Abstract
Background and Objective
Posaconazole (PSZ) is a triazole antifungal for the management of invasive fungal disease (IFD) in adults and children. Although PSZ is available as an intravenous (IV) solution, oral suspension (OS) and delayed-release tablets (DRTs), OS is the preferred formulation for pediatric use because of potential safety concerns associated with an excipient in the IV formulation and difficulty in swallowing intact tablets by children. However, poor biopharmaceutical characteristics of the OS formulation leads to an unpredictable dose-exposure profile of PSZ in children, potentially risking therapeutic failure. The goal of this study was to characterize the population pharmacokinetics (PK) of PSZ in immunocompromised children and assess therapeutic target attainment.
Methods
Serum concentrations of PSZ were collected retrospectively from records of hospitalized patients. A population PK analysis was performed in a nonlinear mixed-effects modeling framework with NONMEM (v7.4). The PK parameters were scaled to body weight, then potential covariate effects were assessed. The final PK model was used to evaluate recommended dosing schemes through simulation of target attainment (as a percentage of the population having steady-state trough concentrations above the recommended target) using Simulx (v2021R1).
Results
Repeated measurement data of 202 serum concentrations of total PSZ were acquired from 47 immunocompromised patients between 1 and 21 years of age receiving PSZ either intravenously or orally, or both. A one-compartment PK model with first-order absorption and linear elimination best fit the data. The estimated absolute bioavailability (95% confidence interval) for suspension (Fs) was 16% (8–27%), which was significantly lower than the reported tablet bioavailability (Ft) [67%]. Fs was reduced by 62% and 75% upon concomitant administration with pantoprazole (PAN) and omeprazole (OME), respectively. Famotidine resulted in a reduction of Fs by only 22%. Both fixed dosing and weight-based adaptive dosing provided adequate target attainment when PAN or OME were not coadministered with the suspension.
Conclusions
The results of this study revealed that both fixed and weight-based adaptive dosing schemes can be appropriate for target attainment across all PSZ formulations, including suspension. Additionally, covariate analysis suggests that concomitant proton pump inhibitors should be contraindicated during PSZ suspension dosing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Posaconazole (PSZ) is a triazole antifungal drug that has off-label use in children, and an oral suspension (OS) is preferred for this population. However, poor biopharmaceutical characteristics of the OS formulation leads to an unpredictable dose-exposure profile of PSZ in children, potentially risking therapeutic failure. |
Population pharmacokinetic (PK) analysis of PSZ leveraging therapeutic drug monitoring (TDM) records of hospitalized immunocompromised children, adolescents, and young adults revealed that PSZ bioavailability from OS is significantly reduced (up to 75%) during the concomitant use of gastric acid-reducing medications. |
Simulation results revealed that both fixed and weight-based adaptive dosing schemes are appropriate for target attainment purposes unless proton-pump inhibitors are coadministered with OS. |
1 Introduction
Invasive fungal disease (IFD) is a potentially life-threatening illness caused by opportunistic fungal infections in immunocompromised patients, both adults and children [1, 2]. Incidence rates of IFD suggest that patients with hematological malignancies and primary or secondary immunodeficiencies, solid organ or stem cell transplant recipients, or neonates born prematurely comprise the highest risk populations for opportunistic infection [3]. The most common species for IFD are Candida and Aspergillus, which are associated with considerable clinical mortality [4, 5]. It is recommended that at-risk patients be provided adequate prophylactic therapy with systemic antifungal medications.
Posaconazole (PSZ) is a broad-spectrum, second-generation triazole antifungal that has been approved for prophylaxis of invasive Aspergillus and Candida species for individuals 13 years of age and older. Apart from its prophylactic use, PSZ is also approved for the treatment of oropharyngeal candidiasis, including those refractory to itraconazole or fluconazole therapy [6]. In addition, its off-label use has been shown to be effective in IFD for both prophylactic (in children below the age of 13 years) [7] and treatment (in adolescents) [8] purposes. Antifungal activity of PSZ stems from inhibition of ergosterol biosynthesis (an essential component of fungal cell membrane), thereby disrupting fungal growth and preventing the progression of IFD [9].
Clinical pharmacokinetics (PK) of PSZ have been mostly characterized in adults [6, 10,11,12], with a few studies in children [13,14,15]. Following intravenous (IV) administration, PSZ demonstrated low clearance (6.5 L/h), a large volume of distribution (226 L), and a long half-life (approximately 24 h) in adults [6]. The drug is primarily eliminated via biliary excretion, as 66.3% of a radiolabeled IV dose was recovered unchanged in the feces, while the rest of the recovered dose (17.6%) was observed in urine and feces as metabolites, suggesting minor contribution of metabolism and renal excretion to overall clearance [6, 16, 17]. Currently, PSZ is available as a solution for IV infusion, oral suspension (OS), and delayed-release tablets (DRTs). Although two oral formulations are available for PSZ, they cannot be used interchangeably because of significant differences in their biopharmaceutical properties [13, 14]. The bioavailability of OS (Fs) is reported to be significantly lower than that of DRTs (Ft) in both adults and children [13, 18], although a new delayed-release OS has been approved in children with the goal of improving this limitation [19]. Furthermore, high variability in Fs has been reported under various circumstances that broadly modulate the intra-gastric pH, such as coadministration with acidic beverages, high-fat meals, proton pump inhibitors (PPIs; e.g., omeprazole [OME], pantoprazole [PAN]), and H2-receptor blockers (e.g. cimetidine), and also in the presence of diarrhea [13, 20, 21].
It has been shown that the therapeutic success of PSZ, for both prophylaxis and treatment, is linked to the ratio of its area under the plasma concentration–time curve (AUC) to the minimum inhibitory concentration (MIC) of the fungal strain [22]. In practice, given the limited feasibility in measuring AUC, target attainment is generally assessed based on trough concentration. The British Society for Medical Mycology has suggested target trough serum concentrations of 0.7 mg/L and 1.0 mg/L for prophylaxis and treatment of IFD, respectively, in order to avoid potential breakthrough infections or treatment failure due to subtherapeutic treatment [23]. However, given the low and variable Fs, there is a high level of concern whether the recommended targets can be achieved with PSZ suspension [7]. More importantly, given the potential safety concerns associated with IV administration of PSZ in children (based on safety studies in juvenile animals) [6], OS is the primary choice of treatment in young children who cannot swallow DRTs. On the other hand, OS is also preferred in critically ill adults with moderate to severe renal dysfunction because of the potential accumulation of sulfobutyl ether β-cyclodextrin [6], the main ingredient that solubilizes PSZ in the IV formulation. Therefore, the success of PSZ therapy against IFD in these special populations is largely limited by the lack of predictability in exposure following OS administration. While a clinical threshold for PSZ toxicity could not be identified yet, an upper limit of 3.75 mg/L for trough concentration is generally considered well tolerated [24].
The goal of this study was to characterize the population PK of PSZ for children, adolescents, and young adults in order to assess the performance of the currently recommended fixed and weight-based dosing schemes with regard to therapeutic target attainment.
2 Methods
2.1 Subjects and Data Collection
Serum concentrations of total PSZ, dosing information, patient characteristics, and routine laboratory measures were collected retrospectively from electronic health records (EHRs) of UNC Health between 2014 and 2019, which predates the use of the newly approved delayed-release OS for children. Included subjects were hospitalized patients 1–21 years of age receiving PSZ for the first time per standard of care. The PSZ concentration data represents the results of routine therapeutic drug monitoring (TDM), which were used as the basis for dose adjustments or switching to an alternative route or formulation in the inpatient hospital setting. This study was approved by the University of North Carolina at Chapel Hill Institutional Review Board (IRB).
2.2 Bioanalytical Method
Briefly, the serum concentrations were quantified at UNC Health McLendon Clinical Laboratories during TDM using a validated high-performance liquid chromatography-tandem mass spectrometry (HPLC-MS/MS) method. The analytes were extracted from serum by protein precipitation, which was followed by reverse-phase separation though a Waters Xbridge C18 (4.6 × 50 mm, 5 µm) chromatographic column using gradient elution technique with mobile phase A (2 mM ammonium acetate and 0.1% formic acid in LCMS grade water) and B (2 mM ammonium acetate and 0.1% formic acid in LCMS grade methanol) and analysis using Waters Quattro Micro API tandem mass spectrometer (Milford, MA, USA). The lower limit of quantitation (LLOQ) was 0.08 mg/L and adequate linearity was established (R2 = 0.9958) between 0.08 and 8.5 mg/L concentration range.
2.3 Population PK Model Development
Population PK analysis was performed in a nonlinear mixed effects modeling framework using the first-order conditional estimation with interaction (FOCEI) method implemented in the NONMEM® software version 7.4 (Icon PLC, Dublin, Ireland). Both one- and two-compartment models were evaluated as the structural model. Given the wide body size range in the pediatric population, allometric body weight was included a priori in the base model to scale clearance and volume of distribution. The allometric exponents were initially fixed to 0.75 and 1.00 for clearance and volume of distribution, respectively, and were also empirically estimated later. Between-subject variability (BSV) on the PK parameters was modeled using a lognormal distribution. The residual unexplained variance (RUV) on the observations was accounted for by a proportional error model. Other error models, including additive and combination (additive and proportional) models, were also considered during base model development.
Potential covariates were initially evaluated through a graphical examination, based on correlation between the empirical Bayesian estimates (EBEs) of the relevant PK parameter(s) from the base model and the potential covariates. Possible observed covariate effects during the graphical examination were considered, along with reported shrinkage estimates for each random effect and physiological plausibility. After the EBE-based evaluation, a stepwise covariate modeling process was implemented for plausible relationships, where the forward addition and backward deletion steps were based on a statistical significance level of p < 0.05 and p < 0.01, respectively (which correspond to the reduction in NONMEM objective function value > 3.84 and > 6.63, respectively, for one degree of freedom). Continuous covariates were evaluated using a power function by centering the individual covariates (covind) at their respective median (covmed) values, as shown in Eq. 1.
where TVθ represents the typical value of the population-level parameter \({\theta }_{\mathrm{pop}}\), and θcov represents the effect size.
Categorical covariates were modeled using a switch variable COV, as shown in Eq. 2, where COV = 0 or 1 in the absence and presence of the covariate, respectively.
The potential effect of age-related maturation on PSZ’s clearance was assessed by using a sigmoidal maturation function with respect to age, as shown in Eq. 3. Here, post-natal age (PNA) was used since gestational age was not available for calculation of post-menstrual age.
Where the typical value of the individual clearance is modified by the maturation factor (MF), which matures with PNA in years (AGE), reaching half of the fully mature value (θpop) when AGE is equal to PNA50 [25]. The Hill coefficient (Hill) was fixed to 1.
Similarly, the potential effect of PSZ dose on suspension bioavailability was also evaluated using an asymptotic model as shown in Eq. 4. Total (in milligrams [mg]), weight-normalized (in milligrams/kilogram [mg/kg]), and body surface area-normalized (in milligrams/meters squared [mg/m2]) doses were considered for this evaluation.
where the bioavailability from OS (Fs,i) decreases as the dose increases, reaching half of the maximal individual value (θpop) at DOSE50.
Covariates included in the final model were further evaluated for other criteria, such as BSV reduction, the precision of estimates, and, above all, biological plausibility and clinical relevance.
2.4 Model Evaluation
Standard goodness-of-fit plots were created using the ggplot2 package in R (R Foundation for Statistical Computing, Vienna, Austria), and were used for graphical evaluation of model fits. These included plots of observed concentrations (DV) versus both population predictions (PRED) and individual predictions (IPRED), conditional weighted residuals (CWRES) versus PRED, and individual fits (DV and IPRED over time). The final model was also evaluated by prediction-corrected visual predictive check (pcVPC) [26], non-parametric bootstrap analysis using 1000 replicates, which were performed in Perl Speaks NONMEM (PsN, version 4.7), and normalized prediction distribution errors (NPDEs) quantified by the R package npde [27].
2.5 Simulation of Target Attainment
Final model parameters were translated into a Simulx model file (Lixoft, Antony, France) to simulate concentration–time profiles. Covariate information (e.g. age, weight) were non-parametrically sampled (n = 1000 individuals per scenario) from the National Health and Nutrition Examination Survey (NHANES) database representing data from 1999 to 2016 (n = 15,600) in order to generate virtual target populations for simulation [28]. Target populations were selected based on the age makeup of individuals within the dataset receiving each formulation. In order to assess off-label administration of PSZ only, target populations for oral dosing were limited to children below the age of 13 years, and intravenous dosing was limited to children and adolescents below 18 years of age. In order to simulate adaptive dosing, the R package RsSimulx (R speaks Simulx) was used to implement dose adjustments after steady-state trough serum concentration measurement. Target attainment values were reported as percentages of the total virtual population for initial steady-state measurements after fixed-rate and weight-based dosing as well as post-adjustment steady-state measurements for weight-based simulations.
Initially, simulations were exclusively performed to evaluate the fixed prophylactic dosing schemes, recommended in the Noxafil™ label [6] as 200 mg three times daily for OS and 300 mg daily for DRT and IV formulations after two 300 mg loading doses on day 1. The simulation of fixed-rate doses did not include any dose adjustments (i.e., a purely non-adaptive dosing). In subsequent simulations, the additional influence of dose adaptation was also assessed by considering the local dosing guideline at UNC Health that recommends adaptive dosing based on initial TDM results 1 week after initiation of weight-based dosing (electronic supplementary material [ESM] Table S1). At UNC Health, dose adjustments are accomplished by sampling the trough concentration after 7 days of dosing, which is a typical occasion for TDM sampling, and applying a one-time proportional dosage increase or decrease by 25–50% (of the initial dose) for all subsequent doses, if the trough level is outside the recommended target range for TDM. The recommended target trough ranges for TDM are 0.7–3.75 mg/L and 1.0–3.75 mg/L for prophylaxis and treatment, respectively, and thus these ranges were set as targets for the adaptive dosing simulations [23, 24].
As per clinical practice, the initial dose was calculated in mg/kg of weight then capped at 400 mg and 300 mg for OS and DRTs, respectively, for individual doses exceeding those upper limits. However, no cap was applied for the successive doses that were increased (from the respective initial dose) due to dose adjustment based on a lower simulated trough level than the target range. To represent clinical reality as closely as possible, all simulated DRT doses were administered as 100 mg (i.e., the lowest tablet strength) or a multiple by rounding to the nearest 100 for both the initial dose (that includes mg/kg calculations with capping) and adaptive dose (that accounts for dose adjustments). In addition, OS dosing in children receiving concomitant PPIs or famotidine (as an H2-receptor antagonist, or H2RA) were simulated to demonstrate their respective effects on PSZ concentrations. In the former, either OME or PAN were randomly assigned to the same individuals who were used for simulation of the OS formulation, and, in the latter, every individual received famotidine.
3 Results
3.1 Subjects and Data
In total, 48 hospitalized patients provided 215 serum PSZ concentrations through their EHR. The number of repeated observations per subject ranged from 1 to 27, with a median per-subject count of 2. Observations of total PSZ concentration were collected as standard of care TDM samples. Generally, all samples were collected as troughs prior to the next dose per standard of care, however the dosing intervals were not uniform for any formulation. Of 215 collected serum concentrations, nine lacked dosing records immediately preceding the recorded serum concentration and were excluded. One subject with four observations was excluded from the modeling process for unusually high concentrations given similar dosages in other individuals (both in mg and mg/kg), two of which were more than threefold higher than the next highest observation from the other patients at similar times post-dose. Two observations were below the LLOQ and were replaced with LLOQ/2 or 0.04 mg/L. Modeling was performed using the remaining 202 observations from 47 individuals.
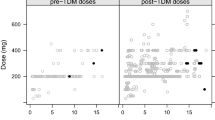
Patient characteristics, their laboratory variables, and dosing information are shown in Table 1. Three patients reported serum concentrations for both IV and OS formulations, representing 17/202 total observations. Four patients reported serum concentrations for both IV and DRT administration, representing 53/202 total observations. No subjects received all three formulations in their included dosing history. Of 202 utilized observations, 49 were taken after the administration of OS and 123 were taken after the administration of DRTs. The distribution of dose-normalized concentrations (by total daily dose) for each formulation is shown in a violin plot (Fig. 1) to demonstrate differential dose-exposure observed within the dataset for OS compared with DRTs and IV administration. Overall target attainment is visualized in a formulation-specific concentration–time after last dose plot (ESM Fig. S1).
Violin plot of observed PSZ plasma concentrations stratified by formulation and normalized to total daily dose, calculated as the observed concentration, in milligrams per liter, divided by the total dose, in milligrams, administered within the previous 24 h. The width of each shape is determined by the frequency of observed plasma concentrations along the y-axis under a particular formulation. Data are not necessarily at steady state. Number of observations incorporated into each shape: suspension, 49; tablet, 123; IV, 30. PSZ posaconazole, IV intravenous, conc. concentration
Continuous covariates available for each individual included age, weight, body mass index (BMI) and percentile (BMI%), estimated glomerular filtration rate (eGFR), serum albumin (ALB), alkaline phosphatase (ALP), alanine aminotransferase (ALT), aspartate aminotransferase (AST), and total bilirubin. Categorical covariates available included sex, obesity status, and administration of comedications. Concomitant use of PPIs and famotidine (as an H2RA) was reported in 21 and 34 subjects, respectively. Observations after OS with PPIs or famotidine represented 18 and 13 of 49 total post-OS serum concentrations, respectively. Of three PPIs reported, esomeprazole (ESO) was only administered to one subject and was not modeled separately from OME. Dose levels of ESO, OME, PAN, and famotidine were available but were not used for modeling.
3.2 Base Model
A one-compartment model with proportional error resulted in the most plausible parameter estimates. Although PSZ demonstrates a biphasic concentration profile in serum following an intravenous dose [29], a two-compartment model was not supported by the limited sparse dataset. The timing of observed serum concentrations post-dose was also limited in terms of covering the absorption phase of PSZ, which led to fixing of the first-order absorption rate constants (Ka) to previously published population PK estimates of 0.325 h−1 and 0.588 h−1 for OS and DRT formulations, respectively [11, 14]. Furthermore, these limitations also led to fixing the absolute bioavailability and lag time for the DRT formulation to 0.67 and 2.5 h, respectively, based on previous reported values [12, 30]. Of note, a lag time was not biologically relevant for the OS, since the suspension is considered an immediate-release formulation.
3.3 Covariate Analysis and Final Model Diagnostics
Analysis of the first stepwise addition phase and selected additional steps are shown in ESM Table S2. The addition of PPIs/H2RA and ALP were conducted in that order, although no additional covariate relationships reached the forward inclusion threshold. Due to the limited number of additions, the results of the backward elimination phase are identical to the monovariate additions shown in ESM Table S2. No pattern was observed in estimated OS bioavailability with increasing suspension dose shown in ESM Fig. S2. Additional EBE visualizations from the base model are provided for the remaining covariates in the ESM (ESM Fig. S2). The effect of age groups on clearance and body surface area normalized dose on Fs represents covariates considered but not included for step 1 covariate addition analysis due to similar or implausible effects. The effects of PPIs and famotidine on Fs were identified as significant after the backward elimination step. The effect of PPIs on bioavailability appeared more influential than famotidine. Among PPIs, OME and PAN reduced the absolute bioavailability of OS by approximately 75% and 62%, respectively, whereas famotidine caused a 22% reduction. Each chosen covariate effect was well-estimated, with a percentage relative standard error (%RSE) of values ranging from 23.6 to 32.7%.
Base and final model parameter estimates, including the parameter precision reported as the %RSE, are shown in Table 2. BSV was considered for clearance, volume of distribution, and Fs. The population estimate of clearance was 6.00 L/h for a 70 kg individual (bootstrap 95% confidence interval [CI] of 4.2–8.0 L/h), with an estimated BSV of 42% (as CV%, shrinkage estimate of 16%). Volume of distribution was similarly variable, with an estimated 50% BSV (shrinkage estimate of 55%) on the population estimate (95% CI) of 146 L for a 70 kg individual (76–327 L). The final model estimate of Fs (95% CI) was 16.5% (8–27%). Importantly, the inclusion of acid-reducing drugs (as covariates on Fs) significantly reduced the BSV estimate to 49% (shrinkage estimate of 58%) from 72% in the base model, which further supported the inclusion of this covariate effect. Generally, final model parameter estimates demonstrated acceptable precision. Standard graphical evaluations appeared reasonable (Fig. 2), and a pcVPC of the final model did not present any obvious model misspecification, although large imprecision was observed due to limited observations after IV dosing (ESM Fig. S3). The distribution of errors from 500 simulated datasets is shown in ESM Fig. S4 as NPDE graphs and statistical tests. The p values for the t test, Fisher variance test, and Shapiro–Wilk test were 0.798, 0.004, and 0.04, respectively.
Graphical evaluation of the final model. a Population predictions versus observed concentrations. b Individual predictions versus observed concentrations. c Conditional weighted residuals versus population predictions. Dashed gray lines represent the line of unity in a, b, but represents ± 2 in panel c. Dashed red lines represent trends in the data points (black circles) using linear (a, b) or loess (c) smoothing with the geom_smooth function in R. conc. concentration
3.4 Simulation of Target Attainment
Age and weight demographics utilized for dosing simulations of each formulation are shown in ESM Table S3. Simulated concentration–time plots representing target populations for each formulation are shown for label-based fixed dosing (Fig. 3) and UNC Health-derived adaptive, weight-based dosing (Fig. 4). All label-based dosing schemes for IV, OS and DRTs provided considerable target attainment within each respective target population. Among the local dosing schemes, initial OS dosing of 6 mg/kg and 8 mg/kg, both three times daily, were deemed sufficient for prophylaxis and treatment, respectively, within the target population of children under the age of 13 years. Dosing the DRT at 8 mg/kg once daily after a twice-daily loading dose for prophylaxis and 6 mg/kg twice daily for treatment provided adequate target attainment in children between 6 and 12 years of age. For the intravenous route, 90-min, once-daily infusions after a twice-daily loading dose were appropriate at 6 mg/kg per infusion for prophylaxis and 10 mg/kg per infusion for treatment in a target population consisting of both children and adolescents. Target attainment for each dosing scheme and dose adjustments for weight-based dosing are shown in Table 3. Dose adjustments of 25% up to 50% improved target attainment for DRTs, IV, and OS dosing, although concomitant PPI use still prevented adequate exposure in the OS simulations after adaptive dose increases. Concomitant use of famotidine with OS dosing demonstrated slightly lower target attainment than monotherapy, although PK targets were readily achievable with dosing adjustments, given the adaptive dosing scheme (ESM Fig. S5). Increasing daily dose numbers (i.e., daily dosing to twice daily) were not evaluated as a dose-adjustment scheme.
Simulated concentration–time curves for each formulation, given label-recommended fixed dosing. a Oral suspension administered to individuals 2–12 years of age. b Delayed-release tablet administered to individuals aged 6–12 years. c Intravenous infusions administered to individuals aged 2–17 years. Gray dotted lines indicate target trough concentration ranges for prophylaxis of 0.7–3.75 mg/L. conc. concentration
Simulated concentration–time curves of the virtual population for each formulation and indication. a Oral suspension without comedication administered to individuals 2–12 years of age. b Oral suspension with PPI use, either omeprazole or pantoprazole, administered randomly to the same population as (a). c Delayed-release tablet administered to individuals 6–12 years of age. d Intravenous infusions of 90 min administered to individuals 2–17 years of age. Gray dotted lines indicate target trough concentration ranges (0.7–3.75 mg/L for prophylaxis, left column, or 1.0–3.75 mg/L for treatment, right column). Black arrows represent the sampling time at 168 h used to determine if dose adjustment is necessary for each individual virtual subject. If necessary, all doses after 168 h were given a one-time adjustment of the indicated percentage, either increasing or decreasing. Unless noted, dose adjustments were set to 25%. conc. concentration, PPI proton pump inhibitor
4 Discussion
This study characterized the population PK of PSZ in pediatric, adolescent, and young adult patients receiving the available IV and oral formulations by utilizing available real-world data. Simultaneous IV/oral modeling allowed for the estimation of the absolute bioavailability of the OS, which has not been previously well characterized. The final model accurately predicted PSZ concentrations across a wide range of doses within a diverse population of children, using body weight as the primary scaler of PK. Simulation results revealed that the currently approved fixed dosing for prophylaxis [6] is adequate to achieve the therapeutic target against breakthrough IFD without the need for additional dose adjustments. Additionally, an alternative (local) dosing guideline proposed by UNC Health that accounts for adaptive dosing based on TDM, also appeared adequate for the purpose of target attainment in the target off-label pediatric populations (i.e., < 13 years and < 18 years for oral and IV formulations, respectively). Simulations using this alternative adaptive dosing scheme also revealed that a dose increment of 25–50% (of the starting dose) upon a low trough level at 1 week would further improve the target attainment in most situations. However, target attainment is unlikely during concomitant use of PPIs, but not famotidine, in younger children who receive the currently available PSZ suspension formulation, even after applying the adaptive dosing strategy, which poses a serious concern regarding the continued use of PPIs in hospitalized children at risk of invasive fungal infection.
Estimates of clearance for an adult individual are similar between previously published parameter estimates and the model value for a 70 kg individual from this study (6.5 L/h and 6.0 L/h) [31]. The volume of distribution for a 70 kg individual was estimated to be nearly 150 L, which is somewhat lower than the previously published average value of 226 L for adults, but still falls into the class of highly distributed drugs (i.e., substantially higher than total body water volume), as expected for PSZ given its high lipophilicity (LogP = 4.6). Previously reported apparent PK parameters in hospitalized children are highly variable, although estimates from this study lie within the range of published values (ESM Table S4). Direct comparison of reported apparent values and calculated oral parameters is considered appropriate because our estimates of bioavailability are in line with previously published values in adults (fixed value for DRTs, and 16.5% compared with a range of 8–47% for OS) [30, 32]. While extensive distribution is likely to be underpinned by multicompartmental distribution, there was limited opportunity to consider that in this modeling work given the TDM data were not informative enough for that purpose. Instead, a one-compartment model was able to precisely estimate clearance, volume of distribution, and bioavailability parameters along with associated variabilities, which was considered fit for the purpose of predicting steady-state exposure of PSZ. While this dataset included multiple hospital stays for several individuals, estimation of individual interoccasion variability (IOV) did not improve the model fit (results not shown) and thus was not included in the final model. The estimates of BSV for clearance, volume of distribution, and Fs were 42%, 50%, and 49%, respectively. In a previously published meta-analysis [33], a 40% BSV was identified as the nominal variability on PK parameters (while 20% and 60% were identified as low and high BSV), which implies that selected covariates in the final model could adequately account for BSV on these PK parameters. However, there are a few more known causes of BSV for the PK of PSZ, particularly Fs, such as diarrhea and fed/fasted state, which could not be accounted for in the model as that information was not recorded in the EHR. This would have further reduced the BSV estimates of the final model.
The most widely reported factor affecting PSZ exposure is the concomitant use of PPIs or H2RAs, both of which were identified by the model as significant predictors of OS bioavailability. In healthy adults, PPIs have been shown to reduce maximal serum concentration of PSZ after OS dosing by around 46% [20]. In children, one population PK analysis estimated a 42% reduction in OS bioavailability during concomitant PPI administration (and no or limited effect of H2RAs), while another study reported a significant decline in target attainment percentage while receiving both OS and PPIs [13, 34], which are similar if not somewhat reduced effects compared with our study results. These findings of heavily reduced suspension bioavailability of PSZ are underpinned by its poor solubility, solubility rate-limited absorption (i.e., Biopharmaceutical Classification System [BCS] class II), and, most importantly, its pH-dependent solubility (i.e., reduced solubility at elevated gastric pH) that have been extensively characterized in the literature [35]. Of note, a similar clinically relevant effect of acid-reducing drugs on bioavailability is well known for a few other BCS class II drugs (e.g. atazanavir), which also have the issue of pH-dependent solubility [36]. While the effect of acid-reducing agents on PSZ bioavailability was reported in previous studies, it was not clear whether the magnitude of change in bioavailability is different between PPIs and H2RAs. This study has addressed the question, as the final model could estimate the effects of PPIs and H2RAs (famotidine) separately, where the latter has a less intense effect on bioavailability. This could be due to the fact that H2RAs (e.g., famotidine) reversibly inhibit a subset of the gastric acid production pathway compared with PPIs, which irreversibly bind proton pumps in the common pathway [37, 38].
Apart from body weight and acid-reducing drugs, no other tested variables, including patient characteristics and laboratory measures, were included in the model due to the lack of significance and/or plausibility. ALB has been reported as a significant covariate of PSZ’s total clearance in adults, where a decrease in albumin at a given BMI would result in lower total PSZ trough concentrations at the same dose [39], which is an anticipated effect for such a highly protein bound drug with < 2% free fraction in plasma [6]. However, ALB did not improve the model fit to a statistically significant extent in the current analysis (ΔOFV = 0.0), which could be due to a low representation of moderate to severe hypoalbuminemic patients in this dataset (14.5% of individuals with at least one measure < 2 g/dL ALB). On the other hand, ALP was a statistically significant covariate on clearance (ΔOFV = − 5.8) in this analysis, although the causation of this effect was not clear and the reported positive relationship between increasing ALP and clearance is not necessarily believable given the small number of individuals at the higher range of the reported ALP concentration; thus, it was not included in the model. Of note, given the involvement of hepatobiliary process in the elimination of PSZ, influence of a liver function marker (ALP) on its clearance cannot be entirely refuted, but more mechanistic insight and empirical evidence would be needed to confirm its effect on the pharmacokinetics of PSZ. Age-related changes to clearance were evaluated by sigmoidal maturation function due to the potential maturation of metabolic and/or possible active transport proteins [17], although the model was unable to estimate a feasible value for PNA50. Empirical estimation of clearance by age group was not considered plausible during EBE analysis and was not explored further, while estimation of the effect of age as a power function did not provide any improvement to model prediction. Previously reported effects of age on PK were limited to adults over the age of 50 years and were not relevant for pediatric modeling [40]. Finally, dose-dependent bioavailability of the OS was reported in a study population with a dose range of 2.5–49 mg/kg [12]. Our dataset did not include any oral dosing > 16 mg/kg, which is the most likely reason that effect of dose on OS bioavailability did not result in a statistical significance in this analysis (ΔOFV = − 2.6).
While retrospectively collected EHR data can be less accurate regarding sampling times, the authors believe that the dataset represents adequate quality to pursue population modeling in this understudied population after thorough exploratory data analysis and comparison with previous studies. Steps such as fixing absorption characteristics and including a lag time for the DRTs were necessary to support the estimation of parameters that the dataset would appropriately inform, including clearance, volume of distribution, and Fs. However, there are some limitations to our approach. TDM sampling comprising mostly trough samples may have prevented reliable estimation of the absorption parameters Ka and ALAG (lag time), instead utilizing fixed literature values reported in both adults and children. Estimation of Fs was reliant on observations from only three pediatric subjects, which may limit generalizability of the population estimate to additional populations, although the authors believe that estimation of this value is vital for understanding pediatric PK for PSZ even using limited data. The limited oral dose range prevented more complex absorption modeling, such as dose-related changes to Fs, which has an additional effect of preventing estimation of an effective OS dose above the maximum observed single dose (600 mg). Bioavailability has been observed to be dose-limited in both adults (up to 800 mg/dose) [41] and children (up to 700 mg/dose) [13, 14], although a full exploration of nonlinearity, as well as additional dose-limiting factors such as palatability, has not been conducted. The target serum concentrations for TDM have been suggested by the British Society of Medical Mycology and supported by a previous retrospective analysis study in Chinese children [34]. These are general guidelines for maximizing prophylaxis and treatment efficacy, and thus the target attainment analysis does not guarantee favorable outcomes (prevention of breakthrough infections or complete cure of IFD) in all cases, especially in instances of drug-resistant pathogens. This study did not seek to estimate dose-dependent changes in clearance that have been previously reported in adults, however the dose range represented in our study falls within the reported linear range [31]. There is a possibility of involvement of an age-related maturation process in the hepatobiliary elimination pathway of PSZ (affecting clearance), however, the current data were probably not informative enough to confirm or refute this potential effect on CL. A physiologically based model that can account for these factors in a bottom-up manner (i.e., not dependent on data or design) would be an appropriate way to further investigate these effects in children.
5 Conclusions
This study leveraged real-world data to characterize the population PK of PSZ in pediatric patients, and characterized the differential effects of PPIs and H2RA as separate classes of acid-reducing drugs on the absolute bioavailability of PSZ suspension (Fs reductions of 62–75% for PPIs and 22% for H2RA). This study also confirmed the effectiveness of the recommended dosing schemes, both adaptive and non-adaptive, in achieving the required therapeutic target based on trough serum concentrations. Importantly, concomitant PPI administration during PSZ OS dosing should be reconsidered as it greatly reduces the likelihood of target attainment even after adaptive dosing is implemented. Despite the limitation of TDM data, such as unbalanced sampling, sparseness, incomplete and missing covariate records, etc., this study has leveraged valuable real-world information and provided useful guidance for dosing and dose adjustment of PSZ in immunocompromised children.
References
Warnock DW. Trends in the epidemiology of invasive fungal infections. Nippon Ishinkin Gakkai Zasshi. 2007;48(1):1–12. https://doi.org/10.3314/jjmm.48.1.
Singh N. Trends in the epidemiology of opportunistic fungal infections: predisposing factors and the impact of antimicrobial use practices. Clin Infect Dis. 2001;33(10):1692–6. https://doi.org/10.1086/323895.
Pana ZD, Roilides E, Warris A, Groll AH, Zaoutis T. Epidemiology of invasive fungal disease in children. J Pediatr Infect Dis Soc. 2017;6(Suppl 1):S3–11. https://doi.org/10.1093/jpids/pix046.
Zaoutis TE, Heydon K, Chu JH, Walsh TJ, Steinbach WJ. Epidemiology, outcomes, and costs of invasive aspergillosis in immunocompromised children in the United States, 2000. Pediatrics. 2006;117(4):e711–6. https://doi.org/10.1542/peds.2006-1161.
Cleveland AA, Harrison LH, Farley MM, Hollick R, Stein B, Chiller TM, Park BJ. Declining incidence of candidemia and the shifting epidemiology of Candida resistance in two US metropolitan areas, 2008–2013: results from population-based surveillance. PLoS ONE. 2015;10(3):e0120452. https://doi.org/10.1371/journal.pone.0120452.
US FDA. Posaconazole [package insert]. Revised 11/2015. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/022003s018s020,0205053s002s004,0205596s001s003lbl.pdf. Accessed 29 Jun 2022.
Vicenzi EB, Calore E, Decembrino N, Berger M, Perruccio K, Carraro F, Cesaro S. Posaconazole oral dose and plasma levels in pediatric hematology-oncology patients. Eur J Haematol. 2018;100(3):315–22. https://doi.org/10.1111/ejh.13017.
Cornely OA, et al. Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med. 2007;356(4):348–59. https://doi.org/10.1056/NEJMoa061094.
Keating GM. Posaconazole. Drugs. 2005;65(11):1553–67. https://doi.org/10.2165/00003495-200565110-00007.
Dolton MJ, Brüggemann RJ, Burger DM, McLachlan AJ. Understanding variability in posaconazole exposure using an integrated population pharmacokinetic analysis. Antimicrob Agents Chemother. 2014;58(11):6879–85.
Petitcollin A, Boglione-Kerrien C, Tron C, Nimubona S, Lalanne S, Lemaitre F, Verdier MC. Population pharmacokinetics of posaconazole tablets and Monte Carlo simulations to determine whether all patients should receive the same dose. Antimicrob Agents Chemother. 2017;61(11):e01166-17.psz-e1217. https://doi.org/10.1128/AAC.01166-17. (DRT bioavailability reference).
van Iersel ML, Rossenu S, de Greef R, Waskin H. A population pharmacokinetic model for a solid oral tablet formulation of posaconazole. Antimicrob Agents Chemother. 2018;62(7):e02465-e2517. https://doi.org/10.1128/AAC.02465-17.
Boonsathorn S, et al. Clinical pharmacokinetics and dose recommendations for posaconazole in infants and children. Clin Pharmacokinet. 2019;58(1):53–61. https://doi.org/10.1007/s40262-018-0658-1.
Elkayal O, et al. A population pharmacokinetic modeling and simulation study of posaconazole oral suspension in immunocompromised pediatric patients: a short communication. Ther Drug Monit. 2021;43(4):512–8. https://doi.org/10.1097/FTD.0000000000000877.
Vanstraelen K, Colita A, Bica AM, Mols R, Augustijns P, Peersman N, Spriet I. Pharmacokinetics of posaconazole oral suspension in children dosed according to body surface area. Pediatr Infect Dis J. 2016;35(2):183–8. https://doi.org/10.1097/INF.0000000000000963.
Blennow O, Eliasson E, Pettersson T, Pohanka A, Szakos A, El-Serafi I, Hassan M, Ringdén O, Mattsson J. Posaconazole concentrations in human tissues after allogeneic stem cell transplantation. Antimicrob Agents Chemother. 2014;58(8):4941–3. https://doi.org/10.1128/AAC.03252-14.
Krieter P, Flannery B, Musick T, Gohdes M, Martinho M, Courtney R. Disposition of posaconazole following single-dose oral administration in healthy subjects. Antimicrob Agents Chemother. 2004;48(9):3543–51. https://doi.org/10.1128/AAC.48.9.3543-3551.2004.
Guarascio AJ, Slain D. Review of the new delayed-release oral tablet and intravenous dosage forms of posaconazole. Pharmacother J Hum Pharmacol Drug Ther. 2015;35(2):208–19.
Groll AH, Abdel-Azim H, Lehrnbecher T, Steinbach WJ, Paschke A, Mangin E, Bruno CJ. Pharmacokinetics and safety of posaconazole intravenous solution and powder for oral suspension in children with neutropenia: an open-label, sequential dose-escalation trial. Int J Antimicrob Agents. 2020;56(3):106084.
Krishna G, Moton A, Ma L, Medlock MM, McLeod J. Pharmacokinetics and absorption of posaconazole oral suspension under various gastric conditions in healthy volunteers. Antimicrob Agents Chemother. 2009;53(3):958–66. https://doi.org/10.1128/AAC.01034-08.
Merck & Co. 2022. Noxafil US prescribing information, revised September 2022. https://www.merck.com/product/usa/pi_circulars/n/noxafil/noxafil_ppi.pdf. Accessed 29 Jun 2022.
Andes D, Marchillo K, Conklin R, Krishna G, Ezzet F, Cacciapuoti A, Loebenberg D. Pharmacodynamics of a new triazole, posaconazole, in a murine model of disseminated candidiasis. Antimicrob Agents Chemother. 2004;48(1):137–42.
Ashbee HR, Barnes RA, Johnson EM, Richardson MD, Gorton R, Hope WW. Therapeutic drug monitoring (TDM) of antifungal agents: guidelines from the British Society for Medical Mycology. J Antimicrob Chemother. 2014;69(5):1162–76. https://doi.org/10.1093/jac/dkt508.
Cornely OA, Duarte RF, Haider S, Chandrasekar P, Helfgott D, Jiménez JL, Waskin H. Phase 3 pharmacokinetics and safety study of a posaconazole tablet formulation in patients at risk for invasive fungal disease. J Antimicrob Chemother. 2016;71(3):718–26. https://doi.org/10.1093/jac/dkv380.
Anderson BJ, Holford NH. Mechanistic basis of using body size and maturation to predict clearance in humans. Drug Metab Pharmacokinet. 2009;24(1):25–36.
Bergstrand M, Hooker AC, Wallin JE, Karlsson MO. Prediction-corrected visual predictive checks for diagnosing nonlinear mixed-effects models. AAPS J. 2011;13(2):143–51. https://doi.org/10.1208/s12248-011-9255-z.
Comets E, Brendel K, Mentré F. Computing normalised prediction distribution errors to evaluate nonlinear mixed-effect models: the npde add-on package for R. Comput Methods Programs Biomed. 2008;90(2):154–66.
Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/nhanes/index.htm. Accessed 25 Oct 2019.
European Medicines Agency. Posaconazole injection assessment report: EPAR-assessment report-Variation. 2014. https://www.ema.europa.eu/en/documents/variation-report/noxafil-h-c-610-x-0033-epar-assessment-report-variation_en.pdf. Accessed June 2022.
Jansen AM, Muilwijk EW, Van Der Velden WJ, Maertens JA, Aerts R, Colbers A, Brüggemann RJ. Posaconazole bioavailability of the solid oral tablet is reduced during severe intestinal mucositis. Clin Microbioland Infect. 2022;28(7):1003–9. https://doi.org/10.1016/j.cmi.2022.01.029
Kersemaekers WM, van Iersel T, Nassander U, O’Mara E, Waskin H, Caceres M, van Iersel ML. Pharmacokinetics and safety study of posaconazole intravenous solution administered peripherally to healthy subjects. Antimicrob Agents Chemother. 2015;59(2):1246–51.
Lipp HP. Clinical pharmacodynamics and pharmacokinetics of the antifungal extended-spectrum triazole posaconazole: an overview. Br J Clin Pharmacol. 2010;70(4):471–80.
Al-Sallami HS, Cheah SL, Han SY, Liew J, Lim J, Ng MA, et al. Between-subject variability: should high be the new normal? Eur J Clin Pharmacol. 2014;70(11):1403–4.
Jia M, Zhang Q, Qin Z, Wang D, Liu P, Yang J, et al. Dose optimisation of posaconazole and therapeutic drug monitoring in pediatric patients. Front Pharmacol. 2022;13:833303. https://doi.org/10.3389/fphar.2022.833303.
Walravens J, Brouwers J, Spriet I, Tack J, Annaert P, Augustijns P. Effect of pH and comedication on gastrointestinal absorption of posaconazole. Clin Pharmacokinet. 2011;50(11):725–34.
Shugg T, Powell NR, Marroum PJ, Skaar TC, Younis IR. Evaluation of US Food and Drug Administration drug label recommendations for coadministration of antivirals and acid-reducing agents. Clin Pharmacol Ther. 2022;112(5):1088–97.
Nugent CC, Falkson SR, Terrell JM. H2 Blockers (updated 13 Feb 2022). Treasure Island, FL: StatPearls Publishing; 2022. https://www.ncbi.nlm.nih.gov/books/NBK525994/. Accessed 13 Nov 2022.
Welage LS. Overview of pharmacologic agents for acid suppression in critically ill patients. Am J Health Syst Pharm. 2005;62(10 Suppl 2):S4–10.
Sime FB, Byrne CJ, Parker S, Stuart J, Butler J, Starr T, et al. Population pharmacokinetics of total and unbound concentrations of intravenous posaconazole in adult critically ill patients. Crit Care. 2019;23(1):1–12.
Kohl V, Muller C, Cornely OA, Abduljalil K, Fuhr U, Vehreschild JJ, et al. Factors influencing pharmacokinetics of prophylactic posaconazole in patients undergoing allogeneic stem cell transplantation. Antimicrob Agents Chemother. 2010;54(1):207–12.
Ezzet F, Wexler D, Courtney R, Krishna G, Lim J, Laughlin M. Oral bioavailability of posaconazole in fasted healthy subjects: comparison between three regimens and basis for clinical dosage recommendations. Clin Pharmacokinet. 2005;44:211–20.
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, et al. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009;20(3):629–37. https://doi.org/10.1681/ASN.2008030287.
Acknowledgements
The authors would like to acknowledge Phillip Bates (McLendon Clinical Laboratories Special Chemistry Lab) and Nichole Korpi-Steiner (Department of Pathology and Laboratory Medicine, UNC Health) for their assistance with the measurement of the PSZ concentrations and the description of the bioanalytical method. They would also like to acknowledge Dr. Joseph Standing for his review of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Authors’ contributions
Acquired and formatted clinical data: WSW, CJM, LMG, JS. Designed the research: SM, JS, WSW, DG. Performed the data analysis: SM, JS. Wrote or contributed to the writing of the manuscript: SM, JS, WSW, CJM, LMG, DG.
Funding
DG receives salary support for research from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD096435 and R01HD102949). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest/competing interests
Sean McCann, Jaydeep Sinha, William S. Wilson, Cameron J. McKinzie, Lauren M. Garner, and Daniel Gonzalez have no relevant conflicts of interest to disclose.
Ethics approval
The data collection and population modeling research for this study was approved by the IRB at the University of North Carolina at Chapel Hill.
Consent to participate
A waiver of informed consent was granted by the IRB at the University of North Carolina at Chapel Hill.
Consent to publish
Not applicable.
Code availability
Code utilized in this manuscript for NONMEM®, and dose adjustments in R using RSSimulx, is provided in the ESM.
Data availability
The dataset analyzed during the current study is available from DG on reasonable request.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
McCann, S., Sinha, J., Wilson, W.S. et al. Population Pharmacokinetics of Posaconazole in Immune-Compromised Children and Assessment of Target Attainment in Invasive Fungal Disease. Clin Pharmacokinet 62, 997–1009 (2023). https://doi.org/10.1007/s40262-023-01254-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-023-01254-2