Abstract
Background
Melasma is an acquired disorder of hyperpigmentation occurring on the face and predominantly affecting women of childbearing age. It is a chronic, often relapsing condition with a negative impact on quality of life. Current treatments for melasma are unsatisfactory.
Objective
The aim of this article was to conduct an evidence-based review of interventions available for the treatment of melasma.
Methods
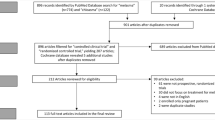
A systematic literature search was performed using PubMed and the keywords ‘melasma’ or ‘chloasma’ in the title. The search was further refined by using a filter for ‘controlled clinical trials’ and ‘randomized controlled trial’. The included studies were used to develop recommendations for treatment.
Results
The electronic search yielded a total of 80 citations. Forty studies were included in this review, which had a total of 2,912 participants. Three different therapeutic modalities were investigated—topical agents, chemical peels, and laser and light therapies. Topical depigmenting agents were found to be the most effective in treating moderate-to-severe melasma, with combination therapies, such as triple-combination therapy (hydroquinone, tretinoin, and fluocinolone acetonide), yielding the best results. Chemical peels as well as laser and light therapies were found to have moderate benefit but more studies are needed to determine their efficacy and long-term safety. Adverse events associated with treatment were mild and short-lasting and included skin irritation, dryness, burning, and erythema. The data could not be statistically pooled because of the heterogeneity of treatments and lack of consistency across study designs.
Conclusions
Topical combination therapies were found to be more effective than monotherapy. Triple combination therapy was found to be the most effective, but approximately 40 % of patients develop erythema and peeling. Chemical peels and laser and light therapies produced mixed results, with increased risk of irritation and subsequent hyperpigmentation, particularly in darker-skinned individuals. Hence, current treatments available for melasma remain unsatisfactory. Many of the studies lacked long-term follow-up. Limitations of current literature include the heterogeneity of study designs, small sample sizes, and poor follow-up rates. Additional evidence for the effects and role of sunscreens is needed. Categorization or stratification of demographic data should also be included in future studies, such as age, melasma type, and duration of melasma prior to initiation of treatment. Patient’s perception of improvement versus investigator’s assessment of improvement should also be included in future studies and standardized methods of study design and assessment of outcomes are needed to form definitive conclusions on the efficacy of different treatment modalities.

Similar content being viewed by others
References
Grimes PE. Melasma: etiologic and therapeutic considerations. Arch Dermatol. 1995;131:1453–7.
Resnik S. Melasma induced by oral contraceptive drugs. JAMA. 1967;199:601–5.
Ponzio HA, Favaretto AL, Rivitti EA. Proposal of a quantitative method to describe melasma distribution in women. J Cosmet Dermatol. 2007;20:103–11.
Pathak MA, Riley FC, Fitzpatrick TB. Melanogenesis in human skin following exposure to long ultraviolet and visible light. J Invest Dermatol. 1962;39:435.
Ortonne JP, Arellano I, Berneburg M, et al. A global survey of the role of ultraviolet radiation and hormonal influences in the development of melasma. J Eur Acad Dermatol Venereol. 2009;23:1254–62.
Sanchez NP, Pathak MA, Sato S. Melasma: a clinical, light microscopic, ultrastructural, and immunofluorescence study. J Am Acad Dermatol. 1981;4:698–709.
Rajaratnam R, Halpern J, Salim A, Emmett C. Interventions for melasma. Cochrane Database Syst Rev. 2010;7(7).
Ennes SBP, Paschoalick RC, De Avelar Alchorne MM. A double-blind comparative placebo-controlled study of the efficacy and tolerability of 4% hydroquinone as a depigmenting agent in melasma. J Dermatol Treat. 2000;11:173–9.
Vázquez M, Sánchez JL. The efficacy of a broad-spectrum sunscreen in the treatment of melasma. Cutis. 1983;32:92–6.
Baliña LM, Graupe K. The treatment of melasma. 20% azelaic acid versus 4% hydroquinone cream. Int J Dermatol. 1991;30:893–5.
Sivayathorn A, Verallo-Rowell V, Graupe K. 20% azelaic acid cream in the topical treatment of melasma: a double- blind comparison with 2% hydroquinone. Eur J Dermatol. 1995;5:680–4.
Farshi S. Comparative study of therapeutic effects of 20% azelaic acid and hydroquinone 4% cream in the treatment of melasma. J Cosmet Dermatol. 2011;10:282–7.
Espinal-Perez LE, Moncada B, Castanedo-Cazares JP. A double-blind randomized trial of 5% ascorbic acid vs. 4% hydroquinone in melasma. Int J Dermatol. 2004;43(8):604–7.
Huh CH, Seo KI, Park JY, Lim JG, Eun HC, Park KC. A randomized, double-blind, placebo-controlled trial of Vitamin C iontophoresis in melasma. Dermatology. 2003;206:316–20.
Khemis A, Kaiafa A, Queille-Roussel C, Duteil L, Ortonne JP. Evaluation of efficacy and safety of rucinol serum in patients with melasma: a randomized controlled trial. Br J Dermaol. 2007;156:997–1004.
Huh SY, Shin JW, Na JI, et al. Efficacy and safety of liposome-encapsulated 4-n-butylresorcinol 0.1% cream for the treatment of melasma: a randomized controlled split-face trial. J Dermatol. 2010;37:311–5.
Thirion L, Pierard-Franchimont C, Pierard G. Whitening effect of a dermocosmetic formulation: a randomized double-blind controlled study on melasma. Int J Cosmet Sci. 2006;28:263–7.
Francisco-Diaz J, Cristi-Cataluna I, Cruz DD, Verallo-Rowell VM. A double-blind randomized placebo controlled trial on the efficacy and safety of botanical extract (Gigawhite® 5% solution) in the treatment of melasma. J Phil Dermatol Soc. 2004;13:18–23.
Ortonne JP. Retinoid therapy of pigmented disorders. Dermatol Ther. 2006;19:280–8.
Romero C, Aberdam E, Larnier C, Ortonne JP. Retinoic acid as modulator of UVB-induced melanocyte differentiation. Involvement of the melanogenic enzymes expression. J Cell Sci. 1994;107:1095–103.
Griffiths CE, Finkel LJ, Ditre CM, Hamilton TA, Ellis CN, Voorhees JJ. Topical tretinoin (retinoic acid) improves melasma. A vehicle-controlled, clinical trial. Br J Dermatol. 1993;129:415–21.
Kimbrough-Green CK, Griffiths CE, Finkel LJ, Hamilton TA, Bulengo-Ransby SM, Ellis CN, et al. Topical retinoic acid (tretinoin) for melasma in black patients. Arch Dermatol. 1994;130:727–33.
Leenutaphong V, Nettakul A, Rattanasuwon P. Topical isotretinoin for melasma in Thai patients: a vehicle-controlled clinical trial. J Med Assoc Thai. 1999;82:868–74.
Kanechorn NA, Niumphradit N, Manosroi A, Nakakes A. Topical 5% tranexamic acid for the treatment of melasma in Asians: a double-blind randomized controlled clinical trial. J Cosmet Laser Ther. 2012;14:150–4.
Lee MH, Kim HJ, Ha DJ, et al. Therapeutic effect of topical of linoleic acid and lincomycin in combination with betamethasone valerate in melasma patients. J Korean Med Sci. 2002;17:518–23.
Alvin G, Catambay N, Vergara A, Jamora MJ. A comparative study of the safety and efficacy of 75% mulberry (Morus alba) extract oil versus placebo as a topical treatment for melasma: a randomized, single-blind, placebo-controlled trial. J Drugs Dermatol. 2011;10:1025–31.
Altaei T. The treatment of melasma by silymarin cream. BMC Dermatol. 2012;12:18.
Taylor SC, Torok H, Jones T, Lowe N, Rich P, Tschen E, et al. Efficacy and safety of a new triple-combination agent for the treatment of facial melasma. Cutis. 2003;72(1):67–72.
Chan R, Park KC, Lee MH, Lee ES, Chang SE, Leow YH, et al. A randomized controlled trial of the efficacy and safety of a fixed triple combination (fluocinolone acetonide 0.01%, hydroquinone 4%, tretinoin 0.05%) compared with hydroquinone 4% cream in Asian patients with moderate to severe melasma. Br J Dermatol. 2008;159:697–703.
Arellano I, Cestari T, Ocampo-Candiani J, et al. Preventing melasma recurrence: prescribing a maintenance regimen with an effective triple combination cream based on long-lasting clinical severity. J Eur Acad Dermatol Venereol. 2012;26(5):611–8.
Guevara IL, Pandya AG. Safety and efficacy of 4% hydroquinone combined with 10% glycolic acid, antioxidants, and sunscreen in the treatment of melasma. Int J Dermatol. 2003;42(12):966–72.
Lim JT. Treatment of melasma using kojic acid in a gel containing hydroquinone and glycolic acid. Dermatol Surg. 1999;25(4):282–4.
Lim JT, Tham SN. Glycolic acid peels in the treatment of melasma among Asian women. Dermatol Surg. 1997;23:177–9.
Hurley ME, Guevara IL, Gonzales RM, Pandya AG. Efficacy of glycolic acid peels in the treatment of melasma. Arch Dermatol. 2002;138:1578–82.
Faghihi G, Shahingohar A, Siadat AH. Comparison between 1% tretinoin peeling versus 70% glycolic acid peeling in the treatment of female patients with melasma. J Drugs Dermatol. 2011;10(12):1439–42.
Ilknur T, Bicak MU, Demirtasoglu M, et al. Glycolic acid peels versus amino fruit acid peels in the treatment of melasma. Dermatol Surg. 2010;36(4):490–5.
Ejaz A, Raza N, Iftikhar N, Muzzafar F. Comparison of 30% salicylic acid with Jessner’s solution for superficial chemical peeling in epidermal melasma. J Coll Physicians Surg Pak. 2008;18:205–8.
Kodali S, Guevara IL, Carrigan CR, et al. A prospective, randomized, split-face, controlled trial of salicylic acid peels in the treatment of melasma in Latin American women. J Am Acad Dermatol. 2010;63(6):1030–5.
Azzam OA, Leheta TM, Naqui NA, Shaarawy E, Hay RM, Hilal RF. Different therapeutic modalities for the treatment of melasma. J Cosmet Dermatol. 2009;8(4):275–81.
Wang CC, Hui CY, Sue YM, Wong WR, Hong HS. Intense pulsed light for the treatment of refractory melasma in Asian persons. Dermatol Surg. 2004;30(9):1196–200.
Goldman MP, Gold MH, Palm MD, et al. Sequential treatment with triple combination cream and intense pulsed light is more efficacious than sequential treatment with an inactive (control) cream and intense pulsed light in patients with moderate to severe melasma. Dermatol Surg. 2011;37(2):224–33.
Figueiredo SL, Trancoso SS. Single-session intense pulsed light combined with stable fixed-dose triple combination topical therapy for the treatment of refractory melasma. Dermatol Ther. 2012;25:477–80.
Wattanakrai P, Mornchan R, Eimputh S. Low-fluence Q-switched neodymium-doped yttrium aluminum garnet (1,064 nm) laser for the treatment of facial melasma in Asians. Dermatol Surg. 2012;36:76–87.
Park KY, Kim DH, Kim HK, et al. A randomized, observer-blinded, comparison of combined 1064-nm Q-switched neodymium-doped yttrium-aluminum-garnet laser plus 30% glycolic acid peel vs. laser monotherapy to treat melasma. Clin Exp Dermatol. 2011;36:864–70.
Kar HK, Gupta L, Chauhan A. A comparative study on efficacy of high and low fluence Q-switched Nd:YAG laser and glycolic acid peel in melasma. Indian J Dermatol Venereol Leprol. 2012;78:165–71.
Passeron T, Fontas E, Kang HY, et al. Melasma treatment with pulsed-dye laser and triple combination cream: a prospective, randomized, single-blind, split-face study. Arch Dermatol. 2011;147:1106–8.
Hong SP, Han SS, Choi SJ, et al. Split-face comparative study of 1550 nm fractional photothermolysis and trichloracetic acid 15% chemical peeling for facial melasma in Asian skin. J Cosmet Laser Ther. 2012;14:81–6.
Wind BS, Kroon MW, Meesters AA, et al. Non-ablative 1,550 nm fractional laser therapy versus triple topical therapy for the treatment of melasma: a randomized controlled split-face study. Lasers Surg Med. 2010;42:607–12.
Kroon MW, Wind BS, Beek JF, et al. Nonablative 1550-nm fractional laser therapy versus triple topical therapy for the treatment of melasma: a randomized controlled pilot study. J Am Acad Dermatol. 2011;64:516–23.
Lynde CB, Kraft JN, Lynde CW. Topical treatments for melasma and postinflammatory hyperpigmentation. Skin Therapy Lett. 2006;11:1–6.
Pandya AG, Hynan LS, Bhore R, et al. Reliability assessment and validation of the Melasma Area and Severity Index (MASI) and a new modified MASI scoring method. J Am Acad Dermatol. 2011;64:78–83.
Acknowledgments
No sources of funding were used to prepare this article. Dr Pandya receives consulting fees from Galderma for his role in the Pigmentary Disorders Academy. The authors have no other conflicts of interest that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rivas, S., Pandya, A.G. Treatment of Melasma with Topical Agents, Peels and Lasers: An Evidence-Based Review. Am J Clin Dermatol 14, 359–376 (2013). https://doi.org/10.1007/s40257-013-0038-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-013-0038-4