Abstract
Background
Abrocitinib, an oral, once-daily Janus kinase 1-selective inhibitor, improved itch severity, sleep, and work productivity versus placebo in patients with moderate-to-severe atopic dermatitis.
Objective
The aim of this study was to investigate relationships among itch, sleep, and work productivity in the phase III JADE MONO-2 clinical trial.
Methods
A repeated-measures longitudinal model was used to examine relationships between itch (using the Peak Pruritus Numerical Rating Scale [PP-NRS] or Nighttime Itch Scale [NTIS]) and sleep disturbance/loss (using the Patient-Oriented Eczema Measure sleep item and SCORing AD Sleep Loss Visual Analog Scale) and, separately, between itch and work productivity (using the Work Productivity and Activity Impairment-Atopic Dermatitis Version 2.0 questionnaire). Mediation modelling was used to investigate the effect of treatment (abrocitinib vs placebo) on work impairment via improvements in itch and sleep.
Results
The relationships between itch/sleep and itch/work productivity were approximately linear. PP-NRS scores of 0, 4–6, and 10 were associated with 0 days, 3–4 days, and 7 days per week of disturbed sleep, respectively. PP-NRS or NTIS scores of 0–1, 4–5, and 10 were associated with 0–10%, 20–30%, and >50% overall work impairment, respectively. Seventy-five percent of the effect of abrocitinib on reducing work impairment was indirectly mediated by improvement in itch, followed by sleep.
Conclusion
These results quantitatively demonstrate that reducing itch severity is associated with improvements in sleep and work productivity. Empirical evidence for the mechanism of action of abrocitinib showed that itch severity is improved, which reduces sleep loss/sleep disruption and, in turn, improves work productivity.
Clinical Trial Registration
NCT03575871
Plain Language Summary
Atopic dermatitis (AD), also called atopic eczema, is a common skin disease that is associated with itch and reduced quality of life. Abrocitinib, a recently approved medicine for AD, was shown in clinical trials to improve itch, which is considered the most bothersome symptom to people with AD. Abrocitinib also improved sleep outcomes and work productivity in people with moderate or severe AD. It is unknown if improvement in itch can lead to improvement in sleep and work productivity. We analyzed data from the JADE MONO-2 study, which included 391 people who received treatment with abrocitinib or placebo for 12 weeks. We used mathematical modelling to study relationships between itch and sleep or work productivity. We also wanted to study if the improvements in itch and sleep with abrocitinib treatment had an impact on work productivity. We found that a relationship existed between itch, sleep disturbance, and work impairment; as itch improved, so too did sleep disturbance and work impairment. When people were treated with abrocitinib, they experienced relief from itch, which improved sleep, which in turn reduced work productivity loss. Larger and longer studies are needed to confirm these results. This analysis further informs the expectations of patients with moderate or severe AD as it relates to progression of symptom relief after treatment with abrocitinib.
Similar content being viewed by others
Atopic dermatitis (AD) is a chronic skin disease associated with intense itch and reduced quality of life. |
This analysis demonstrated the association among itch severity, poor sleep, and reduced work productivity in patients with moderate-to-severe AD. Treatment with abrocitinib was shown to reduce itch, which in turn improved sleep outcomes, resulting in less work impairment. |
1 Introduction
Atopic dermatitis (AD) is a chronic, relapsing inflammatory skin disease that affects up to 20% of children and 5–10% of adults worldwide [1,2,3,4,5,6]. AD is typically characterized by intense pruritus (itch), eczematous lesions, and dry skin [5], of which itch is the most bothersome symptom [4, 7, 8]. Uncontrolled chronic itch is often worse at night and can lead to sleep disturbance/loss and decreased quality of life (QoL) [2, 9,10,11,12,13], which can in turn adversely impact function and productivity. Increasing disease severity augments the negative impact of AD on work productivity [3, 14,15,16].
The pathophysiology of itch in AD is influenced by extrinsic factors (i.e., allergens and irritants), genetic predisposition, and a type-2 immune response mediated via the signaling of pruritic and inflammatory cytokines (i.e., interleukin [IL]-31, IL-4, and IL-13) [17,18,19,20]. Itch likely contributes to sleep disturbance in patients with AD and other inflammatory diseases that involve upregulation of IL-4 and IL-13, given the significant increase in sleep impairment seen in patients with psoriasis and itch compared with those without pruritus [21,22,23]. As such, it is possible that systemic therapies targeting key pruritic cytokines in the itch pathway may also act to improve sleep quality and subsequently other aspects of daily life in patients with AD.
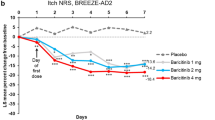
Abrocitinib is an oral, once-daily, selective Janus kinase 1 (JAK1) inhibitor approved for the treatment of moderate-to-severe AD in adults and adolescents [24,25,26,27]. Abrocitinib was shown to be a well-tolerated and effective treatment for moderate-to-severe AD in multiple clinical studies (phase IIb, JADE MONO-1, JADE MONO-2, JADE COMPARE, JADE TEEN, JADE REGIMEN, and JADE DARE) [28,29,30,31,32,33,34]. Significantly greater proportions of patients treated with abrocitinib (200 mg or 100 mg) achieved an Investigator Global Assessment (IGA) response of clear (0) or almost clear (1) with ≥2-grade improvement, a ≥75% improvement in Eczema Area and Severity Index score (EASI-75) response, and/or ≥4-point improvement from baseline in Peak Pruritus Numerical Rating Scale (PP-NRS4) response, than those treated with placebo [30]. In the phase III JADE MONO-1 and JADE MONO-2 trials, abrocitinib resulted in greater decreases from baseline in PP-NRS score compared with placebo [22, 23]. Additionally, in JADE MONO-2, greater decreases were observed with abrocitinib in Work Productivity and Activity Impairment Questionnaire-Atopic Dermatitis (WPAI-AD), Patient-Oriented Eczema Measure sleep item (POEM sleep item), and SCORing AD Sleep Visual Analog Scale (SCORAD Sleep Loss VAS) scores compared with placebo [30, 35].
The direct and indirect effects of abrocitinib on improving itch, sleep, and work productivity have not been evaluated [13]. This supplemental (post hoc) analysis used data from JADE MONO-2 to examine the relationships between itch and sleep disturbance and between itch and overall work impairment. In addition, a mediation model was developed to simultaneously evaluate interrelationships among treatment, itch, sleep, and work productivity. We thereby sought to quantify the direct and indirect effects of abrocitinib on work productivity through analysis of itch and sleep.
2 Methods
2.1 Study Design
JADE MONO-2 (NCT03575871) was a multicenter, international, phase III, randomized, placebo-controlled, parallel-group trial. Patients with moderate-to-severe AD were randomly assigned (2:2:1) to receive abrocitinib 200 mg, 100 mg, or placebo for 12 weeks. Full study details, including the primary efficacy and safety results, have been published previously [30]. The study was conducted in compliance with the ethical principles originating in or derived from the Declaration of Helsinki and in compliance with all International Council for Harmonization Good Clinical Practice Guidelines. All local regulatory requirements were followed. This research was approved by institutional review boards or ethics committees at each study site. An internal review committee monitored the safety of patients throughout the study. All patients provided written informed consent.
2.2 Patients
Eligible patients were aged ≥12 years with clinical diagnosis of moderate-to-severe AD (IGA ≥3, EASI ≥16, percentage of body surface area involvement [%BSA] ≥10, PP-NRS [defined as the worst itch experienced in the last 24 h; used with permission of Regeneron Pharmaceuticals, Inc. and Sanofi [36]] ≥4 on the day of the baseline visit) and a recent (within 6 months) history of inadequate response to topical corticosteroids or calcineurin inhibitors given for ≥4 weeks or an inability to receive topical treatment because it was medically inadvisable. Previous dupilumab use was permitted if it was discontinued >6 weeks before study initiation. Concomitant use of topical (corticosteroids, calcineurin inhibitors, tars, antibiotic creams, or antihistamines) or systemic therapies for AD was prohibited [30]. Rescue medication (including topical corticosteroids) was prohibited during the study. Full inclusion and exclusion criteria are published elsewhere [30].
2.3 Post Hoc Analysis
A repeated-measures longitudinal model [37, 38] was employed to estimate relationships between itch severity (PP-NRS or Night Time Itch Scale [NTIS], scored 0–10, higher scores indicating worse itch) as a predictor and sleep disturbance (POEM sleep item or SCORAD Sleep Loss VAS) as an outcome. The relationship between itch severity (PP-NRS or NTIS) as a predictor and work productivity (WPAI-AD) as an outcome was also investigated. In addition, the relationship between POEM sleep item and SCORAD Sleep Loss VAS was examined.
PP-NRS and NTIS were assessed daily during the 28-day screening period and the first 2 weeks after randomization, followed by single measurements at week 4, week 8, and week 12. As a result, in the analysis NTIS and PP-NRS values for baseline (week 0), week 1 and week 2 are represented by the mean of all available weekly measurements (if at least 4 observations were available). The POEM sleep item and SCORAD Sleep Loss VAS were collected at baseline and weeks 2, 4, 8, and 12.
WPAI-AD was assessed in adult patients at baseline and week 12 to measure the effect of AD on work productivity and regular activities during the previous 7 days. The activity impairment component of this questionnaire was completed by all adult patients, while the work impairment component was completed by only those adult patients who were employed during the study period and assessed the level of impairment in productivity while working. The WPAI-AD is designed in such a way that questions that are not applicable (i.e., impact of AD on work productivity) can be skipped by patients who are not employed and as such, for these patients, absenteeism, presenteeism, and overall work productivity were not calculated. As this omission is by design, these domains should not be considered as ‘missing’.
To study the appropriateness of the linear approximation of the relationship between the predictor and the outcome, two models were investigated. The main model, with the predictor as a continuous variable, imposed a linear relationship between the predictor and the outcome. A model with the predictor as a categorical variable (sensitivity analysis) was also studied whereby a functional relationship between the outcome and the predictor is not imposed. The models assume that measurements from the same patient are not independent, which means that the error terms covary over time within a patient, and the error at one time point is allowed to covary with the error at another time point for any patient [38]. The covariance of the error terms for the same patient over time was modeled with a spatial power covariance structure that allows for time intervals that are not evenly spaced [38]. The models, which were fit in SAS with Prox Mixed and the Repeated statement, use all available data and assume that data were missing at random.
A mediation model, which can help elucidate the mechanism of action of a drug, was used to investigate the direct and indirect effects of the treatment (abrocitinib [200 mg and 100 mg] vs placebo) on overall work impairment (WPAI-AD), and how these effects were influenced by itch (PP-NRS and NTIS), and sleep (POEM sleep item and SCORAD Sleep Loss VAS), denoted as mediators [39]. The initial model included indirect causal paths from abrocitinib to overall work impairment through itch severity (latent variable F1) and sleep (latent variable F2) as well as direct effects of abrocitinib to overall work impairment (representing all other possible paths; Supplementary Fig. S1, see electronic supplementary material [ESM]). Variables e_ppnrs, e_ntis, e_poem, e_scrd, and e_wpai represent error terms, which reflect unexplained variation due to random measurement error (score unreliability). Variables e_itch and e_sleep represent disturbance terms, which reflect unexplained variation due to omitted (unmeasured) causes and score unreliability in the corresponding latent variables. Based on the results of the initial model, the mediation model can be re-specified to resolve any irregularities and contradictions.
3 Results
3.1 Patients
This post hoc analysis used data from the JADE MONO-2 study (n = 391), which included patients randomized to treatment with abrocitinib 200 mg, abrocitinib 100 mg, or placebo. The baseline disease and demographic characteristics of these patients have been previously reported and were generally similar across treatment groups (Table 1) [30]. Patients from the JADE MONO-2 study were mostly male (59%) with a mean age of 35.1 years and an average PP-NRS score of 7 [30]. For this post hoc analysis, only those patients with at least one observation for each of the parameters assessed in the respective associations were included (Table 2).
3.2 Linearity Between Outcomes Through a Longitudinal Model
All available data from baseline to week 12 were included in a repeated-measures longitudinal model, with predictors as continuous or categorical variables. Similar results were observed in models in which the predictor was used as a continuous variable versus a categorical variable, supporting the linearity assumption for (a) the relationships between itch (PP-NRS and NTIS) and sleep (SCORAD sleep loss VAS and POEM sleep items) (Fig. 1); (b) the relationships between PP-NRS as a predictor and either POEM sleep item or SCORAD Sleep Loss VAS as the outcome, or WPAI as the outcome for work productivity (Fig. 2); and (c) the relationship between NTIS as a predictor and either POEM sleep item or SCORAD Sleep Loss VAS as the outcome, or WPAI as the outcome for work productivity (Fig. 3).
Relationships between a PP-NRS and NTIS and b SCORAD and POEM sleep items. NTIS Night Time Itch Scale, POEM Patient-Oriented Eczema Measure, PP-NRS Peak Pruritus Numerical Rating Scale, SCORAD Sleep Loss VAS SCORing of Atopic Dermatitis Sleep Loss Visual Analog Scale, WPAI-AD Work Productivity and Activity Impairment-Atopic Dermatitis
Relationships between outcomes and PP-NRS as the anchor (continuous predictor or categorical predictor): a PP-NRS and POEM Sleep item, b PP-NRS and SCORAD Sleep Loss VAS, and c PP-NRS and WPAI overall work impairment. NTIS Night Time Itch Scale, POEM Patient-Oriented Eczema Measure, PP-NRS Peak Pruritus Numerical Rating Scale, SCORAD Sleep Loss VAS SCORing of Atopic Dermatitis Sleep Loss Visual Analog Scale, WPAI Work Productivity and Activity Impairment questionnaire
Relationships between outcomes and NTIS as the anchor (continuous predictor or categorical predictor): a NTIS and POEM sleep item, b NTIS and SCORAD Sleep Loss VAS, and c NTIS and WPAI overall work impairment. NTIS Night Time Itch Scale, POEM Patient-Oriented Eczema Measure, PP-NRS Peak Pruritus Numerical Rating Scale, SCORAD Sleep Loss VAS SCORing of Atopic Dermatitis Sleep Loss Visual Analog Scale, WPAI Work Productivity and Activity Impairment questionnaire
The relationship between itch and the POEM sleep item showed that PP-NRS (N = 390) scores of 0, 4–6, and 10 and NTIS (N = 389) scores of 0, 4–6, and 9–10 are associated with no days, 3–4 days per week, and every day of disturbed sleep, respectively (Fig. 4a): every 1-point improvement in itch corresponded to an approximate 0.4-point improvement in the POEM sleep item. The relationship between itch and WPAI-AD showed that PP-NRS (N = 220) scores of 0–1, 4–5, and 10 and NTIS (N = 219) scores of 0–1, 4–5, and 10 are associated with 0–10%, 20–30%, and >50% overall work impairment, respectively (Fig. 4b): every 1-point improvement in itch corresponded to an approximate 5% improvement in WPAI-AD overall work impairment. With the interpretations of the relationships between outcomes found in the longitudinal model, further investigation of specific paths between outcomes was evaluated through mediation modeling.
Interpretation of the association between itch and a sleep and b overall work impairment. NTIS Night Time Itch Scale, POEM Patient-Oriented Eczema Measure, PP-NRS Peak Pruritus Numerical Rating Scale, SCORAD Sleep Loss VAS SCORing of Atopic Dermatitis Sleep Loss Visual Analog Scale, WPAI-AD Work Productivity and Activity Impairment-Atopic Dermatitis questionnaire version 2.0
3.3 Mediation Modeling
The mediation model investigated the effect of abrocitinib on work productivity with itch and sleep as mediators. Data from 148 patients at week 12 were available for analysis. The direct effect of abrocitinib on overall work impairment was found to be 2.2% and not statistically significant (p = 0.95); the overall indirect effect was 97.8% and statistically significant (p = 0.0027), indicating that abrocitinib affects overall work impairment predominantly indirectly (Fig. 5a).
Mediation modeling: a direct and overall indirect effects, b path via itch, c path via sleep, and d path via itch and sleep. WPAI-AD Work Productivity and Activity Impairment—Atopic Dermatitis questionnaire version 2.0. Solid, single-headed arrows indicate direct paths; Dashed, single-headed arrows, indicate indirect paths
Furthermore, the path from abrocitinib to overall work impairment through itch was 0.8% (p = 0.97) and through sleep was 22.2% (p = 0.27) (Fig. 5b & c, respectively).
Finally, the effect of treatment on overall work impairment via itch and sleep (i.e., treatment improves itch, improved itch improves sleep, and improved sleep improves overall work impairment) was 74.9% and statistically significant (p = 0.02) (Fig. 5d).
Based on the above results, the mediation model was re-specified: (a) the direct path from treatment to WPAI was excluded, (b) the path from itch (Factor 1) to WPAI was excluded, and (c) the path from treatment to sleep (Factor 2) was also excluded from the model (Supplementary Fig. S2, see ESM). In this re-specified model, treatment affects WPAI overall work impairment only indirectly, first via improving itch, followed by improved sleep outcomes, which in turn reduces work impairment.
4 Discussion
Itch is the most common symptom for patients with AD and affects several aspects of everyday life [40]. Itch, particularly at night, interferes with sleep and the normal cycle of physical and mental relaxation and thus can adversely affect daytime physical and mental function and alertness [13, 41,42,43,44]. This analysis systematically establishes relationships among the patient-reported assessments of itch, sleep, and work productivity and identifies the path that best models the effects of treatment on work productivity through itch and sleep outcomes, evaluating their relative contributions. The relationships between itch and sleep and between itch and work productivity were approximately linear and indicate that greater itch severity is strongly associated with greater sleep disturbance/loss and has a notable impact on work impairment. Severe PP-NRS or NTIS (≥7) is associated with ≥5 days/week of sleep disturbance and ≥30% overall work impairment, with each 1-point reduction in itch severity reducing overall work impairment by 5%.
Intense itch, sleep disturbances, and poor work productivity are all bothersome impacts of AD that have an adverse effect on patients’ QoL [13, 44]. Improvements in these symptoms can provide substantial changes in a patient’s daily life. The mediation model quantitatively shows that, in patients with moderate-to-severe AD, abrocitinib improves overall work productivity in a sequential process beginning with treatment effects on itch, which translate into improvement in sleep that eventually manifests as lesser impairment in work productivity.
This analysis was limited by its post hoc nature and the relatively small and varied number of observations for employed patients in the mediation model (53.7%–98.5% of total sample size). In addition, the contribution of factors (other than itch) to sleep disturbance, such as increased monoamine and cytokine dysregulation, and decreased melatonin and skin temperature [44], were not considered, although one may argue that at least some of the effects mediated by these additional variables may be accounted for within itch. Furthermore, this model does not explore dose relationships.
5 Conclusions
In JADE MONO-2, the relationships between itch and sleep outcomes and between itch and work productivity were approximately linear, demonstrating that reduction in itch severity was associated with improved sleep and work productivity [45]. Empirical evidence for the mechanism of action of abrocitinib suggests that the effect of abrocitinib on work productivity is predominantly mediated by an indirect path wherein treatment with abrocitinib improves itch severity, which reduces sleep loss/sleep disturbance that, in turn, improves work productivity. Future research using data from clinical studies with longer duration of treatment may expand these observations.
References
Silverberg JI, Hanifin JM. Adult eczema prevalence and associations with asthma and other health and demographic factors: a US population-based study. J Allergy Clin Immunol. 2013;132(5):1132–8.
Williams H, Robertson C, Stewart A, Aït-Khaled N, Anabwani G, Anderson R, et al. Worldwide variations in the prevalence of symptoms of atopic eczema in the International Study of Asthma and Allergies in Childhood. J Allergy Clin Immunol. 1999;103(1 Pt 1):125–38.
Chiesa Fuxench ZC, Block JK, Boguniewicz M, Boyle J, Fonacier L, Gelfand JM, et al. Atopic Dermatitis in America Study: a cross-sectional study examining the prevalence and disease burden of atopic dermatitis in the US adult population. J Invest Dermatol. 2019;139(3):583–90.
Silverberg JI, Gelfand JM, Margolis DJ, Boguniewicz M, Fonacier L, Grayson MH, et al. Patient burden and quality of life in atopic dermatitis in US adults: a population-based cross-sectional study. Ann Allergy Asthma Immunol. 2018;121(3):340–7.
Boguniewicz M, Fonacier L, Guttman-Yassky E, Ong PY, Silverberg J, Farrar JR. Atopic dermatitis yardstick: practical recommendations for an evolving therapeutic landscape. Ann Allergy Asthma Immunol. 2018;120(1):10-22.e2.
Barbarot S, Auziere S, Gadkari A, Girolomoni G, Puig L, Simpson EL, et al. Epidemiology of atopic dermatitis in adults: results from an international survey. Allergy. 2018;73(6):1284–93.
Werfel T, Allam JP, Biedermann T, Eyerich K, Gilles S, Guttman-Yassky E, et al. Cellular and molecular immunologic mechanisms in patients with atopic dermatitis. J Allergy Clin Immunol. 2016;138(2):336–49.
de Bruin-Weller M, Gadkari A, Auziere S, Simpson EL, Puig L, Barbarot S, et al. The patient-reported disease burden in adults with atopic dermatitis: a cross-sectional study in Europe and Canada. J Eur Acad Dermatol Venereol. 2020;34(5):1026–36.
Ramirez FD, Chen S, Langan SM, Prather AA, McCulloch CE, Kidd SA, et al. Association of atopic dermatitis with sleep quality in children. JAMA Pediatr. 2019;173(5): e190025.
Silverberg JI, Garg NK, Paller AS, Fishbein AB, Zee PC. Sleep disturbances in adults with eczema are associated with impaired overall health: a US population-based study. J Invest Dermatol. 2015;135(1):56–66.
Sack R, Hanifin J. Scratching below the surface of sleep and itch. Sleep Med Rev. 2010;14(6):349–50.
Fishbein AB, Vitaterna O, Haugh IM, Bavishi AA, Zee PC, Turek FW, et al. Nocturnal eczema: review of sleep and circadian rhythms in children with atopic dermatitis and future research directions. J Allergy Clin Immunol. 2015;136(5):1170–7.
Girolomoni G, Luger T, Nosbaum A, Gruben D, Romero W, Llamado LJ, et al. The economic and psychosocial comorbidity burden among adults with moderate-to-severe atopic dermatitis in Europe: analysis of a cross-sectional survey. Dermatol Ther (Heidelb). 2020;11(1):117–30.
Whiteley J, Emir B, Seitzman R, Makinson G. The burden of atopic dermatitis in US adults: results from the 2013 National Health and Wellness Survey. Curr Med Res Opin. 2016;32(10):1645–51.
Eckert L, Gupta S, Amand C, Gadkari A, Mahajan P, Gelfand JM. Impact of atopic dermatitis on health-related quality of life and productivity in adults in the United States: an analysis using the National Health and Wellness Survey. J Am Acad Dermatol. 2017;77(2):274-9.e3.
Yano C, Saeki H, Ishiji T, Ishiuji Y, Sato J, Tofuku Y, et al. Impact of disease severity on work productivity and activity impairment in Japanese patients with atopic dermatitis. J Dermatol. 2013;40(9):736–9.
Legat FJ. Itch in atopic dermatitis—what is new? Front Med (Lausanne). 2021;8:644760.
Langan SM, Irvine AD, Weidinger S. Atopic dermatitis. Lancet. 2020;396(10247):345–60.
Sutaria N, Adawi W, Goldberg R, Roh YS, Choi J, Kwatra SG. Itch: pathogenesis and treatment. J Am Acad Dermatol. 2022;86(1):17–34.
Kwatra SG, Misery L, Clibborn C, Steinhoff M. Molecular and cellular mechanisms of itch and pain in atopic dermatitis and implications for novel therapeutics. Clin Transl Immunol. 2022;11(5): e1390.
Misery L. Sleep disturbance and psoriasis. J Eur Acad Dermatol Venereol. 2022;36(5):633.
Cheng FL, An YF, Han ZQ, Li C, Li ZQ, Yang PC, et al. Period2 gene regulates diurnal changes of nasal symptoms in an allergic rhinitis mouse model. Int Forum Allergy Rhinol. 2020;10(11):1236–48.
Chang YS, Chiang BL. Sleep disorders and atopic dermatitis: A 2-way street? J Allergy Clin Immunol. 2018;142(4):1033–40.
Cibinqo 100 mg film-coated tablets. Summary of product characteristics. Kent: Pfizer Limited; 2021. (09/10/2021).
Japan's MHLW approves Pfizer’s Cibinqo® (abroctinib) for adults and adolescents with moderate to severe atopic dermatitis. New York: Pfizer, Inc.; 2021.
European Medicines Agency. Cibinqo® (abrocitinib). Summary of Product Characteristics (SmPC). Belgium: Pfizer Europe MA EEIG; 2021. (12/2021).
Cibinqo (abrocitinib) tablets, for oral use. Prescribing information. New York: Pfizer Inc; 2023. (02/2023).
Gooderham MJ, Forman SB, Bissonnette R, Beebe JS, Zhang W, Banfield C, et al. Efficacy and safety of oral Janus kinase 1 inhibitor abrocitinib for patients with atopic dermatitis: a phase 2 randomized clinical trial. JAMA Dermatol. 2019;155(12):1371–9.
Simpson EL, Sinclair R, Forman S, Wollenberg A, Aschoff R, Cork M, et al. Efficacy and safety of abrocitinib in adults and adolescents with moderate-to-severe atopic dermatitis (JADE MONO-1): a multicentre, double-blind, randomised, placebo-controlled, phase 3 trial. Lancet. 2020;396(10246):255–66.
Silverberg JI, Simpson EL, Thyssen JP, Gooderham M, Chan G, Feeney C, et al. Efficacy and safety of abrocitinib in patients with moderate-to-severe atopic dermatitis: a randomized clinical trial. JAMA Dermatol. 2020;156(8):863–73.
Bieber T, Simpson EL, Silverberg JI. Abrocitinib versus placebo and dupilumab for atopic dermatitis. N Engl J Med. 2021;384(12):1101–12.
Eichenfield LF, Flohr C, Sidbury R. Efficacy and safety of abrocitinib in combination with topical therapy in adolescents with moderate-to-severe atopic dermatitis: results from JADE TEEN. J Dermatol. 2021;157(10):1165–73.
Blauvelt A, Silverberg JI, Lynde CW, Bieber T, Eisman S, Zdybski J, et al. Abrocitinib induction, randomized withdrawal, and retreatment in patients with moderate-to-severe atopic dermatitis: results from the JAK1 Atopic Dermatitis Efficacy and Safety (JADE) REGIMEN phase 3 trial. J Am Acad Dermatol. 2022;86(1):104–12.
Thaci T, Bieber T, Simpson EL, Silverberg JI, Paul C, Sinclair R. A phase 3 study to investigate the efficacy and safety of abrocitinib and dupilumab in comparison with placebo in adults with moderate-to-severe atopic dermatitis. 29th EADV Congress. Virtual; 2020.
Yosipovitch G, Fonacier L, Ständer S, Su J, Gooderham M, Szepietowski J, et al. Pruritus, sleep, and productivity: a post hoc analysis of abrocitinib versus placebo in patients with moderate-to-severe atopic dermatitis (AD) from JADE MONO-2. J Allergy Clin Immunol. 2021;147(2, Supplement):AB34.
Yosipovitch G, Reaney M, Mastey V, Eckert L, Abbe A, Nelson L, et al. Peak Pruritus Numerical Rating Scale: psychometric validation and responder definition for assessing itch in moderate-to-severe atopic dermatitis. Br J Dermatol. 2019;181(4):761–9.
Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. 2nd ed. Hoboken: Wiley; 2011.
Bushmakin AG, Cappelleri JC. A practical approach to quantitative validation of patient-reported outcomes: a simulation-based guide using SAS. Hoboken: Wiley; 2022.
Iacobucci D. Mediation analysis. Thousand Oaks: SAGE Publications, Inc.; 2008.
Matterne U, Apfelbacher CJ, Loerbroks A, Schwarzer T, Buttner M, Ofenloch R, et al. Prevalence, correlates and characteristics of chronic pruritus: a population-based cross-sectional study. Acta Derm Venereol. 2011;91(6):674–9.
Carskadon MA, Acebo C, Jenni OG. Regulation of adolescent sleep: implications for behavior. Ann N Y Acad Sci. 2004;1021:276–91.
Fuligni AJ, Chiang JJ, Tottenham N. Sleep disturbance and the long-term impact of early adversity. Neurosci Biobehav Rev. 2021;126:304–13.
Institute of Medicine Committee on Sleep Medicine and Research. The National Academies Collection: reports funded by National Institutes of Health. In: Colten HR, Altevogt BM, editors. Sleep disorders and sleep deprivation: an unmet public health problem. Washington: National Academies Press (US) National Academy of Sciences; 2006.
Lavery MJ, Stull C, Kinney MO, Yosipovitch G. Nocturnal pruritus: the battle for a peaceful night’s sleep. Int J Mol Sci. 2016;17(3):425.
Cappelleri JC, Zou KH, Bushmakin AG, Ma J, Alemayehu D, Symonds T. Patient-reported outcomes: measurement, implementation and interpretation. Chapman and Hall/CRC Press; 2013.
Acknowledgments
This study was sponsored by Pfizer Inc. Editorial/medical writing support under the guidance of the authors was provided by Susanna Bae, PharmD (ApotheCom, San Francisco, CA, USA) and was funded by Pfizer Inc., New York, NY, USA, in accordance with Good Publication Practice (GPP 2022) guidelines (Ann Intern Med. 2015;163:461-464).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was sponsored by Pfizer, Inc.
Conflict of Interest
Gil Yosipovitch is a consultant and advisor for Cara Therapeutics, Eli Lilly, Escient, Galderma, GlaxoSmithKline, Kiniksa, LEO Pharma, Novartis, Pfizer Inc., Regeneron, Sanofi, Trevi Therapeutics, and Vifor and a principal investigator for Arcutis, Celldex, Eli Lilly, Escient, Galderma, Kiniksa, LEO Pharma, Novartis, Pfizer Inc., and Sanofi Regeneron. Melinda J. Gooderham has received grants, personal fees, honoraria, and/or nonfinancial support from AbbVie, Amgen, AkrosPharma, AnaptysBio, Arcutis, ASLAN Pharmaceuticals, Bausch Health (Valeant), Bristol Myers Squibb, Boehringer-Ingelheim, Celgene, Dermavant Sciences, Dermira, Eli Lilly, Galderma, Janssen, Kyowa Kirin, LEO Pharma, MedImmune, Meiji, Merck, Novartis, Pfizer Inc., Roche, Sanofi Genzyme, Regeneron, Sun Pharma, and UCB. Sonja Ständer is a principal investigator for Almirall, Dermasence, Galderma, Kiniksa, LEO Pharma, Menlo Therapeutics, Novartis, Sanofi, and Trevi Therapeutics; a member of scientific advisory boards for Beiersdorf, Celgene, Galderma, Kiniksa, Pfizer, and Trevi Therapeutics; and a consultant for Bellus Health, Galderma, Novartis, Sanofi, and Vifor. Luz Fonacier received research grants (made to NYU Langone Hospital-LI) from AstraZeneca, Pfizer, Regeneron, and Shire and was a consultant and advisor for AbbVie, Eli Lilly, Pfizer, and Regeneron. Jacek C. Szepietowski has been a consultant/advisory board member for LEO Pharma, Novartis, Sanofi Genzyme, Trevi, and Viofor; a speaker for AbbVie, LEO Pharma, Novartis, Sanofi Genzyme, and Sunfarm; and an investigator for AbbVie, Bristol Myers Squibb, Galapagos, Galderma, Helm, Incyte, InfaRX, Janssen-Cilag, Novartis, Pfizer, Regeneron, UCB, and Trevi. Mette Deleuran has been a principal investigator in clinical trials and an advisory board member and/or speaker for AbbVie, ASLAN, Arena Pharmaceuticals, Eli Lilly, Incyte, La Roche Posay, LEO Pharma, Novartis, Pfizer, Pierre Fabre, Regeneron, and Sanofi Genzyme. Giampiero Girolomoni has been principal investigator in clinical trials sponsored by and/or has received personal fees from AbbVie, Almirall, Amgen, Biogen, Boehringer-Ingelheim, Bristol Myers Squibb, Celgene, Eli Lilly, Fresenius Kabi, Genzyme, LEO Pharma, Menlo Therapeutics, Novartis, OM Pharma, Pfizer, Regeneron, Samsung Bioepis, and Sanofi. John Su has received grants/research funding for his role as an investigator for AbbVie, Amgen, AstraZeneca, Bristol Myers Squibb, Eli Lilly, Galderma, Janssen, Novartis, Pfizer Inc., Pierre Fabre, and Sanofi; has received honoraria for serving on advisory boards for Eli Lilly, GSK, Janssen, LEO Pharma, L’Oréal, Novartis, Pfizer Inc., and Sanofi; and has received honoraria for serving as a speaker for Ego Pharmaceuticals and Pierre Fabre. Andrew G. Bushmakin, Pinaki Biswas, Claire Feeney, Hernan Valdez, Andrew J. Thorpe, Gary Chan, Joseph C. Cappelleri, Marco DiBonaventura, and Daniela E. Myers are employees and shareholders of Pfizer Inc. Ricardo Rojo is a former employee and current shareholder of Pfizer Inc.
Ethics Approval
All study documents and procedures were approved by the appropriate institutional review boards/ethics committees at each study site. The study was conducted in compliance with the ethical principles originating in or derived from the Declaration of Helsinki and in compliance with all International Council for Harmonization Good Clinical Practice Guidelines. All local regulatory requirements were followed. This research was approved by institutional review boards or ethics committees at each study site. An internal review committee monitored the safety of patients throughout the study.
Consent to Participate
All patients provided written informed consent.
Consent to Publish
Not applicable.
Availability of Data and Materials
Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions and exceptions, Pfizer may also provide access to the related individual de-identified participant data. See https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information.
Code Availability
Not applicable.
Author Contributions
Andrew G. Bushmakin, Joseph C. Cappelleri, and Daniela E. Myers contributed to study concept and design. Andrew G. Bushmakin and Joseph C. Cappelleri conducted the statistical analysis of the data. Gil Yosipovitch, Melinda J. Gooderham, Sonja Ständer, Luz Fonacier, Jacek C. Szepietowski, Mette Deleuran, Giampiero Girolomoni, John C. Su, Andrew G. Bushmakin, Joseph C. Cappelleri, Claire Feeney, Gary Chan, Andrew J. Thorpe, Hernan Valdez, Pinaki Biswas, Ricardo Rojo, Marco DiBonaventura, and Daniela E. Myers interpreted the data, provided critical feedback on the manuscript, approved the final manuscript for submission, and are accountable for the accuracy and integrity of the manuscript.
Additional information
Ricardo Rojo: Affiliation at the time this study was conducted.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yosipovitch, G., Gooderham, M.J., Ständer, S. et al. Interpreting the Relationship Among Itch, Sleep, and Work Productivity in Patients with Moderate-to-Severe Atopic Dermatitis: A Post Hoc Analysis of JADE MONO-2. Am J Clin Dermatol 25, 127–138 (2024). https://doi.org/10.1007/s40257-023-00810-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-023-00810-7