenheck RA, McEvoy JP, Saltz BL, Riggio S, Chakos MH, Swartz MS, Keefe RS, Stroup TS, Lieberman JA, Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. Extrapyramidal side effects of antipsychotics in a randomised trial. Br J Psychiatry. 2008;193:279–88.
Kahn RS, Fleischhacker WW, Boter H, Davidson M, Vergouwe Y, Keet IP, Gheorghe MD, Rybakowski JK, Galderisi S, Libiger J, Hummer M, Dollfus S, López-Ibor JJ, Hranov LG, Gaebel W, Peuskens J, Lindefors N, Riecher-Rössler A, Grobbee DE, EUFEST study group. Effectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trial. Lancet. 2008;371(9618):1085–97.
Sikich L, Frazier JA, McClellan J, Findling RL, Vitiello B, Ritz L, Ambler D, Puglia M, Maloney AE, Michael E, De Jong S, Slifka K, Noyes N, Hlastala S, Pierson L, McNamara NK, Delporto-Bedoya D, Anderson R, Hamer RM, Lieberman JA. Double-blind comparison of first- and second-generation antipsychotics in early-onset schizophrenia and schizo-affective disorder: findings from the treatment of early-onset schizophrenia spectrum disorders (TEOSS) study. Am J Psychiatry. 2008;165:1420–31.
Gao K, Kemp DE, Ganocy SJ, Gajwani P, Xia G, Calabrese JR. Antipsychotic-induced extrapyramidal side effects in bipolar disorder and schizophrenia: a systematic review. J Clin Psychopharmacol. 2008;28:203–9.
Rummel-Kluge C, Komossa K, Schwarz S, Hunger H, Schmid F, Kissling W, Davis JM, Leucht S. Second-generation antipsychotic drugs and extrapyramidal side effects: a systematic review and meta-analysis of head-to-head comparisons. Schizophr Bull. 2012;38:167–77.
Demyttenaere K, Detraux J, Racagni G, Vansteelandt K. Medication induced akathisia with newly approved antipsychotics in patients with a severe mental illness: a systematic review and meta-analysis. CNS Drugs. 2019;33:549–66.
Martino D, Karnik V, Osland S, Barnes TRE, Pringsheim TM. Movement disorders associated with antipsychotic medication in people with schizophrenia: an overview of Cochrane reviews and meta-analysis. Can J Psychiatry. 2018;63:730–9.
Pringsheim T, Gardner D, Addington D, et al. The assessment and treatment of antipsychotic-induced akathisia. Can J Psychiatry. 2018;63:719–29.
Lonnen AJ, Stahl SM. The mechanism of drug-induced akathisia. CNS Spectr. 2011;16:7–10.
Lima AR, Bacalcthuk J, Barnes TR, Soares-Weiser K. Central action beta-blockers versus placebo for neuroleptic-induced acute akathisia. Cochrane Database Syst Rev. 2004;4:CD001946.
Adler LA, Angrist B, Retter S, et al. Neuroleptic-induced akathisia: a review. Psychopharmacology. 1989;97:1–11.
Lima AR, Weiser KV, Bacaltchuk J, Barnes TR. Anticholinergics for neuroleptic-induced acute akathisia. Cochrane Database Syst Rev. 2004;1:CD003727.
Fleischhacker WW, Roth SD, Kane JM. The pharmacologic treatment of neuroleptic-induced akathisia. J Clin Psychopharmacol. 1990;10:12–211.
Rathbone J, Soares-Weiser K. Anticholinergics for neuroleptic-induced acute akathisia. Cochrane Database Syst Rev. 2006;4:CD003727.
Barnes TR, McPhillips MA. Critical analysis and comparison of the side-effect and safety profiles of the new antipsychotics. Br J Psychiatry Suppl. 1999;38:34–43.
Kutcher S, Williamson P, MacKenzie S, et al. Successful clonazepam treatment of neuroleptic-induced akathisia in older adolescents and young adults: a double-blind, placebo-controlled study. J Clin Psychopharmacol. 1989;9:403–6.
Pujalte D, Bottaï T, Huë B, et al. A double-blind comparison of clonazepam and placebo in the treatment of neuroleptic-induced akathisia. Clin Neuropharmacol. 1994;17:236–42.
Lima AR, Soares-Weiser K, Bacaltchuk J, Barnes TR. Benzodiazepines for neuroleptic-induced acute akathisia. Cochrane Database Syst Rev. 2002;1:CD001950.
Meltzer HY. The role of serotonin in antipsychotic drug action. Neuropsychopharmacol. 1999;21(suppl. 2):106S–15S.
Kapur S, Remington G. Serotonin–dopamine interaction and its relevance to schizophrenia. Am J Psychiatry. 1996;153:466–76.
Poyurovsky M, Weizman A. Serotonergic agents in the treatment of acute neuroleptic-induced akathisia: open-label study of buspirone and mianserin. Int Clin Psychopharmacol. 1997;12:263–8.
Lane RM. SSRI-induced extrapyramidal side effects and akathisia: implications for treatment. J Psychopharmacol. 1998;12:192–21414.
Kapur S, Remington G. Atypical antipsychotics: new directions and new challenges in the treatment of schizophrenia. Annu Rev Med. 2001;52:503–17.
Miller GH, Fleischhacker WW, Ehrman H, et al. Treatment of neuroleptic-induced akathisia with the 5-HT2 antagonist ritanserin. Psychopharmacol Bull. 1990;26:373–6.
Poyurovsky M. Acute antipsychotic-induced akathisia revisited. Br J Psychiatry. 2010;196:89–91.
Miller CH, Hummer M, Pycha R, et al. The effect of ritanserin on treatment-resistant neuroleptic-induced akathisia: case reports. Prog Neuropsychopharmacol Biol Psychiatry. 1992;16:247–51.
Weiss D, Aizenberg D, Hermesh H, et al. Cyproheptadine treatment in neuroleptic-induced akathisia. Br J Psychiatry. 1995;167:483–6.
Fischel T, Hermesh H, Aizenberg D, Zemishlany Z, Munitz H, Benjamini Y, Weizman A. Cyproheptadine vs. propranolol for the treatment of acute neuroleptic-induced akathisia: a comparative double-blind study. J Clin Psychopharmacol. 2001;21:612–5.
Stryjer R, Strous RD, Bar F, Poyurovsky M, Weizman A, Kotler M. Treatment of neuroleptic-induced akathisia with the 5-HT2a antagonist trazodone. Clin Neuropharmacol. 2003;26(3):137–41. https://doi.org/10.1097/00002826-200305000-00006.
Stryjer R, Rosenzcwaig S, Bar F, Ulman AM, Weizman A, Spivak B. Trazodone for the treatment of neuroleptic-induced acute akathisia: a placebo-controlled, double-blind, crossover study. Clin Neuropharmacol. 2010;33:219–22.
Ribosa-Nogué R, Pagonabarraga J, Kulisevsky J. Efficacy of trazodone in antipsychotic-induced akathisia resistant to conventional treatment. Parkinsonism Relat Disord. 2012;18:902–3.
Poyurovsky M, Fuchs C, Weizman A. Low-dose mianserin in the treatment of acute neuroleptic-induced akathisia. J Clin Psychopharmacol. 1998;18:253–4.
Poyurovsky M, Shardorodsky M, Fuchs C, et al. Treatment of neuroleptic-induced akathisia with the 5-HT2 antagonist mianserin. Double-blind, placebo-controlled study. Br J Psychiatry. 1999;174:238–42.
Hirose S. The causes of underdiagnosing akathisia. Schizophr Bull. 2003;29:547–58.
Poyurovsky M, Epshtein S, Fuchs C, et al. Efficacy of low-dose mirtazapine in neuroleptic-induced akathisia: a double-blind randomized placebo-controlled pilot study. J Clin Psychopharmacol. 2003;23:305–8.
Poyurovsky M, Pashinian A, Weizman R, Fuchs C, Weizman A. Low-dose mirtazapine: a new option in the treatment of antipsychotic-induced akathisia. A randomized, double-blind, placebo- and propranolol-controlled trial. Biol Psychiatry. 2006;59:1071–7.
Praharaj SM, Kongasseri S, Behere RV, Sharma PS. Mirtazapine for antipsychotic-induced acute akathisia: a systematic review and meta-analysis of randomized placebo-controlled trials. Ther Adv Psychopharmacol. 2015;5:307–13.
Laoutidis ZG, Luckhaus C. 5-HT2a receptor antagonists for the treatment of neuroleptic-induced akathisia: a systematic review and meta-analysis. Int J Neuropsychopharmacol. 2014;17:823–32.
Mamo D, Graff A, Mizrahi R, Shammi CM, Romeyer F, Kapur S. Differential effects of aripiprazole on D(2), 5-HT(2), and 5-HT(1A) receptor occupancy in patients with schizophrenia: a triple tracer PET study. Am J Psychiatry. 2007;164(9):1411–7.
Poyurovsky M, Weizman R, Weizman A. Aripiprazole's receptor pharmacology and extrapyramidal side effects. Am J Psychiatry. 2008;165:398.
Citrome L. Aripiprazole, brexpiprazole and cariprazine: not all the same. Curr Psychiatry. 2018;17:25–34.
Poyurovsky M, Bergman J, Pashinian A, Weizman A. Beneficial effect of low-dose mirtazapine in acute aripiprazole-induced akathisia. Int Clin Psychopharmacol. 2014;29:296–8.
Poyurovsky M, Weizman A. Very Low-Dose Mirtazapine (7.5 mg) in Treatment of Acute Antipsychotic-Associated Akathisia. J Clin Psychopharmacol. 2018;38:609–11.
Ruwe F, Jzerman-Boon P, Roth T, et al. A phase 2 randomized dose-finding study with esmirtazapine in patients with primary insomnia. J Clin Psychopharmacol. 2016;36:457–64.
Koller K. Propranolol for mirtazapine-induced akathisia: Single case report. Ment Health Clin [Internet]. 2019;9:61–3.
Patel RS, Bhela J, Tahir M, Pisati SR, Hossain S. Pimavanserin in Parkinson's disease-induced psychosis: a literature review. Cureus. 2019;11(7):e5257.
Poyurovsky M, Weizman A. Lack of efficacy of the 5-HT3 receptor antagonist granisetron in the treatment of acute neuroleptic-induced akathisia. Int Clin Psychopharmacol. 1999;14:357–60.
Avital A, Gross-Isseroff R, Stryjer R, Hermesh H, Weizman A, Shiloh R. Zolmitriptan compared to propranolol in the treatment of acute neuroleptic-induced akathisia: a comparative double-blind study. Eur Neuropsychopharmacol. 2009;19:476–82.
Miller CH, Fleischhacker WW, Ehrmann H, Kane JM. Treatment of neuroleptic induced akathisia with the 5-HT2 antagonist ritanserin. Psychopharmacol Bull. 1990;26(3):373–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
There were no sources of funding for the study or for preparation of the manuscript.
Conflict of interest
There are no conflicts of interest to report for either author.
Rights and permissions
About this article
Cite this article
Poyurovsky, M., Weizman, A. Treatment of Antipsychotic-Induced Akathisia: Role of Serotonin 5-HT2a Receptor Antagonists. Drugs 80, 871–882 (2020). https://doi.org/10.1007/s40265-020-01312-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-020-01312-0