Abstract
Background
The likelihood to help or harm (LHH) is an absolute measure of the benefit versus risk profile of a medication, which can be used to assess the potential for benefit versus harm of different disease-modifying treatments (DMTs) for relapsing multiple sclerosis (R-MS) and facilitate clinical decision-making.
Objective
The objective of this study was to assess absolute differences in benefit:risk ratios of oral DMTs for R-MS, using LHH analysis with no evidence of disease activity (NEDA) as beneficial outcome.
Design/Methods
The number needed to treat for a paient to achieve NEDA (NNTBNEDA) was used as an effect size metric of efficacy and the number needed to treat for a patient to experience an adverse event (NNTHAE), a serious adverse event (NNTHSAE), or treatment discontinuation due to an adverse event (NNTHAE-D) were used as measures of risk. The LHH—which is the ratio of NNTH:NNTB—values were calculated from published phase III trial data for oral DMTs.
Results
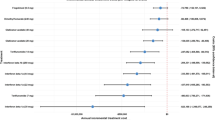
The values for likelihood to achieve NEDA than experience any AE ratio (LHH(AE/NEDA)) were 3.9, 6.8, 12.5 and 3.7, the likelihood to achieve NEDA than experience a SAE ratio (LHH(SAE/NEDA)) values were 3.5, 15, 23.5 and 2.8, and the likelihood to achieve NEDA versus discontinue treatment (LHH(AE-D/NEDA)) values were 20.3, 4.3, 3.9 and 3.1 for cladribine, dimethyl-fumarate, fingolimod, and teriflunomide, respectively.
Conclusions
With all of the oral DMTs examined, R-MS patients are more likely to achieve NEDA than experience any adverse event.

Similar content being viewed by others
Change history
20 December 2018
NEDA was evaluated as the proportion of patients free of relapses, 3-month confirmed disability progression, and free of new or newly enlarging T2 lesion and Gadolinium enhancing lesions.
References
Citrome L, Ketter TA. When does a difference make a difference? Interpretation of number needed to treat, number needed to harm, and likelihood to be helped to harmed. Int J Clin Pract. 2013;67:407–11.
Andrade C. Likelihood of being helped or harmed as a measure of clinical outcomes in psychopharmacology. J Clin Psychiatr. 2017;78:e73–5.
Parks NE, Flanagan EP, Lucchinetti CF, Wingerchuk DM. NEDA treatment target? No evident disease activity as an actionable outcome in practice. J Neurol Sci. 2017;383:31–4.
Giovannoni G, Turner B, Gnanapavan S, Offiah C, Schmierer K, Marta M. Is it time to target no evident disease activity (NEDA) in multiple sclerosis? Mult Scler Relat Disord. 2015;4:329–33.
Giovannoni G, Tomic D, Bright JR, Havrdová E. “No evident disease activity”: the use of combined assessments in the management of patients with multiple sclerosis. Mult Scler. 2017;23:1179–87.
Hincapie AL, Penm J, Burns CF. Factors associated with patient preferences for disease-modifying therapies in multiple sclerosis. J Manag Care Spec Pharm. 2017;23:822–30.
Higuera L, Carlin CS, Anderson S. adherence to disease-modifying therapies for multiple sclerosis. J Manag Care Spec Pharm. 2016;22:1394–401.
Mitsikostas DD, Goodin DS. Comparing the efficacy of disease modifying therapies in multiple sclerosis. Mult Scler Relat Disord. 2017;18:109–16.
Mendes D, Alves C, Batel-Marques F. Benefit-risk of therapies for relapsing-remitting multiple sclerosis: testing the number needed to treat to benefit (NNTB), number needed to treat to harm (NNTH) and the likelihood to be helped or harmed (LHH): a systematic review and meta-analysis. CNS Drugs. 2016;30:909–29.
Freedman MS, Montalban X, Miller AE, Dive-Pouletty C, Hass S, Thangavelu K, et al. Comparing outcomes from clinical studies of oral disease-modifying therapies (dimethyl fumarate, fingolimod, and teriflunomide) in relapsing MS: assessing absolute differences using a number needed to treat analysis. Mult Scler Relat Disord. 2016;10:204–12.
Giovannoni G, Comi G, Cook S, Rammohan K, Rieckmann P, Soelberg Sorensen P, et al. CLARITY study Group. A placebo-controlled trial of oral cladribine for relapsing multiple sclerosis. N Engl J Med. 2010;362:416–26.
Gold R, Kappos L, Arnold DL, Bar-Or A, Giovannoni G, Selmaj K, et al. DEFINE Study Investigators. Placebo-controlled phase 3 study of oral BG-12 for relapsing multiple sclerosis. N Engl J Med. 2012;367:1098–107.
Fox RJ, Miller DH, Phillips JT, Hutchinson M, Havrdova E, Kita M, et al. CONFIRM Study Investigators. Placebo-controlled phase 3 study of oral BG-12 or glatiramer in multiple sclerosis. N Engl J Med. 2012;367:1087–97.
Kappos L, Radue E-W, O’Connor P, Polman C, Hohlfeld R, Calabresi P, et al. FREEDOMS Study Group. A placebo-controlled trial of oral fingolimod in relapsing multiple sclerosis. N Engl J Med. 2010;362:387–401.
Calabresi PA, Radue E-W, Goodin D, Jeffery D, Rammohan KW, Reder AT, et al. Safety and efficacy of fingolimod in patients with relapsing-remitting multiple sclerosis (FREEDOMS II): a double-blind, randomized, placebo-controlled, phase 3 trial. Lancet Neurol. 2014;13:545–56.
O’Connor P, Wolinsky JS, Confavreux C, Comi G, Kappos L, Olsson TP, et al. TEMSO Trial Group. Randomised trial of oral teriflunomide for relapsing multiple sclerosis. N Engl J Med. 2011;365:1293–303.
Confavreaux C, O’Connor P, Comi G, Freedman MS, Miller AE, Olsson TP, et al. TOWER Trial Group. Oral teriflunomide for patients with relapsing multiple sclerosis (TOWER): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol. 2014;13:247–56.
Havrdova E, Giovannoni G, Gold R, Fox RJ, Kappos L, Phillips JT, et al. Effect of delayed-release dimethyl fumarate on no evidence of disease activity in relapsing-remitting multiple sclerosis: integrated analysis of the phase III DEFINE and CONFIRM studies. Eur J Neurol. 2017;24:726–33.
Viglietta V, Miller D, Bar-Or A, Phillips JT, Arnold DL, Selmaj K, et al. Efficacy of delayed-release dimethyl fumarate in relapsing-remitting multiple sclerosis: integrated analysis of the phase III trials. Ann Clin Transl Neurol. 2015;2:103–18.
Kappos L, De Stefano N, Freedman MS, Cree BA, Radue EW, Sprenger T, et al. Inclusion of brain volume loss in a revised measure of ‘no evidence of disease activity’ (NEDA-4) in relapsing-remitting multiple sclerosis. Mult Scler J. 2016;22:1297–305.
Giovannoni G, Cook S, Rammohan K, Rieckmann P, Sørensen PS, Vermersch P, et al. CLARITY study group. Sustained disease-activity-free status in patients with relapsing-remitting multiple sclerosis treated with cladribine tablets in the CLARITY study: a post hoc and subgroup analysis. Lancet Neurol. 2011;10:329–37.
Freedman M, O’Connor P, Wolinsky J, Confavreux C, Comi G, Kappos L, et al. Teriflunomide increases the proportion of patients free from disease activity in the TEMSO phase III study. Neurology. 2012;78(suppl):PD5.007.
Altman DG. Confidence intervals for the number needed to treat. BMJ. 1998;317:1309–12.
Dahdaleh D, Sharrack B. We can compare the relative efficacy of multiple sclerosis medications by examining the results of independent clinical trials: yes. Mult Scler J. 2015;21:35–6.
Ciccarelli O, Chataway J. We can compare the relative efficacy of multiple sclerosis medications by examining the results of independent clinical trials: no. Mult Scler J. 2015;21:37–8.
Zakaria M. Smoke and mirrors: limited value of relative risk reductions for assessing the benefits of disease-modifying therapies for multiple sclerosis. Mult Scler Relat Disord. 2015;4:187–91.
Goodin DS. Disease-modifying therapy in multiple sclerosis: update and clinical implications. Neurology 2008;71:(24 Suppl 3) S8–13.
Citrome L. Relative vs. absolute measures of benefit and risk: what’s the difference? Acta Psychiatr Scand. 2010;121:94–102.
Nixon R, Bergvall N, Tomic D, Sfikas N, Cutter G, Giovannoni G. No evidence of disease activity: indirect comparisons of oral therapies for the treatment of relapsing-remitting multiple sclerosis. Adv Ther. 2014;31:1134–56.
Goodin DS, Mitsikostas DD. Reply to Tsivgoulis and colleagues comments [letter]. Mult Scler Relat Disord. 2018;21:120–1.
Goltz HH, Smith ML. Yule-Simpson’s paradox in research. Pract Assess Res Eval. 2010;15:1–9.
Acknowledgements
The authors thank Dr S.J. Kedikoglou, MD, MPH, PhD and Mrs. E. Delicha, MSc for their expert statistical advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval and Consent
No ethics approval or patient consent was obtained because all data used in this study were collected from previously published peer-reviewed articles.
Conflict of interest
DP has received consulting, speaking fees, and travel grants from Bayer, Genesis Pharma, Merck, Novartis, Roche, Sanofi-Aventis, Specifar, and Teva. DDM has received consulting, speaking fees, and travel grants from Allergan, Amgen, Cefaly, ElectroCore, Genesis Pharma, Eli Lily, Merck-Serono, Novartis, Roche, Sanofi-Genzyme, Speficar, and Teva.
Funding
No funding source had a role in the conception and preparation of this article.
Rights and permissions
About this article
Cite this article
Papadopoulos, D., Mitsikostas, DD.D. Oral Disease-Modifying Treatments for Relapsing Multiple Sclerosis: A Likelihood to Achieve No Evidence of Disease Activity or Harm Analysis. CNS Drugs 32, 1069–1078 (2018). https://doi.org/10.1007/s40263-018-0547-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-018-0547-z