Abstract
Introduction
In addition to the growing interest of different cannabinoids for therapeutic purposes, the safety profile of these substances has changed, with the recent identification of new events such as acute pancreatitis.
Objective
The aim of this study was to characterize cannabinoid-related acute pancreatitis, based on the recent literature and the analysis of pharmacovigilance data available worldwide.
Methods
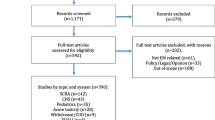
Nine national and international pharmacovigilance databases were requested for individual case safety reports of acute pancreatitis related to cannabinoid exposure. A systematic review was performed searching in PubMed®, Web of Science®, and Google Scholar® for any publication dealing with acute pancreatitis and cannabinoid exposure (cannabis, cannabinoid, cannabidiol, tetrahydrocannabinol, nabilone, dronabinol), to identify case reports, observational studies, clinical trials, or reviews. All queries were updated on 1 January, 2021.
Results
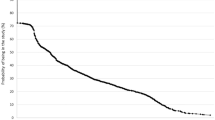
Twenty-two individual case safety reports were identified in the pharmacovigilance databases and 51 in the literature, corresponding to a predominantly young male population (74% of men, median age 28 interquartile range [21–39]) using recreational Cannabis sativa with high intensity. A therapeutic purpose was identified in 13 cases (including tetrahydrocannabinol, cannabidiol, and dronabinol). The outcome was often favorable after dechallenge (except three deaths), and frequent recurrences were observed in the case of rechallenge or sustained consumption. Eleven cross-sectional studies and one ecological study showed an increasing trend of cannabis use in in-patients with acute pancreatitis, with a significantly lower in-hospital mortality.
Conclusions
This review underlines that acute pancreatitis is a potential adverse effect of cannabinoid use. It remains often unrecognized and can occur during recreational or therapeutic use. The development of the therapeutic use of cannabinoids in frail patients deserves a better investigation of the benefit-risk ratio of these different products.


Similar content being viewed by others
References
EMCDDA. European drug report 2019: trends and developments. Lisbon: EMCDDA; 2019.
Goodman S, Wadsworth E, Leos-Toro C, Hammond D, International Cannabis Policy Study Team. Prevalence and forms of cannabis use in legal vs. illegal recreational cannabis markets. Int J Drug Policy. 2020;76:102658.
Bouquet E, Pain S, Eiden C, Jouanjus E, Richard N, Fauconneau B, French Addictovigilance Network, et al. Adverse events of recreational cannabis use reported to the French addictovigilance network (2012–2017). Br J Clin Pharmacol. 2021;87(10):3925–37.
Meczker A, Hanak L, Parniczky A, Szentesi A, Eross B, Hegyi P, et al. Analysis of 1060 cases of drug-induced acute pancreatitis. Gastroenterology. 2020;159(5):1958–61.
Vivian E, Cler L, Conwell D, Cote GA, Dickerman R, Freeman M, et al. Acute Pancreatitis Task Force on Quality: development of quality indicators for acute pancreatitis management. Am J Gastroenterol. 2019;114(8):1322–42.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89.
Fouretier A, Malriq A, Bertram D. Open access pharmacovigilance databases: analysis of 11 databases. Pharm Med. 2016;30(4):221–31.
Berbain T, Pariente A, Miremont-Salamé G, Grandvuillemin A, Micallef J, Chouchana L, et al. Contribution of causality assessment for an automated detection of safety signals: an example using the French Pharmacovigilance Database. Drug Saf. 2020;43(3):243–53.
Lindquist M. VigiBase, the WHO global ICSR database system: basic facts. Drug Inf J. 2008;42(5):409–19.
Aach RA. Acute-pancreatitis after marijuana smoking: is there a relationship. JAMA 1985. 1985;253(12):1791.
Grant P, Gandhi P. A case of cannabis-induced pancreatitis. J Pancreas. 2004;5(1):41–3.
Bournet B, Buscail L. Cannabis: a rare cause of acute pancreatitis. Gastroenterol Clin Biol. 2008;32(11):922–3.
Lingutla D, Rohatgi A, Li J, Sorrentino S, DiSalle M, Leschingski R. Cannabis induced pancreatitis. Am J Gastroenterol. 2009;104:S236–7.
Belze O Jr, Legras A, Ehrmann S, Garot D, Perrotin D. Cannabis-induced acute pancreatitis. Am J Emerg Med. 2011;29(1):131.e3-4.
Safsaf H, Stirnemann J, Maire F, Fain O. Pancréatite aiguë au cannabis: une étiologie classique ? Rev Med Interne. 2011;32:S376–7.
Zayouna N, Dudar A, Iskanderian Z, Stawick L, Ahsan S. Acute pancreatitis secondary to marijuana use. Am J Gastroenterol. 2012;107:S339.
Howaizi M, Chahine M, Haydar F, Jemaa Y, Lapoile E. Cannabis-induced recurrent acute pancreatitis. Acta Gastroenterol Belg. 2012;75(4):446–7.
Fatma H, Mouna B, Leila M, Radhouane D, Taoufik N. Cannabis: a rare cause of acute pancreatitis. Clin Res Hepatol Gastroenterol. 2013;37(1):e24–5.
Jalal T, Ramchandani H. Cannabis abuse: a rare cause of acute pancreatitis. J Gen Intern Med. 2013;28;S304.
Kayar Y, Eroglu H, Pamukcu O, Cetin H, Kocas O, Atci M. Cannabinoid-induced acute pancreatitis. Turk J Gastroenterol. 2014;25(3):335–6.
Akkucuk MH, Erbayrak M. A rare and unexpected side-effect of cannabis use: abdominal pain due to acute pancreatitis. Case Rep Emerg Med. 2015. https://doi.org/10.1155/2015/463836.
Gino M, Mete F. A rare case of acute pancreatitis. Italian J Med. 2015;9(S2):47.
Lorvellec A, Thiriet L, Andrianjafy C, Gervaise A, Seigne AL, Rey P. Recurrent cannabis-induced acute pancreatitis. Presse Medicale. 2015;44(4 Pt 1):468–71.
Nayak SK, Preethi M, Zanwar S, Palaniswamy KR. Cannabis induced recurrent acute pancreatitis. Trop Doct. 2016;46(4):238–9.
Espino García A, Jorge Tufet C, Lafarga Giribets MA, Justribó Sánchez ME, Carré GG. Cannabis-induced pancreatitis. SEMERGEN. 2016;42(2):123–4.
Herrero LN, Chaucer B, Singh S, Deshpande V, Patel SH. Acute pancreatitis secondary to marijuana consumption. J Pancreas. 2016;17(3):322–3.
Tripathi N, Koirala N. Cannabinoid induced pancreatitis: a case report and literature review. J Gen Emerg Med. 2017;2(5):1–4.
Basnyat S, Patel M, Irfan H, Nandish B, Steinberger D. An unusual case of marijuana induced acute pancreatitis. Chest. 2018;154(4):331a.
Szurnicki P, Alansari A, Alansari T, Khan G. Cannabis as an overlooked cause of acute pancreatitis: a case report and literature review: 1383. Am J Gastroenterol. 2018;113:S794.
Ghazaleh S, Alqahtani A, Nehme C, Abugharbyeh A, Said Ahmed TS. A rare case of cannabis-induced acute pancreatitis. Cureus. 2019;11(6):e4878.
Pagliari D, Saviano A, Brizi MG, Mancarella FA, Cannone F, Musso M, et al. Cannabis-induced acute pancreatitis: a case report with comprehensive literature review. Eur Rev Med Pharmacol Sci. 2019;23(19):8625–9.
Chandy J, Hassan A, Sciarra M. “HASH”ing out pancreatitis: the new increasingly common culprit. J Community Hosp Intern Med Perspect. 2019;9(4):360–1.
John J, Gandhi S, Nam D, Niakan L. A case of cannabis-induced acute pancreatitis. Cureus. 2019;11(9):e5754.
Hutflesz C, Parihar V. Clinical innovation poster abstracts: medical cannabis induced acute pancreatitis and hyperemesis syndrome in a patient with a complex regional pain syndrome. Can J Pain. 2019;3(1):A50-72.
Ahuja AC, Aijazi M. Severe acute pancreatitis secondary to topical cannabinoid use: 3031. Am J Gastroenterol. 2019;114(2019 ACG Annual Meeting Abstracts):1637.
Osueni A, Osueni GI, Mbamalu DC, Owoseni O, Nemakallu SR. A smoked-out pancreas: an unusual case of acute pancreatitis. Am J Gastroenterol. 2020;115:S1742–3.
Singh R, Torre K, Saba M, Stepczynski J. Cannabis-induced pancreatitis: a new clinical entity. Pancreas. 2020;49(7):e66–7.
Wargo KA, Geveden BN, McConnell VJ. Cannabinoid-induced pancreatitis: a case series. J Pancreas. 2007;8(5):579–83.
Culetto A, Bournet B, Haennig A, Alric L, Peron JM, Buscail L. Prospective evaluation of the aetiological profile of acute pancreatitis in young adult patients. Digest Liver Dis. 2015;47(7):584–9.
Culetto A, Bournet B, Buscail L. Clinical profile of cannabis-associated acute pancreatitis. Digest Liver Dis. 2017;49(11):1284–5.
Mikolašević I, Milić S, Mijandrušić-Sinčić B, Licul V, Štimac D. Cannabis-induced acute pancreatitis. Med Glas. 2013;10(2):405–7.
Chadalavada P, Simons-Linares CR, Chahal P. Drug-induced acute pancreatitis: prevalence, causative agents, and outcomes. Pancreatology. 2020;20(7):1281–6.
Hutflesz C, Parihar V. Medical cannabis induced acute pancreatitis and hyperemesis syndrome in a patient with complex regional pain syndrome. Can J Pain. 2019;3(1): A71.
Goyal H, Guerreso K, Smith B, Harper K, Patel S, Patel A, et al. Severity and outcomes of acute alcoholic pancreatitis in cannabis users. Transl Gastroenterol Hepatol. 2017;2:60.
Goyal H, Desai R, Patel U, Perisetti A, Chhabra R. Outcomes of acute pancreatitis treatment in the cannabis users: a nationwide propensity matched analysis. Am J Gastroenterol. 2018;113:S51-S.
Njei B, McCarty TR, Sharma P, Singh M, Haque L, Aslanian H, et al. Cannabis use disorder is associated with increased risk of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis: analysis of the U.S. Nationwide Inpatient Sample (NIS) Database, 2004–2014. ACG. 2017;112:S19.
Njei B, Sharma P, McCarty TR, Singh M, Haque L, Aslanian HR, et al. Cannabis use is associated with increased risk of post–endoscopic retrograde cholangiopancreatography pancreatitis: analysis of the US nationwide inpatient sample database, 2004–2014. Pancreas. 2018;47(9):1142–9.
Simons-Linares CR, Barkin JA, Wang Y, Jaiswal P, Trick W, Bartel MJ, et al. Is there an effect of cannabis consumption on acute pancreatitis? Dig Dis Sci. 2018;63(10):2786–91.
Adejumo AC, Akanbi O, Adejumo KL, Bukong TN. Reduced risk of alcohol-induced pancreatitis with cannabis use. Alcohol Clin Exp Res. 2019;43(2):277–86.
Enofe I, Igenoza O, Osaghae O, Rai M, Aluko A, Laird-Fick H. Prevalence of acute pancreatitis among cannabis users: review of the National Inpatient Sample database. HPB. 2019;21:S118–9.
Nemer L, Hinton A, Krishna S, Conwell D, Lara L. 31 The relationship between acute pancreatitis and cannabis use before and after recreational legalization in select States. ACG. 2019;114:S19.
Salazar M, Abou Saleh M, Barkin JA, Elkhouly MA, Mansoor E, Barkin JS, et al. 29 cannabis use is associated with worse outcomes in acute pancreatitis: analysis of a large database. ACG. 2019;114:S16–8.
Salazar M, Barkin JA, Ramey JS, Kumapley R, Paintsil I, Barkin JS, et al. 20 comparison and outcomes of cannabis users with acute pancreatitis according to severity using the Revised Atlanta Classification of Acute Pancreatitis. ACG. 2019;114:S11.
Salazar M, Ramey JS, Barkin JA, Kumapley R, Paintsil I, Barkin JS, et al. 19 outcomes of acute necrotizing pancreatitis and associated fluid collections in cannabis users. ACG. 2019;114:S11.
Saleem S, Then EO, Abu-Heija A, Weissman S, Gaduputi V. 22 association between acute pancreatitis and cannabis use: a US population-based study. ACG. 2019;114:S12–3.
Sarmini MT. Evaluation of acute pancreatitis and cannabis use association and outcomes: a cross sectional study using large inpatient data. Eur J Biomed. 2019;6(7):72–7.
Simons-Linares CR, Barkin JA, Jang S, Bhatt A, Lopez R, Stevens T, et al. The impact of cannabis consumption on mortality, morbidity, and cost in acute pancreatitis patients in the United States: a 10-year analysis of the National Inpatient Sample. Pancreas. 2019;48(6):850–5.
Bolourani S, Diao L, Thompson DA, Wang P, Coppa GF, Patel VM, et al. Risk factors for early readmission after acute pancreatitis: importance of timely interventions. J Surg Res. 2020;252:96–106.
Barkin JA, Nemeth Z, Saluja AK, Barkin JS. Cannabis-induced acute pancreatitis: a systematic review. Pancreas. 2017;46(8):1035–8.
Buscail L, Le Cosquer G, Gilletta C, Bournet B, Culetto A. Cannabis et pancréatite aiguë. La Presse Méd Formation. 2020;1(4):373–7.
Sagaram M, Sundar P, Reddy S. S0021Cannabis-induced acute pancreatitis: a systematic review. Am J Gastroenterol. 2020;115(1):S10-S.
Weissman S, Aziz M, Perumpail RB, Mehta TI, Patel R, Tabibian JH. Ever-increasing diversity of drug-induced pancreatitis. World J Gastroenterol. 2020;26(22):2902–15.
Kim J, Lee KJ, Kim JS, Rho JG, Shin JJ, Song WK, et al. Cannabinoids regulate Bcl-2 and cyclin D2 expression in pancreatic beta cells. PLoS ONE. 2016;11(3):e0150981.
Kim W, Lao Q, Shin YK, Carlson OD, Lee EK, Gorospe M, et al. Cannabinoids induce pancreatic beta-cell death by directly inhibiting insulin receptor activation. Sci Signal. 2012;5(216):ra23.
Gotfried J, Naftali T, Schey R. Role of cannabis and its derivatives in gastrointestinal and hepatic disease. Gastroenterology. 2020;159(1):62–80.
Zyromski NJ, Mathur A, Wade T, Wang S, Swartz-Basile DA, Prather A, et al. Cannabinoid receptor blockade attenuates acute pancreatitis by an adiponectin mediated mechanism. Gastroenterology. 2008;134(4):A876-A.
Van Rafelghem B, Covaci A, Anseeuw K, van Nuijs ALN, Neels H, Mahieu B, et al. Suicide by vaping the synthetic cannabinoid 4F-MDMB-BINACA: cannabinoid receptors and fluoride at the crossroads of toxicity? Forensic Sci Med Pathol. 2021;17: 684–688.
de Almeida DL, Devi LA. Diversity of molecular targets and signaling pathways for CBD. Pharmacol Res Perspect. 2020;8(6):e00682.
Utomo WK, de Vries M, van Rijckevorsel DC, Peppelenbosch MP, van Goor H, Fuhler GM. Cannabinoid receptor agonist namisol does not affect cytokine levels in chronic pancreatitis patients. Am J Gastroenterol. 2015;110(8):1244–5.
de Vries M, Van Rijckevorsel DC, Vissers KC, Wilder-Smith OH, Van Goor H. Single dose delta-9-tetrahydrocannabinol in chronic pancreatitis patients: analgesic efficacy, pharmacokinetics and tolerability. Br J Clin Pharmacol. 2016;81(3):525–37.
Charilaou P, Agnihotri K, Garcia P, Badheka A, Frenia D, Yegneswaran B. Trends of cannabis use disorder in the inpatient: 2002 to 2011. Am J Med. 2017;130(6):678-87.e7.
Lara LF, Nemer L, Hinton A, Balasubramanian G, Conwell DL, Krishna S. Acute and severe acute pancreatitis and the effect of cannabis in States before and after legalization compared with States without legalized cannabis. Pancreas. 2021;50(5):766–72.
Han B, Gfroerer JC, Colliver JD. Associations between duration of illicit drug use and health conditions: results from the 2005–2007 national surveys on drug use and health. Ann Epidemiol. 2010;20(4):289–97.
Lafaurie M, Pochard L, Lotiron C, Molinier L, Lapeyre-Mestre M, Jouanjus E. Identification of somatic disorders related to psychoactive drug use from an inpatient database in a French University Hospital. Clin Drug Investig. 2018;38(10):977–82.
Bhandari R, Gupta S, Modi K, Raval MR, Joundi H, Patel JR, et al. Persistent cannabis abuse and risk for hospitalization for acute pancreatitis: a cross-sectional study in United States hospitals. Cureus. 2021;13(6):e15601.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This work has been conducted in the context of a research master training of Camille Azam at the University of Toulouse.
Conflicts of interest/Competing interests
Camille Azam, Adrian Culetto, and Maryse Lapeyre-Mestre declare that they have no conflict of interest. Louis Buscail has received research grants from CVASTHERA pharmaceutical.
Ethics approval
This study did not required any specific ethics approval, case reports included have been already published in the scientific literature, or are accessible through open or restricted national or international pharmacovigilance databases.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
As indicated in the article, data extracted from the open pharmacovigilance databases can be extracted by any individual. Information from databases with a restricted access can be obtained on request from the Uppsala Monitoring Center and/or from national pharmacovigilance centers. All data used and generated in the literature review are presented in the main text of the article or in the ESM. All literature cases are available as published on request.
Code availability
Not applicable.
Authors’ contributions
MLM had the idea for the article, CA and MLM performed the literature search, data extraction and data analysis, and the pharmacovigilance database search, LB and EC provided their list of references and published case series, CA drafted the first draft, and all authors revised the work and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Azam, C., Buscail, L., Culetto, A. et al. Cannabinoid-Related Acute Pancreatitis: An Update from International Literature and Individual Case Safety Reports. Drug Saf 45, 215–235 (2022). https://doi.org/10.1007/s40264-022-01146-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-022-01146-7