Abstract
Objective
To study the pharmacokinetics of micafungin in intensive care patients and assess pharmacokinetic (PK) target attainment for various dosing strategies.
Methods
Micafungin PK data from 20 intensive care unit patients were available. A population-PK model was developed. Various dosing regimens were simulated: licensed regimens (I) 100 mg daily; (II) 100 mg daily with 200 mg from day 5; and adapted regimens 200 mg on day 1 followed by (III) 100 mg daily; (IV) 150 mg daily; and (V) 200 mg daily. Target attainment based on a clinical PK target for Candida as well as non-Candida parapsilosis infections was assessed for relevant minimum inhibitory concentrations [MICs] (Clinical and Laboratory Standards Institute). Parameter uncertainty was taken into account in simulations.
Results
A two-compartment model best fitted the data. Clearance was 1.10 (root square error 8%) L/h and V 1 and V 2 were 17.6 (root square error 14%) and 3.63 (root square error 8%) L, respectively. Median area under the concentration–time curve over 24 h (interquartile range) on day 14 for regimens I–V were 91 (67–122), 183 (135–244), 91 (67–122), 137 (101–183) and 183 (135–244) mg h/L, respectively, for a typical patient of 70 kg. For the MIC/area under the concentration–time curve >3000 target (all Candida spp.), PK target attainment was >91% on day 14 (MIC 0.016 mg/L epidemiological cut-off) for all of the dosing regimens but decreased to (I) 44%, (II) 91%, (III) 44%, (IV) 78% and (V) 91% for MIC 0.032 mg/L. For the MIC/area under the concentration–time curve >5000 target (non-C. parapsilosis spp.), PK target attainment varied between 62 and 96% on day 14 for MIC 0.016.
Conclusions
The licensed micafungin maintenance dose results in adequate exposure based on our simulations with a clinical PK target for Candida infections but only 62% of patients reach the target for non-C. parapsilosis. In the case of pathogens with an attenuated micafungin MIC, patients may benefit from dose escalation to 200 mg daily. This encourages future study.
Similar content being viewed by others
A population pharmacokinetic model of micafungin in critically ill patients greatly assists in applying simulations to derive pharmacokinetic target attainment. |
Current micafungin dosing regimens are adequate to treat Candida infections with species up to 0.016 mg/L but the dose should be increased to 200 mg in the case of minimum inhibitory concentrations ≥0.032 mg/L. |
Irrespective of the susceptibility of the species, a loading dose will lead to early higher exposure. |
1 Introduction
Candida or Aspergillus species are the fourth most dominant pathogens causing disease complication in the intensive care unit (ICU) and account for approximately 20% of infections in the ICU [1, 2]. Micafungin is an antifungal agent belonging to the class of echinocandins that act by inhibiting the synthesis of β-(1,3)-d-glucan, an important component of the fungal cell wall. It is a semi-synthetic compound, freely soluble in water and it has a molecular weight of 1292.26 [3, 4]. Micafungin shows in vitro and in vivo activity against Candida species and it is licensed as a first-line treatment for invasive candidiasis [3–5]. Micafungin, like other echinocandins, achieves adequate clinical responses in about 70% of patients with invasive candidiasis or candidaemia [2, 6].
The recommended micafungin dose is a daily (QD) intravenous infusions of 100 mg (infusion time approximately 1 h) [4]. In the case of insufficient response, such as when the clinical condition does not improve or in case of persistent positive cultures, the dose may be increased to 200 mg QD [4].
Recently, we analysed the pharmacokinetics of micafungin in 20 critically ill patients (ICU patients) by means of a non-compartmental approach [7]. A lower total exposure [area under the concentration–time curve over 24 h (AUC0–24h)] was observed in this cohort as compared with healthy volunteers, although the total exposure was comparable to other patient populations [7].
The pharmacodynamic (PD) index of the echinocandins is best described by the area under the concentration–time curve:minimum inhibitory concentration (AUC:MIC) ratio [8, 9]. To design optimal dosing regimens for micafungin in critically ill patients, both pharmacokinetic (PK) and PD factors need to be incorporated into a model. A non-compartmental analysis is not sufficient for the purpose of modelling and simulations. Hence, we will deploy an additional PK-PD analysis using non-linear mixed-effect modelling to obtain a further understanding of the pharmacokinetics of micafungin. Defining such a PK model will enable us to simulate different dosing regimens and assess the corresponding exposure (AUC) and PK target attainment, taking into account the susceptibility profiles of the pathogen.
Micafungin clinical breakpoints have been defined in a phase III clinical study among patients with invasive candidiasis. An AUC:MIC between 3000 and 12,000 was associated with 98% success for all Candida species. A specific target was defined of an AUC:MIC ratio of 5000:12,000 for non C. parapsilosis species and above 285 for C. parapsilosis [10]. Micafungin has an overall favourable safety profile; therapy with 150–200 mg QD is well tolerated [3].
We aimed to combine our PK data and the clinical breakpoints data to determine the probability of target attainment (PTA) in a population of critically ill patients. This will enable us to make simulations for other regimens to investigate the gain in the PTA in pathogens with altered susceptibility profiles.
2 Materials and Methods
2.1 Ethics
This study was conducted in compliance with the Declaration of Helsinki and approved by the local medical ethics committee (Commissie Mensgebonden Onderzoek region Arnhem-Nijmegen number, clinical trials.gov NCT01783379). Informed consent was given by all participants.
2.2 Study Design, Drug Regimen and Population
All data were collected in a prospective PK study published previously [7]. Patients admitted to the ICU and receiving micafungin for suspected or proven fungal infection were eligible if they met the following inclusion criteria: ≥18 years of age on the day of the first micafungin dose, not receiving micafungin treatment for >2 days before enrolment and having an indwelling central venous or arterial catheter. Exclusion criteria included patients with a history of hypersensitivity to echinocandins or excipients similar to those found in the micafungin preparation, human immunodeficiency virus or hepatitis B/C infection, or abuse of alcohol or drugs. All participants received micafungin 100 mg QD. Micafungin was administered intravenously over approximately 1 h. Micafungin therapy was continued as long as was considered clinically indicated, but the duration of the study was limited to a maximum of 14 days with an additional 3 days after the end of therapy.
Demographic information was gathered and included age, sex, race, weight (available from the medical record previous to ICU admission, estimated or weighted on the ICU), height, relevant co-medication, indication for micafungin use, clinical characteristics, chemistry and haematological parameters. In addition, Acute Physiology and Chronic Health Evaluation II, Sequential Organ Failure Assessment (SOFA), Child-Pugh score and (type of) renal replacement therapy were recorded.
2.3 Pharmacokinetic Sampling and Analysis
At day 3 (±1) patients were intensively sampled (2 mL) at t = 0 (pre-dose) and 0.5, 1, 2, 4, 6, 8, 12, 18 and 24 h post start infusion during a dosing interval. At day 7 (±1), a second PK curve of six samples was drawn at t = 0, (pre-dose) and 1, 4, 8, 12 and 24 h post start infusion. Additional daily trough concentrations were drawn daily until 3 days after cessation of micafungin therapy. A validated ultra-performance liquid chromatography-fluorescence assay was used to analyse the samples, details have been described previously [7].
2.4 Pharmacokinetic Model
Population PK analysis of micafungin was performed with non-linear mixed-effects modelling using the first-order conditional estimation method with interaction between random effects and residual variability as implemented in NONMEM (version 7.3; ICON Development Solutions, Ellicott City, MD, USA) [11]. Pirana interface (PiranaJS, version 1.01) (Pirana Software & Consulting BV 2016, Amsterdam, The Netherlands) [12, 13] was used as an interface for NONMEM, Perl-Speaks-NONMEM (version 4.2.0), Xpose (version 4.5.3) and R (version 3.2.1) [14].
As body weight (BW) is a known confounder for pharmacokinetics, the impact of BW on the pharmacokinetics of micafungin were accounted for by allometric scaling, as proposed previously, with an allometric exponent of 0.75 for all flow parameters and an exponent of 1 for all volume parameters standardised to a 70-kg patient as proposed previously [15–18]. One-, two- and three-compartment models were considered to describe the drug disposition. The primary PK parameters were clearance (CL) and volume of distribution (V). Inter-individual variability (IIV) and inter-occasion variability (IOV) was estimated using an exponential model. Residual variability was evaluated by proportional, additive and combined additive, and proportional models. Inter-individual random effects were evaluated with a single covariance matrix on the parameters of the first compartment as well as with a full covariance matrix on the parameters of all compartments. IOV was considered on CL and V. Structural model selection was guided by objective function value (OFV) as computed by NONMEM, corresponding to minus twice the log-likelihood (a Δ of −3.84 with 1 degree of freedom, Chi-squared distribution, corresponds to a significance level of p = 0.05) goodness-of-fit plots and physiological plausibility. In addition, the precision of the parameter estimates, ETA shrinkage, and IIV and IOV were assessed, as well as parameter correlation. Candidate models were further evaluated by a prediction-corrected visual predictive check (n = 1000 simulations) and a numerical predictive check based on n = 1000 simulations [19]. With the visual predictive check, the observed data were compared with the model-simulated data to evaluate the internal validity of the model.
After selection of the base model, the following covariates were tested on CL and V based on physiological plausibility: albumin, Continuous Veno-Venous Hemofiltration (CVVH) and SOFA. The effect of albumin was assessed on V 1 and CL. The effect of CVVH was assessed on V 1 (dichotomous covariate). SOFA scores were obtained on different days. Missing values of non-sampling days before the observation were replaced by the first value (usually at 48 h) and missing values after observations were carried forward. In the case of completely missing SOFA scores, the median of 7 was used. The SOFA score was divided into a low score (<10) and a high score (>10) based on associated mortality risks [20, 21] and was assessed as a categorical covariate on CL and V.
Covariates were tested in a stepwise fashion (forward inclusion, backward elimination). A covariate was included when it was physiologically plausible and the OFV decreased with 3.84 points (Chi-squared distribution, p = 0.05). The precision of the parameter estimates was assessed using a non-parametric bootstrap method in which resampling of the data to create new datasets with the same size but containing different sets of individuals and yielding new parameter estimates and confidence intervals occurred (n = 1000 replications).
2.5 Monte-Carlo Simulations of Pharmacokinetics and Target Attainment with Various Dosing Regimens
The final model was used to perform a simulation study exploring various dosing regimens. As the ICU cohort used for model building was considered too small for simulation purposes (n = 20), a cohort of 1000 hypothetical individuals with a mean BW of 70 kg with 20% coefficient of variation (CV) in BW was generated for each dosing regimen. This variation in weight (20% CV) was based on the weight distribution of a haematological cohort from our hospital (n = 1706, median 76.4 kg and standard deviation 14.5, resulting in 18.96% CV). Simulations were performed also propagating parameter uncertainty, with the TNPRI function in NONMEM, using priors from the final model.
Five dosing regimens were simulated including licensed regimens and alternative regimens, chosen at the discretion of the researchers. Licensed regimens included (I) 100 mg QD for 14 days and (II) 100 mg QD the first 4 days with 200 mg QD from day 5 (labelled indication for non-responders); alternative regimens included (III) 200-mg loading dose on day 1 followed by 100 mg QD from day 2, (IV) 200-mg loading dose followed by 150 mg QD from day 2 and (V) 200 mg QD. A 200-mg dose is not expected to be associated with toxicity as micafungin doses of 8 mg/kg are well tolerated [4].
2.6 Probability of Target Attainment
The PK-PD target for micafungin in the treatment of invasive candidiasis was determined by the group of Andes et al. [10]. The exposure-response relationship of micafungin has been well established: an AUC/MIC ratio of 3000:12,000 has previously been associated with a 98% mycological response for all Candida infections, while a target of 5000:12,000 has been associated with a 97.8% mycological response for non-C. parapsilosis infections [10]. We used both an AUC/MIC ratio of > 3000 well as 5000 as the PK-PD target for the simulations. Furthermore, the model presented will allow other researchers to use our PK model for simulations on different Candida species whenever needed. However, this is beyond the scope of this article as the focus is on PK variability in a population of critically ill patients.
Target attainment at days 3 and 14 was assessed for a range of clinically relevant MIC values (0.002–1 mg/L) of the Clinical and Laboratory Standards Institute. This range includes both the modal MIC for micafungin for C. albicans (0.015 mg/L) as the epidemiological cut-off MIC (0.03 mg/L, Clinical and Laboratory Standards Institute reference method) [22, 23].
2.7 Minimum Inhibitory Concentration Distribution
In addition to the determination of the PTA for each individual MIC, the PTA considering the population distribution was evaluated. For each MIC, the fraction of simulated patients who attained the PK target was multiplied by the fraction of the MIC distribution of C. albicans. The cumulative fraction of response was calculated as the sum of fraction products over all MICs. The population distribution of C. albicans was gathered from Pfaller et al., as this species is often involved in candidaemia in ICU patients [22].
3 Results
3.1 Patients, Dosing and Samples
Twenty patients completed the first PK curve on day 3 and were eligible for analysis. A total of 356 time-concentration observations were available to build the model. Baseline patient characteristics are summarised in Table 1. Median age was 68 years (range 20–84 years) and median BW was 77 kg (range 50–134 kg). All patients had pronounced hypoalbuminaemia (serum albumin ≤34 g/L). All patients received micafungin 100 mg QD. No dose adaptations were performed [7].
3.2 Population Pharmacokinetic Model
A two-compartment disposition model with first-order elimination from the central compartment and a proportional residual error model fitted the data best. IIV on CL and V 1 further improved the model while data did not support the addition of IIV on Q or V 2. Allowing a correlation between IIV of CL and V 1 further improved the model (difference OFV = 13.98). High IOV on V 1 was observed, indicating important variation in V 1 from day to day within this population. Parameter estimates of the model are shown in Table 2. CL, V 1, Q and V 2 were estimated to be 1.10 L/h, 17.6 L, 0.363 L/h and 3.63 L. The IIV on CL and V 1 were estimated to be 40 and 73% CV with ETA shrinkage of 1.2 and 41%, respectively, while IOV on V 1 was estimated to be 37% CV. No covariates were identified to significantly affect CL or V 1.
Basic goodness-of-fit plots are shown in the supplementary file (Fig. S1). The plots did not show major deviations. A prediction-corrected visual predictive check of the final model is shown in the supplementary file (Fig. S2). Predictions were consistent with the observations, suggesting a good validity of the model to the data. The numerical predictive check showed that 0.9% (95% confidence interval 0–6.8%) of observations fell below the 95% prediction interval and 2.0% (95% confidence interval 0–8.8%) fell above the 95% prediction interval. Parameter precision was assessed using a bootstrap re-sampling approach of the final model, the results of which are listed in Table 2.
3.3 Monte-Carlo Simulations of Alternative Dosing Regimens
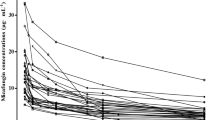
Monte-Carlo simulations were performed to assess daily exposure (AUC0–24h) obtained with licensed and alternative dosing regimens. AUC0–24h values on day 14 of therapy are shown in Fig. 1. Median (interquartile range) AUC0–24h values on day 3 for the five regimens (I–V) were 86 (62–116), 86 (62–116), 92 (66–125), 132 (95–180) and 172 (124–232) mg h/L and on day 14 were 91 (67–122), 183 (135–244), 91 (67–122), 137 (101–183) and 183 (135–244) mg h/L, respectively.
Area under the concentration–time curve (AUC) over 24 h on day 14 based on Monte-Carlo simulations. The horizontal line represents the AUC over 24 h for healthy volunteers. Licensed regimens, I 100 mg daily (QD) and II 100 mg QD followed by 200 mg QD from day 5. Alternative regimens, III a 200-mg loading dose followed by 100 mg maintenance; IV a 200-mg loading dose followed by 150 mg maintenance; and V 200 mg QD
Simulated plasma concentration–time profiles of the first week of therapy in a typical patient weighing 70 kg following the different dosing regimens are shown in the supplementary file (Fig. S3). Administration of a loading dose resulted in higher exposure early in therapy (regimens III–IV).
3.4 Pharmacokinetic Target Attainment
The PTA on day 3 of therapy based on the Monte-Carlo simulations are shown in Figs. 2 and 3. As can be expected, the PTA increased with increasing doses and decreased with higher MIC values. For example, adding a loading dose together with increasing the maintenance dose to 150–200 mg QD led to increased target attainment: ≤46 vs. >74% on day 3 for a micafungin MIC of 0.032 mg/L for the target of >3000.
Predicted target attainment at day 3 vs. minimal inhibitory concentration (MIC) for all five simulated regimens based on a clinical target area under the concentration–time curve over 24 h/MIC ratio of ≥3000 (valid for all Candida spp.). Bars represent the wild-type population distribution of Candida albicans for micafungin, as gathered from [22]
Predicted target attainment at day 3 vs. minimal inhibitory concentration (MIC) for all five simulated regimens based on a clinical target area under the concentration–time curve over 24 h/MIC ratio of ≥5000 (valid for non-Candida parapsilosis spp.). Bars represent the wild-type population distribution of Candida albicans for micafungin, as gathered from [22]
The main differences in the PTA between days 3 and 14 are observed for regimen II, as with this regimen the maintenance dose is increased from 100 to 200 mg on day 5 of therapy. The PTA for all simulated regimens is also given as a supplementary file (Supplementary Tables 1, 2). Table 3 shows the results of the PTA integrated with the distribution of the MIC for C. albicans and non-C. parapsilosis, resulting in the cumulative fraction of the predicted response. Higher maintenance dose (regimens II, IV and V) resulted in a higher cumulative PTA.
4 Discussion
We developed a population PK model for micafungin in ICU patients. The model was successfully used to assess different dosing regimens of micafungin to predict the corresponding PTA, taking into account parameter uncertainty. The simulations revealed that the majority of the population is treated sufficiently with the current licensed dosing regimen, but the PTA for infections with Candida species with a MIC of 0.032 mg/L can be improved by increasing the maintenance dose a priori to 200 mg.
Clearance in our cohort was 1.10 L/h and modestly higher compared with CL in healthy volunteers [24, 25]. Three population PK models have been published previously. Clearance in our cohort was similar to ICU patients on CVVH, mechanical ventilation or with an intra-abdominal infection [26–29]. Inter-individual variability on CL was 40% CV in our cohort and therefore higher than observed in healthy volunteers [24] or ICU patients on CVVH (17–20% CV) [26] but similar to ICU patients with sepsis and mechanical ventilation (34%) [29]. Volume of distribution was higher than in healthy volunteers (13.3 L for a healthy 70-kg patient) [24] and the central V was higher than in ICU with severe peritonitis, sepsis or burn injuries [27–29] but very similar to ICU patients on CVVH (22.5 L for a 70-kg patient) [26]. IIV on V 1 was 73% CV in our cohort and thereby two- to ten-fold higher compared with other studies (8–38% CV) [24, 26, 29]. One explanation could be that healthy volunteers and subjects on CVVH are more homogenous populations, in which less variability is observed, while our cohort consisted of ICU patients with and without CVVH. The estimated IIV may also have been inflated by one influential individual (BW 134 kg) who seems to be responsible for the improved model fit when including IIV on V 1. V 2 was lower in our analysis but the total V (V 1 + V 2) was comparable to other pharmacokinetics. [26, 29]
BW was a priory added in the model on CL and V 1 in agreement with physiological plausibility and based on previous work. [15–18, 26, 29]. It remains a matter of debate whether one should estimate or fix the allometric exponents. One group empirically estimated this for micafungin [29] while another one fixed it [26]. For illustration purposes, we have estimated the allometric exponent of BW to CL, which was 1.26 and this did not significantly improve the model fit (ΔOFV −2.97); 1.26 is very different from what is physiologically plausible and from the results of another group (0.59) [29]. Based on our data (n = 20 patients), the true exponent is not identifiable and using an empirical estimate would not allow for extrapolation beyond our dataset.
Although not present in our cohort, in the case of morbidly obese, critically ill patients, BW may not be the ideal parameter to relate size to pharmacokinetics. Other weight-derived parameters such as fat-free mass could be alternative descriptors to explain the variability in PK parameters in this subpopulation [30]. As micafungin has a relative low V, only a small fraction is metabolised and kidney function does not play an important role [3, 26]. BW is assumed to adequately describe the relationship between body size and the PK parameters for the normal weight ICU patients [3].
We found an important IOV on V, which means that V may change considerably from day to day within one patient. While our data also supported the addition of IOV on CL, we considered IOV on V more physiologically plausible, as we observed important fluctuations in peak concentrations of micafungin. Day-to-day fluctuations in V may be explained by haemodynamic changes including fluid retention or fluid loss as result of a capillary leak, which may occur in ICU patients [31, 32]. Moreover, including IOV on both CL and V 1 resulted in an unidentifiable model with parameter correlation and including both was, therefore, not considered. A study among ten ICU patients on CVVH found an IOV on V 1 and V 2 of 27–28% CV, which was lower compared with our cohort (37% CV) [26]. This difference might be explained by the difference in clinical condition: patients on CVVH might be haemodynamically more stable and controlled in terms of fluid retention and diuresis than ICU patients not on CVVH. This is reflected in the lower IOV of V 1.
As referenced, we have now conducted several population PK studies of echinocandins in ICU patients. We observed some differences between the various echinocandins. Unlike caspofungin with identical CL and V in critically ill patients compared with healthy volunteers, micafungin showed a higher CL (1.10 L/h compared with 0.55 L/h) and a higher V (21.2 L compared with 13.9 L for V 1 and V 2 together) in ICU patients [33]. Anidulafungin showed similar changes in CL when comparing critically ill patients with healthy volunteers, while V was equal in both populations [34]. It remains unclear why micafungin pharmacokinetics changes but caspofungin pharmacokinetics is less affected by critical illness, as we could not find any covariates, apart from BW, to explain the variability in PK parameters. Covariates might be obscured owing to the overall high variability in pharmacokinetics among ICU patients, caused by a mixture of factors (e.g. systemic inflammatory response, capillary leak, protein-binding capacity) [35]. Combining datasets and thereby increasing sample size may help to further clarify this.
Our results confirm that the exposure (AUC0–24h) in the ICU population after 100 mg QD is much lower than the exposure with the same dose in healthy volunteers, which is consistent with our previous analysis [7]. Increasing the maintenance dose in ICU patients to 150 mg led to equal exposure compared with healthy volunteers. When the labeled 200 mg is chosen, this would lead to higher exposure compared with healthy volunteers. Theoretically, lower exposure risks decreased efficacy and it is known that AUC is inversely linked to disease outcome when exposed to pathogens with increasing MICs [9].
We have simulated the licensed regimens, as well as alternative regimens. Based on our simulations and the PTA assessment with the 3000 target (all Candida spp.), the majority (83%) of the ICU population is treated adequately with the currently licensed 100-mg maintenance dose. Higher maintenance doses of 200 mg QD are only required in the case of infections with species with decreased susceptibility. However, based on the 5000 target (non-C. parapsilosis), the majority of the population may benefit from a dose increase to 200 mg QD as a result of low target attainment with the 100 mg QD (62% attains the 5000 target with MIC 0.016). Although this can be considered a worst-case scenario, no susceptibility profiles are available upon the start of therapy, for which a 200-mg dose QD may be beneficial until the results of the microbiology are available. If the MIC allows, one can scale down to 100 mg QD. This should be evaluated prospectively. Alternatively, a 200-mg loading dose for all ICU patients can be beneficial, to achieve early adequate exposure (also shown in Fig. S3). Especially given the high IOV of V 1, it is of great importance to adequate saturate all compartments with micafungin.
Our results are comparable to previous work [26, 29] and confirm that species with attenuated MICs may benefit from higher maintenance doses. It should be noted that PK-PD targets vary considerable among Candida species and the target greatly influences the outcome: the PTA decreases when the target increases [8]. Thus, correct selection of the target is crucial for adequate interpretation of the PTA. When starting therapy, the MIC is often unknown. With this in mind, our results encourage the prospective evaluation of a higher initial dose (e.g. 200 mg maintenance), as it may have the potential to decrease the rate of patients not attaining the target. This should be evaluated for superiority in a prospective trial.
In addition, modelling and simulation are always associated with uncertainty, further challenging the interpretation of the estimated PTA. We therefore took parameter uncertainty into account when performing Monte-Carlo simulations of micafungin in ICU patients, subsequently used for the PTA predictions. The variability in exposure (Fig. 1) is a combination of parameter uncertainty and variability in BW. Although this uncertainty is taken into account in the PTA predictions, Fig. 2 does not show any variability as it was based on the proportion of patients attending the PK target. Another approach could be to perform multiple simulations (e.g. 1000 times) using parameter precision information from a bootstrap analysis and calculate confidence intervals around the PTA [36].
The current work is inevitably associated with some limitations, which are discussed below. The first relates to the high IIV on V 1, which may have been inflated by an influential individual with a BW of 134 kg, the highest BW of the cohort. However, the inclusion of the parameter improved the model fit to the data significantly and it is not surprising to encounter deviating individuals in heterogeneous ICU cohorts. We therefore decided to retain this individual in the cohort and proceed with IIV on V 1, but at the same time underline the uncertainty in the estimated value of this parameter. The second limitation relates to the fact we did not have information on the unbound micafungin concentrations. As micafungin is highly protein bound, fluctuations in albumin (likely to occur among ICU patients) may influence total concentrations and thereby the PTA. This might have led to an underestimation rather than an overestimation of the PTA.
5 Conclusion
In summary, a population PK model of micafungin in ICU patients was developed and used to assess the PTA for licensed as well as alternative dosing regimens. We are the first to incorporate uncertainty in parameter estimates in Monte-Carlo simulations. We conclude that the majority of the population is adequately treated with a 100-mg maintenance dose based on the 3000 target but not with the 5000 target. Candida species with higher MICs require higher maintenance doses of 200 mg. As it takes several days before microbiology results are obtained, starting with a higher initial dose (e.g. 200 mg QD) may result in a superior treatment outcome. Although this alternative dosing strategy may be off-label, our findings encourage its investigation.
References
Vincent JL, Rello J, Marshall J, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009;302:2323–9.
Kullberg BJ, Arendrup MC. Invasive candidiasis. N Engl J Med. 2015;373:1445–56.
European Medicines Agency. Mycamine: EPAR scientific discussion. 2008. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Public_assessment_report/human/000734/WC500031079.pdf. Accessed 2017 Jan 19.
European Medicines Agency. Summary of product characteristics: mycamine. 2009. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000734/WC500031075.pdf. Accessed 2017 Jan 19.
Pappas PG, Kauffman CA, Andes DR, et al. Executive summary: clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62:409–17.
Andes DR, Safdar N, Baddley JW, et al. Impact of treatment strategy on outcomes in patients with candidemia and other forms of invasive candidiasis: a patient-level quantitative review of randomized trials. Clin Infect Dis. 2012;54:1110–22.
Lempers VJ, Schouten JA, Hunfeld NG, et al. Altered micafungin pharmacokinetics in intensive care unit patients. Antimicrob Agents Chemother. 2015;59:4403–9.
Andes D, Diekema DJ, Pfaller MA, et al. In vivo comparison of the pharmacodynamic targets for echinocandin drugs against Candida species. Antimicrob Agents Chemother. 2010;54:2497–506.
Andes DR, Diekema DJ, Pfaller MA, et al. In vivo pharmacodynamic target investigation for micafungin against Candida albicans and C. glabrata in a neutropenic murine candidiasis model. Antimicrob Agents Chemother. 2008;52:3497–503.
Andes D, Ambrose PG, Hammel JP, et al. Use of pharmacokinetic-pharmacodynamic analyses to optimize therapy with the systemic antifungal micafungin for invasive candidiasis or candidemia. Antimicrob Agents Chemother. 2011;55:2113–21.
Beal S, Sheiner LB, Boeckmann A. NONMEM user’s guides (1989–2006). Ellicott City: ICON Development Solutions; 2006.
Jonsson EN, Karlsson MO. Xpose: an S-PLUS based population pharmacokinetic/pharmacodynamic model building aid for NONMEM. Comput Methods Programs Biomed. 1999;58:51–64.
Lindbom L, Pihlgren P, Jonsson EN. PsN-Toolkit: a collection of computer intensive statistical methods for non-linear mixed effect modeling using NONMEM. Comput Methods Programs Biomed. 2005;79:241–57.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2013.
Anderson BJ, Holford NH. Mechanistic basis of using body size and maturation to predict clearance in humans. Drug Metab Pharmacokinet. 2009;24:25–36.
Gumbo T, Hiemenz J, Ma L, et al. Population pharmacokinetics of micafungin in adult patients. Diagn Microbiol Infect Dis. 2008;60:329–31.
Hall RG, Swancutt MA, Gumbo T. Fractal geometry and the pharmacometrics of micafungin in overweight, obese, and extremely obese people. Antimicrob Agents Chemother. 2011;55:5107–12.
Holford N, Heo YA, Anderson B. A pharmacokinetic standard for babies and adults. J Pharm Sci. 2013;102:2941–52.
Bergstrand M, Hooker AC, Wallin JE, Karlsson MO. Prediction-corrected visual predictive checks for diagnosing nonlinear mixed-effects models. AAPS J. 2011;13:143–51.
Ferreira FL, Bota DP, Bross A, et al. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286:1754–8.
Vincent JL, de Mendonca A, Cantraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26:1793–800.
Pfaller MA, Boyken L, Hollis RJ, et al. Wild-type MIC distributions and epidemiological cutoff values for the echinocandins and Candida spp. J Clin Microbiol. 2010;48:52–6.
Pfaller MA, Diekema DJ, Andes D, et al. Clinical breakpoints for the echinocandins and Candida revisited: integration of molecular, clinical, and microbiological data to arrive at species-specific interpretive criteria. Drug Resist Updat. 2011;14:164–76.
Hebert MF, Smith HE, Marbury TC, et al. Pharmacokinetics of micafungin in healthy volunteers, volunteers with moderate liver disease, and volunteers with renal dysfunction. J Clin Pharmacol. 2005;45:1145–52.
Undre NA, Stevenson P, Kuse ER, Demeyer I. Pharmacokinetics of micafungin in adult patients with invasive candidiasis and candidemia. Open J Med Microbiol. 2012;2:84–90.
Maseda E, Grau S, Villagran MJ, et al. Micafungin pharmacokinetic/pharmacodynamic adequacy for the treatment of invasive candidiasis in critically ill patients on continuous venovenous haemofiltration. J Antimicrob Chemother. 2014;69:1624–32.
Grau S, Luque S, Campillo N, et al. Plasma and peritoneal fluid population pharmacokinetics of micafungin in post-surgical patients with severe peritonitis. J Antimicrob Chemother. 2015;70:2854–61.
Garcia-de-Lorenzo A, Luque S, Grau S, et al. Comparative population plasma and tissue pharmacokinetics of micafungin in critically ill patients with severe burn injuries and patients with complicated intra-abdominal infection. Antimicrob Agents Chemother. 2016;60:5914–21.
Jullien V, Azoulay E, Schwebel C, et al. Population pharmacokinetics of micafungin in ICU patients with sepsis and mechanical ventilation. J Antimicrob Chemother. 2017;72(1):181–9.
Alobaid AS, Hites M, Lipman J, et al. Effect of obesity on the pharmacokinetics of antimicrobials in critically ill patients: a structured review. Int J Antimicrob Agents. 2016;47:259–68.
Roberts JA, Abdul-Aziz MH, Lipman J, et al. Individualised antibiotic dosing for patients who are critically ill: challenges and potential solutions. Lancet Infect Dis. 2014;14:498–509.
Roberts JA, Lipman J. Pharmacokinetic issues for antibiotics in the critically ill patient. Crit Care Med. 2009;37:840–51 (quiz 59).
Martial LC, Bruggemann RJ, Schouten JA, et al. Dose reduction of caspofungin in intensive care unit patients with Child Pugh B will result in suboptimal exposure. Clin Pharmacokinet. 2016;55:723–33.
Liu P, Ruhnke M, Meersseman W, et al. Pharmacokinetics of anidulafungin in critically ill patients with candidemia/invasive candidiasis. Antimicrob Agents Chemother. 2013;57:1672–6.
Blot SI, Pea F, Lipman J. The effect of pathophysiology on pharmacokinetics in the critically ill patient: concepts appraised by the example of antimicrobial agents. Adv Drug Deliv Rev. 2014;77:3–11.
Colin P, Eleveld DJ, Jonckheere S, et al. What about confidence intervals? A word of caution when interpreting PTA simulations. J Antimicrob Chemother. 2016;71:2502–8.
Acknowledgements
The authors thank Vincent Lempers and Thomas Dorlo for their contributions to this study.
Author contributions
Dr. Brüggemann designed the study. Drs. Schouten, Hunfeld, de Lange, van Leeuwen and Pickkers recruited patients for this study. Ms. Martial, Dr. Ter Heine and Dr. Brüggemann analysed the data. Dr. Verweij supervised the microbiology results. All authors have read and improved the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The original study published by Lempers et al. was supported by an unrestricted educational grant from Astellas.
Conflict of interest
R. J. Brüggemann has served as a consultant to and has received unrestricted and research grants from Astellas Pharma, Inc., Gilead Sciences, Merck Sharpe and Dohme Corp., and Pfizer, Inc. P. E. Verweij has served as a consultant to and has received unrestricted and research grants from Astellas Pharma, Inc., Gilead Sciences, Merck Sharpe and Dohme Corp., and Pfizer, Inc., F2G Ltd. J. A. Schouten has received support for educational activities from Astellas and Merck Sharpe and Dohme.
Additional information
On behalf of the FANTASTIC Consortium: Jeroen A. Schouten, Dylan W. de Lange, Roger J. Brüggemann.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Martial, L.C., ter Heine, R., Schouten, J.A. et al. Population Pharmacokinetic Model and Pharmacokinetic Target Attainment of Micafungin in Intensive Care Unit Patients. Clin Pharmacokinet 56, 1197–1206 (2017). https://doi.org/10.1007/s40262-017-0509-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-017-0509-5