Abstract
Atrial fibrillation (AF) is the most prevalent cardiac arrhythmia, affecting approximately 335 million patients worldwide. Comprehensive pharmacological treatment of AF includes medications for rate or rhythm control and anticoagulants to reduce the risk of thromboembolism; yet, these agents have significant limitations. Oral anti-arrhythmic agents have a slow onset of action, and rapid onset formulations require hospitalization for intravenous therapy. Orally administered drugs also require high doses to attain therapeutic levels, and thus dose-related severe adverse effects are often unavoidable. Given the therapeutic benefits of inhaled drug delivery, including rapid onset of action and very low doses to achieve therapeutic efficacy, this review will discuss the benefits of novel pulmonary delivery of drugs for the management of AF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Atrial fibrillation (AF) is an exceedingly common cardiac arrhythmia associated with increased mortality and decreased quality of life. |
Currently available medication delivery systems are inefficient and associated with dose-related adverse effects. |
Pulmonary drug delivery is a novel delivery technology and provides effective therapeutic benefits at a very low dose of the delivered drug. |
Direct delivery of drug into lungs can be used for management of AF with rapid onset of action and significantly reduced dose-related adverse effects. |
1 Introduction
Atrial fibrillation (AF) is the most prevalent cardiac arrhythmia worldwide and is associated with increased mortality and decreased quality of life through its complications such as heart failure and stroke [1, 2]. It has been reported that more than 335 million people are suffering from AF globally [3]. More importantly, the incidence is rapidly rising owing to changing lifestyles and an increasingly aging global population. AF results from abnormal electrical impulses in the atria, and the passing of these irregular signals to the ventricles results in a rapid and abnormal heartbeat. While the exact cause of AF is uncertain, common risk factors include coronary artery disease, hypertension, cardiomyopathies and valvular heart disease, along with other comorbidities that impact the heart. Contemporary drug management of AF using currently available oral anti-arrhythmic drugs has a relatively slow onset of action, which reduces their effectiveness for management of acute episodes of rapid AF, while rapid-onset intravenous formulations often require hospitalization and intravenous cannulation for drug administration and monitoring of adverse effects. AF can lead to thromboembolic phenomena such as stroke or myocardial infarction [4]. Oral vitamin K antagonist (warfarin) and novel non-vitamin K antagonist oral anticoagulant (NOAC) drugs substantially reduce the risk of thrombus formation and clinical sequalae such as stroke [5,6,7]. The use of these drugs in clinical practice remains challenging as long-term use of oral anticoagulants has the potential to cause dose-related gastrointestinal bleeding and fatal intracranial hemorrhage. To overcome these limitations and complexities, an alternative drug delivery system, such as the pulmonary route of anti-arrhythmic and anticoagulant delivery, may be considered, as this route of drug delivery can produce rapid onset of action and efficient therapeutic benefits at very low doses [8, 9]. Pulmonary drug delivery avoids first-pass metabolism of drugs and any associated toxicities typical to oral dosage forms. The inhaled drug delivery system may also be used as an efficient route for delivering drugs, having systemic activity owing to the lungs’ large surface area, with thin vasculature for drug absorption, and therapeutic action at a greatly low dose. Therefore, this mini-review will briefly discuss the pathophysiology of AF as well as the available treatment options and their limitations. Finally, it will highlight and discuss the benefits of inhaled drug delivery for improved therapeutic benefits in AF at a much lower dose compared with those required for oral drug delivery.
2 Pathophysiology
Emerging evidence suggests that several pathophysiological mechanisms may underlie AF, including structural and electrical abnormalities, tissue remodeling and inflammation [10]. It is well recognized that when the atrial tissue develops electrical or structural defects, the atrial contractions become irregular, with an uncoordinated flow of blood into the ventricles. Thus, AF can contribute to large variations in blood pressure and cardiac output. Furthermore, several triggers, like single rapidly firing foci in the atria, may cause AF [10], which ultimately produces fibrillatory conduction through the heart [10]. Several studies have reported that this rapid focus firing occurs most frequently in the pulmonary veins, which can instigate repetitive firing or, in some cases, episodic re-entrant activation of the foci in the veins [11]. The exact mechanisms underlying AF initiation due to rapid firing have not been well understood; however, they may involve increased automaticity, micro-reentry or triggered activity [12]. Additionally, the focal rapid firing activity in the atria seems to be the cause of paroxysmal AF and is the rationale behind pulmonary vein isolation as a treatment option. Fibrosis in the atria was reported to create abnormal substrates that can further prolong AF and promote ectopic activity and/or re-entry [13], which can potentially induce the creation of re-entrant circuits that will further propagate AF. Moreover, electrophysiological changes can also occur within minutes of AF onset, shortening the refractory period and increasing the likelihood of persistent AF. Multiple risk factors have been identified to increase the risk of AF, including genetic factors, obesity, extreme endurance exercise and alcohol and caffeine consumption [10].
3 Pharmacotherapy and Limitations of Current Treatment
3.1 Antiarrhythmic Drugs
Pharmacological agents in the management of AF focus on controlling the ventricular response rate or restoring normal sinus rhythm. Controlling ventricular rate with atrioventricular nodal-blocking agents such as digoxin, beta-blockers and calcium channel blockers is most commonly used in patients with persistent or chronic AF with minimal symptoms. Nevertheless, oral formulations of these drugs have a relatively slow onset of action and patients frequently require intravenous loading doses to rapidly achieve therapeutic levels. For example, oral loading of digoxin is recommended over 7–10 days, while intravenous loading typically required 1 g over 24 h in divided doses. Moreover, digoxin requires monitoring of therapeutic levels, owing to safety concerns, and hospitalization due to toxicity remains common [15][15]. Similarly, oral beta-blockers and calcium channel blockers have relatively slow onsets of action and time and have high first-pass metabolism, and peak plasma concentrations vary widely among individuals. Intravenous formulations offer more rapid onset of action, yet, require intravenous access, hospitalization and cardiac monitoring for adverse events such as bradycardia.
Restoring normal sinus rhythm is often used for new-onset AF or in those who have ongoing symptoms despite rate control, whereby antiarrhythmic drugs such as flecainide, amiodarone and sotalol are used in an attempt to revert and maintain sinus rhythm and alleviate symptoms [14]. Among these, flecainide, a sodium channel blocker, has a promising safety profile in AF patients without structural heart disease [18]. Oral administration has bioavailability of around 90–95% and will achieve cardioversion at a rate of 50–60% and 75–85% at 3 h and 6–8 h, respectively, and 100-mg oral tablets have a peak plasma concentration of 0.138 μg/mL in 3.36 h [20, 21], which is a very long onset of action. Oral flecainide undergoes remarkable first-pass metabolism, which reduces its therapeutic potential [19]. Amiodarone can be used in those with structural heart disease, but has poor oral bioavailability, with extensive inter-subject variation [23]. The first-pass metabolism in the gut and liver is responsible for determining the systematic bioavailability. The remaining unused drug accumulates in tissues, particularly the adipose tissue, and in highly perfused organs such as the liver, lung, kidney, spleen and heart and causes toxic effects such as pulmonary fibrosis with long-term use [24,25,26]. A typical 200-mg oral tablet can reach a peak plasma concentration of 0.1437 μg/mL in up to 7.6 h [23]. Intravenous loading and infusions are often required to ensure rapid antiarrhythmic effects, with reversion rates of 95% with high-dose (> 1500 mg/day) intravenous loading and infusion [14].
Sotalol inhibits the inward potassium ion channels and extends the duration of action potential and refractory periods [29]. Sotalol is also a non-selective beta-blocker that reduces the rate and force of contraction [29]. When administered orally in the form of 80- to 120-mg tablets, the bioavailability is 90–100%, with an elimination half-life of 12 h [30,31,32]. An oral tablet with an 80-mg dose will achieve a peak plasma concentration of 0.61 ± 0.16 μg/mL in 2.12 h [31]. Due to this drug’s non-selective beta-blocking action, adverse effects such as bronchospasms, excessive bradycardia and pro-arrhythmias such as torsades de pointes can result [30, 31].
3.2 Anticoagulation Therapy
Warfarin and NOACs are widely prescribed for the prevention of stroke in patients with non-valvular AF (NVAF) [15]. The marketed NOACs include apixaban, dabigatran, edoxaban and rivaroxaban, which are available in a range of doses for a range of indications. However, the use of these anticoagulants with currently available dosage forms is associated with limited effectiveness and an increased risk of dose-related major bleeding [1, 2, 6]. Warfarin is recommended in clinical guidelines for the management of valvular AF and NVAF although long-term use requires frequent blood tests and involves the difficulty of achieving stable international normalized ratios, making therapy complex for physicians and patients. Due to the potential risk of blood clots and stroke associated with different types of NVAF, it is not clear whether the direct oral anticoagulants can replace warfarin [7].
3.3 Limitations of Current Treatment
Although current treatment options for AF have been used in clinical practice for an extended period of time, some unavoidable limitations still exist. For example, rate control medications are not always effective in adequately controlling the heart rhythm, and rhythm control medications can fail or worsen arrhythmias in some patients. Catheter ablation of AF is markedly reducing the burden of AF and improves mortality in those with left ventricular dysfunction. Nevertheless, ablation is invasive and is associated with a clinically significant risk of early complications [16]. Moreover, about half of patients undergoing AF ablation have recurrence of AF of sufficient severity to warrant re-hospitalization over time; thus, this is not a cure or replacement for pharmacological therapy [17]. Furthermore, anticoagulation reduces but does not eliminate the embolic risk of AF [6] and is associated with a risk of bleeding [18]. While left atrial appendage closure devices can reduce the risk of embolic events in NVAF without using anticoagulation, they are associated with a risk of serious adverse events [19] and are generally recommended only for those who have an appropriate reason to seek a nondrug alternative. Therefore, additional research with newer agents and/or better delivery systems for existing drugs may improve the effectiveness of these currently approved drugs for the management of AF.
4 Advanced Drug Delivery Technology for AF
Studies in developing advanced drug delivery technology have not progressed for the treatment of AF. The sub-optimal nature of current treatment strategies for AF presents the need to develop more efficient and advanced options that may help to eliminate some of the many adverse effects seen by traditional therapy. Recently, cardiovascular gene therapy has been explored as a potential alternative over typical drugs and catheter-based ablation therapies. Several gene therapy targets have already been identified as relevant to the control of rate or rhythm of the heart during AF. For rate control, through genetic modification of the atrioventricular node, there is a proposed reduced conduction and thus ventricular response rate to AF [4]. The proposed vector would be delivered by arterial perfusion, which is desirable as there is minimal invasiveness and the method is practical with current standard clinical approaches. A disadvantage, however, is the limited efficacy involved with whole nodal transduction [4]. Rhythm control through modification of atrial muscle to become a substrate less supportive of AF has also been investigated [20]. Many studies so far have been conducted in large animal models, making the easy transition to human studies more promising than the outcomes obtained from small animals. However, the vector used (such as adenovirus) can present limitations such as the induction of strong inflammatory responses and subsequent clearance of the vector and limits gene expression [4].
5 Pulmonary Drug Delivery Technology and Advantages
Pulmonary drug delivery technology is the most suitable route of drug administration as it delivers drugs deep into the lungs, avoids first-pass metabolism and produces therapeutic benefits at a very low dose of the delivered drugs (Fig. 1). Currently, oral medications for the management of AF have a relatively slow onset of action and are also associated with dose-related adverse effects. There are three main categories of device available for lung delivery of drugs, i.e., metered dose inhalers (MDIs) (Fig. 1a), dry powder inhalers (DPIs) (Fig. 1b) and nebulizers. The MDI formulations are solutions or suspensions of drugs in liquified hydrofluoroalkane or propellant. The DPI formulations consist of either the agglomerated forms of the micronized drug particles (< 5 µm) with controlled flow properties or the large carrier-based powder mixtures. The micronized drug particles (< 5 µm) are highly cohesive with reduced flowability, which affects the aerosolization performance of the powder. Therefore, large carriers (preferably lactose powder) are used to enhance the flowability of the formulations. The nebulizer formulations are aqueous solutions or suspensions of drugs, which are delivered as a large dose. As presented in Fig. 1, the lung-deposited drug can be translocated into the heart through the air–blood pulmonary barrier, avoiding first-pass metabolism and any associated toxicities typical to oral ingestion. Furthermore, the profuse vascular nature of the lungs, as well as relatively low levels of proteolytic enzymes, presents the opportunity for the drug to enter the systemic system more rapidly at very low doses compared to those required for oral delivery [21]. A successful drug would have both an appropriate inhalable formulation [22, 23] and stable aerodynamic properties [24]. Factors such as the varying anatomy between human respiratory tracts, inhalation flow rate and drug particle size (< 5 µm) must also be considered for the efficient delivery of drug. The drug particle size must be < 5 µm for efficient delivery of the drug deep into lungs for appropriate absorption. Effective drug delivery to the lungs using inhaled formulations is dependent on the drug particle formulation, the delivery device and the patient’s inhalation force.
6 Inhaled Drugs for the Management of AF
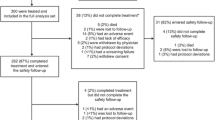
The inhaled route, with potential advantages for delivering antiarrhythmic drugs for rapid conversion of AF, is progressing [25]. Preclinical and clinical studies of the inhaled drugs for potential application in the management of AF are summarized in Table 1.
Among the antiarrhythmic drugs, flecainide is the most investigated drug for pulmonary delivery, with significant success in preclinical studies [25,26,27,28,29,30]. Tessarolo et al. demonstrated that the intratracheal instillation of flecainide rapidly terminated AF through multimodal effects such as slowing down of atrial conduction velocity and decreasing AF frequency at a reduced dose [31]. Inhaled cyclodextrin complexed flecainide formulation was found to accelerate the conversion of AF to sinus rhythm in a dose-dependent mode and shortened the duration of AF. The authors suggested that flecainide complexed with cyclodextrin formulation effectively terminated AF by slowing down the atrial conduction velocity as well as decreasing the frequency of AF. The peak plasma level of flecainide complexed cyclodextrin formulation was achieved within 2 min of intratracheal instillation. The authors emphasized that the rapid increase in plasma drug levels upon inhalation optimized its anti-AF effects at a low dose, with reduced adverse effects versus an oral formulation. These excellent outcomes proved the applicability of inhaled formulations for the efficient management of AF. Intratracheal instillation of this drug in Yorkshire pigs showed fast absorption of the delivered drug and increased the concentration of drug in pulmonary veins and the left atrium, resulting in the termination of AF [26]. Marum et al. [29] investigated the reduction of AF by rapid administration of a low dose of flecainide, by intratracheal or intravenous routes in pig models. They found a similar reduction of AF duration with both intratracheal and intravenous administration of the drug. The authors concluded that the rapid delivery (inhalation or intravenous) of a low dose of flecainide optimized the plasma drug concentration profile for effective conversion of AF. In Stocco et al.’s study, low-dose inhaled flecainide was shown to allow flecainide to reach systemic circulation in 2 min, with a pharmacokinetic profile similar to that of an intravenous route. The authors concluded that the inhaled flecainide was safe and well tolerated [28]. The outcomes of the above investigations indicate that the pulmonary delivery of flecainide is a promising avenue in the therapeutic approach for the treatment of AF.
The clinical application of flecainide has recently been investigated in 101 patients with symptomatic onset of AF less than 48 h. An inhaled 120-mg dose produced cardioconversion in 48% of the patients 8 min after the end of inhalation [32]. The peak plasma concentration (386 ± 209 ng/mL) occurred with a 120-mg dose within 3 min of inhalation. This is the first clinical study to reveal that inhaled flecainide has the potential to be a practical application for rapid conversion of AF to sinus rhythm. A comprehensive phase 3 clinical trial (identifier # NCT05039359) involving 400 participants is ongoing, and more data will be published in future.
The pulmonary delivery of the beta-adrenergic blocker metoprolol was found to terminate AF in a pig model [30]. The authors demonstrated that the inhaled metoprolol efficiently reduced the ventricular rate and enhanced conversion to normal sinus rhythm. Additionally, the inhaled metoprolol was also found to reduce AF dominant frequency by 31% compared to that of control (sterile water). Belardinelli et al. patented the inhaled formulations of metoprolol and flecainide for the treatment of heart conditions such as cardiac arrhythmia, atrial arrhythmia and AF [33]. Further details of the inhaled antiarrhythmic drugs for rapid changes of AF have been reported [25].
Recently, inhalation of < 50-nm calcium phosphate (CaP) nanoparticles loaded with a peptide dyed with cyanine 7 (Cy7) was found to show rapid translocation of CaP from the pulmonary tree to the bloodstream and to the myocardium, where the peptide was released very quickly in an animal model [34]. The authors demonstrated that drug administration via inhalation was a more efficient delivery method in the rapid delivery of Cy7-loaded CaP to the myocardium compared to oral and parenteral delivery. Oral delivery did not get the drug into the target 40 min after administration. This is a very encouraging effect of the inhaled drug delivered into the heart via the lungs and is considered a pioneering method for the management of heart diseases. Inhaled amiodarone was found to induce transient pulmonary inflammation with little damage to the lungs of Wistar rats [35]; however, further investigations are warranted to understand the suitability of the inhaled delivery of this drug to overcome the dose-related adverse effects of oral administration.
Pulmonary delivery of anticoagulants was demonstrated to be a safe and beneficial route for treatment [36,37,38]. Very recently, Abdur Rashid et al. developed inhaled edoxaban (EDX), which showed very promising anticoagulation effects at a greatly reduced concentration (3 μg/mL) in 20 min [8]. It can be highlighted that the required therapeutic concentration of 256 ng/mL (0.26 μg/mL), which is obtained from 60 mg of orally administered EDX, can be attained by lung delivery of 208–309 μg of EDX for anticoagulation effect. Lung delivery of heparin for idiopathic pulmonary fibrosis (IPF) is well documented [37]. Inhaled low molecular weight heparin (LMWH) from DPI formulations has been reported as an alternative to multiple parenteral administration [39]. Additionally, the DPI formulation of LMWH showed better absorption compared to that of an inhalable solution formulation [40]. The DPI formulation produced an approximately 1.5-fold increase in the bioavailability (41.6%) compared to the liquid formulation (32.5%). Inhaled anticoagulant therapy in both preclinical and clinical studies was found to increase the survival of the patients and decrease the morbidity [41]. Inhaled heparin was also found to be effective and safe for the patients with asthma and chronic obstructive pulmonary disease (COPD). The pulmonary route for unfractionated heparin delivery was also reported as the most suitable for obtaining anti-inflammatory, antioxidant and mucolytic effects in the patients with asthma and COPD [42].
7 Conclusion
Currently available medications for the management of AF have a relatively slow onset of action and require high doses via the oral route, which causes an increase in drug concentration in the systemic circulation, with considerably long elimination half-lives that together result in dose-related adverse effects. This mini-review has demonstrated the possibility of developing an inhaled drug delivery system for the treatment of AF at very low doses, which potentially can achieve a rapid therapeutic effect and significantly reduce the dose-related adverse effects seen with oral drug delivery. Although preclinical studies and some clinical studies have been performed, wider clinical investigations are warranted to draw a comprehensive conclusion. Based on the evidence presented, we believe that this novel delivery approach will have significantly improved efficacy and clinical outcomes over current strategies in the management of AF.
References
Floria M, Radu S, Gosav EM, Moraru AC, Serban T, Carauleanu A, et al. Cardiac optogenetics in atrial fibrillation: current challenges and future opportunities. BioMed Res Int. 2020;2020:8814092.
Nattel S, Heijman J, Zhou L, Dobrev D. Molecular basis of atrial fibrillation pathophysiology and therapy a translational perspective. Circ Res. 2020;127(1):51–72.
Kirchhof P. The future of atrial fibrillation management: integrated care and stratified therapy. Lancet. 2017;390(10105):1873–87.
Farraha M, Chong JJ, Kizana E. Therapeutic prospects of gene therapy for atrial fibrillation. Heart Lung Circ. 2016;25(8):808–13.
Heijman J, Dobrev D. Challenges to the translation of basic science findings to atrial fibrillation therapies. Future Cardiol. 2016;12(3):251–4.
Heijman J, Guichard J-B, Dobrev D, Nattel S. Translational Challenges in Atrial Fibrillation. Circ Res. 2018;122(5):752–73.
Wu J, Zhang Y, Liao X, Lei Y. Anticoagulation therapy for non-valvular atrial fibrillation: a mini-review. Front Med (Lausanne). 2020;7:350.
Abdur Rashid M, Alhamhoom Y, Muneer S, Izake Emad L, Mendhi J, Zaidur Rahman Sabuj M, et al. Inhaled edoxaban dry powder inhaler formulations: development, characterization and their effects on the coagulopathy associated with COVID-19 infection. Int J Pharm. 2021;608:121122.
Muneer S, Wang T, Rintoul L, Ayoko GA, Islam N, Izake EL. Development and characterization of meropenem dry powder inhaler formulation for pulmonary drug delivery. Int J Pharm. 2020;587: 119684.
Xu J, Luc JGY, Phan K. Atrial fibrillation: review of current treatment strategies. J Thorac Dis. 2016;8(9):E886–900.
Haissaguerre M, Jais P, Shah DC, Takahashi A, Hocini M, Quiniou G, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998;339(10):659–66.
Roten L, Derval N, Jais P. Catheter ablation for persistent atrial fibrillation: elimination of triggers is not sufficient. Circ Arrhythm Electrophysiol. 2012;5(6):1224–32.
Iwasaki Y-K, Nishida K, Kato T, Nattel S. Atrial fibrillation pathophysiology: implications for management. Circulation. 2011;124(20):2264–74.
Khan IA, Mehta NJ, Gowda RM. Amiodarone for pharmacological cardioversion of recent-onset atrial fibrillation. Int J Cardiol. 2003;89(2–3):239–48.
Patti G, Haas S. Non-vitamin K antagonist oral anticoagulants and factors influencing the ischaemic and bleeding risk in elderly patients with atrial fibrillation: a review of current evidence. J Cardiovasc Pharmacol. 2020;77(1):11–21.
Ngo L, Ali A, Ganesan A, Woodman R, Adams R, Ranasinghe I. Ten-year trends in mortality and complications following catheter ablation of atrial fibrillation. Eur Heart J Qual Care Clin Outcomes. 2022;8(4):398–408.
Ngo L, Woodman R, Denman R, Walters TE, Yang IA, Ranasinghe I. Longitudinal risk of death, hospitalisations for atrial fibrillation and cardiovascular events following catheter ablation of atrial fibrillation: a cohort study. Eur Heart J Qual Care Clin Outcomes. 2022; p. 1–11.
Chan NC, Eikelboom JW. How I manage anticoagulant therapy in older individuals with atrial fibrillation or venous thromboembolism. Blood. 2019;133(21):2269–78.
Darden D, Duong T, Du C, Munir MB, Han FT, Reeves R, et al. Sex Differences in Procedural Outcomes Among Patients Undergoing Left Atrial Appendage Occlusion: Insights From the NCDR LAAO Registry. JAMA Cardiol. 2021; 6(11):1275-1284.
Bikou O, Thomas D, Trappe K, Lugenbiel P, Kelemen K, Koch M, et al. Connexin 43 gene therapy prevents persistent atrial fibrillation in a porcine model. Cardiovasc Res. 2011;92(2):218–25.
de Kruijf W, Ehrhardt C. inhalation delivery of complex drugs—the next steps. Curr Opin Pharmacol. 2017;36:52–7.
Islam N, Gladki E. Dry powder inhalers (DPIs)-A review of device reliability and innovation. Int J Pharm. 2008;360(1–2):1–11.
Islam N, Stewart P, Larson I, Hartley P. Effect of carrier size on the dispersion of salmeterol xinafoate from interactive mixtures. J Pharm Sci. 2004;93(4):1030–8.
Forbes B, Asgharian B, Dailey LA, Ferguson D, Gerde P, Gumbleton M, et al. Challenges in inhaled product development and opportunities for open innovation. Adv Drug Deliv Rev. 2011;63(1–2):69–87.
Verrier RL, Belardinelli L. Pulmonary delivery of antiarrhythmic drugs for rapid conversion of new-onset atrial fibrillation. J Cardiovasc Pharmacol. 2020;75(4):276–83.
Verrier RL, Bortolotto AL, Silva BA, Marum AA, Stocco FG, Evaristo E, et al. Accelerated conversion of atrial fibrillation to normal sinus rhythm by pulmonary delivery of flecainide acetate in a porcine model. Heart Rhythm. 2018;15(12):1882–8.
Tessarolo SF, Pedreira GC, Medeiros SA, Bortolotto AL, Araujo SB, Verrier RL, et al. Multimodal mechanisms and enhanced efficiency of atrial fibrillation cardioversion by pulmonary delivery of a novel flecainide formulation. J Cardiovasc Electrophysiol. 2020;31(1):205–13.
Stocco FG, Evaristo E, Silva AC, de Antonio VZ, Pfeiffer J, Rangachari N, et al. Comparative pharmacokinetic and electrocardiographic effects of intratracheal and intravenous administration of flecainide in anesthetized pigs. J Cardiovasc Pharmacol. 2018;72(3):129–35.
Marum AA, Silva BA, Bortolotto AL, Silva AC, de Antonio VZ, Belardinelli L, et al. Optimizing flecainide plasma concentration profile for atrial fibrillation conversion while minimizing adverse ventricular effects by rapid, low-dose intratracheal or intravenous administration. Int J Cardiol. 2019;274:170–4.
Marum AA, Araujo Silva B, Bortolotto AL, Pedreira GC, Tessarolo Silva F, Medeiros SA, et al. Pulmonary delivery of metoprolol reduces ventricular rate during atrial fibrillation and accelerates conversion to sinus rhythm. J Cardiovasc Pharmacol. 2020;75(2):135–40.
Tessarolo Silva F, Pedreira GC, Medeiros SA, Bortolotto AL, Araujo Silva B, Hurrey M, et al. Multimodal mechanisms and enhanced efficiency of atrial fibrillation cardioversion by pulmonary delivery of a novel flecainide formulation. J Cardiovasc Electrophysiol. 2020;31(1):205–13.
Crijns HJGM, Elvan A, Al-Windy N, Tuininga YS, Badings E, Aksoy I, et al. Open-label, multicenter study of flecainide acetate oral inhalation solution for acute conversion of recent-onset, symptomatic atrial fibrillation to sinus rhythm. Circ Arrhythmia Electrophysiol. 2022;15(3):e010204.
Belardinelli L, Narasimhan R, Schuler C, inventors; InCarda Therapeutics, Inc., USA . assignee. Methods of treating or preventing heart rate conditions using selective β-adrenergic blockers and class I antiarrhythmic agents patent WO2019183470A2. 2019.
Miragoli M, Ceriotti P, Iafisco M, Vacchiano M, Salvarani N, Alogna A, et al. Inhalation of peptide-loaded nanoparticles improves heart failure. Sci Transl Med. 2018;10(424):eaan6205/1.
Patel A, Hoffman E, Ball D, Klapwijk J, Steven RT, Dexter A, et al. Comparison of oral, intranasal and aerosol administration of amiodarone in rats as a model of pulmonary phospholipidosis. Pharmaceutics. 2019;11(7):345.
Bandeshe H, Boots R, Dulhunty J, Dunlop R, Holley A, Jarrett P, et al. Is inhaled prophylactic heparin useful for prevention and Management of Pneumonia in ventilated ICU patients? J Crit Care. 2016;34:95–102.
Yildiz-Pekoz A, Ozsoy Y. Inhaled heparin: therapeutic efficacy and recent formulations. J Aerosol Med Pulm Drug Deliv. 2017;30(3):143–56.
Horowitz RI, Freeman PR. Three novel prevention, diagnostic, and treatment options for COVID-19 urgently necessitating controlled randomized trials. Med Hypotheses. 2020;143: 109851.
Rawat A, Majumder QH, Ahsan F. Inhalable large porous microspheres of low molecular weight heparin: in vitro and in vivo evaluation. J Control Release. 2008;128(3):224–32.
Bai S, Gupta V, Ahsan F. Inhalable lactose-based dry powder formulations of low molecular weight heparin. J Aerosol Med Pulm Drug Delivery. 2010;23(2):97–104.
Miller AC, Elamin EM, Suffredini AF. Inhaled anticoagulation regimens for the treatment of smoke inhalation-associated acute lung injury: a systematic review. Crit Care Med. 2014;42(2):413–9.
Shute JK, Puxeddu E, Calzetta L. Therapeutic use of heparin and derivatives beyond anticoagulation in patients with bronchial asthma or COPD. Curr Opin Pharmacol. 2018;40:39–45.
Rabêlo Evangelista AB, Monteiro FR, Nearing BD, Belardinelli L, Verrier RL. Flecainide-induced QRS complex widening correlates with negative inotropy. Heart Rhythm. 2021;18(8):1416–22.
de Antonio VZ, Silva AC, Stocco FG, Silva BA, Marum AA, Bortolotto AL, et al. Pulmonary delivery of flecainide causes a rate-dependent predominant effect on atrial compared with ventricular depolarization duration revealed by intracardiac recordings in an intact porcine model. J Cardiovasc Electrophysiol. 2018;29(11):1563–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. No external funding was used in the preparation of this manuscript.
Conflict of interest
Nazrul Islam, Emma Cichero, Shafiqur Rahman and Isuru Ranasinghe declare that they have no potential conflicts of interest that might be relevant to the contents of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Data availability statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Code availability
Not applicable.
Authors' contributions
Conceptualization: NI, SR and IR. Writing: NI, EC and SR. Reviewing and editing: NI, SR and IR.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Islam, N., Cichero, E., Rahman, S. et al. Novel Pulmonary Delivery of Drugs for the Management of Atrial Fibrillation. Am J Cardiovasc Drugs 23, 1–7 (2023). https://doi.org/10.1007/s40256-022-00551-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-022-00551-8