Abstract
Purpose
This study aimed to investigate the effects of photobiomodulation (PBM) and conditioned medium (CM) derived from human adipose-derived stem cells (h-ASCs), both individually and in combination, on the maturation stage of an ischemic infected delayed healing wound model (IIDHWM) in type I diabetic (TIDM) rats.
Methods
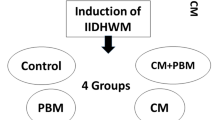
The study involved the extraction of h-ASCs from donated fat, assessment of their immunophenotypic markers, cell culture, and extraction and concentration of CM from cultured 1 × 10^6 h-ASCs. TIDM was induced in 24 male adult rats, divided into four groups: control, CM group, PBM group (80 Hz, 0.2 J/cm2, 890 nm), and rats receiving both CM and PBM. Clinical and laboratory evaluations were conducted on days 4, 8, and 16, and euthanasia was performed using CO2 on day 16. Tensiometrical and stereological examinations were carried out using two wound samples from each rat.
Results
Across all evaluated factors, including wound closure ratio, microbiological, tensiometrical, and stereological parameters, similar patterns were observed. The outcomes of CM + PBM, PBM, and CM treatments were significantly superior in all evaluated parameters compared to the control group (p = 0.000 for all). Both PBM and CM + PBM treatments showed better tensiometrical and stereological results than CM alone (almost all, p = 0.000), and CM + PBM outperformed PBM alone in almost all aspects (p = 0.000). Microbiologically, both CM + PBM and PBM exhibited fewer colony-forming units (CFU) than CM alone (both, p = 0.000).
Conclusion
PBM, CM, and CM + PBM interventions substantially enhanced the maturation stage of the wound healing process in IIDHWM of TIDM rats by mitigating the inflammatory response and reducing CFU count. Moreover, these treatments promoted new tissue formation in the wound bed and improved wound strength. Notably, the combined effects of CM + PBM surpassed the individual effects of CM and PBM.






Similar content being viewed by others
References
Sapra A, Bhandari P. Diabetes. 2023 Jun 21. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan?. PMID: 31855345
Khanolkar M, Bain S, Stephens J. The diabetic foot. QJM: An International Journal of Medicine. 2008;101:685–95.
Armstrong D, Boulton A. Bus SA Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376:2367–75.
Amin N, Doupis J. Diabetic foot disease: from the evaluation of the foot at risk to the novel diabetic ulcer treatment modalities. World J Diabetes. 2016;7:153.
Jeffcoate WJ, Vileikyte L, Boyko EJ, Armstrong DG, Boulton AJ. Current challenges and opportunities in the prevention and management of diabetic foot ulcers. Diabetes Care. 2018;41:645–52.
Prompers L, Schaper N, Apelqvist J, Edmonds M, Jude E, Mauricio D, Uccioli L, Urbancic V, Bakker K, Holstein P. Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. Volume 51. Diabetologia: The EURODIALE Study; 2008. pp. 747–55.
Yang Y, Huang K, Wang M, Wang Q, Chang H, Liang Y, Wang Q, Zhao J, Tang T, Yang S. Ubiquitination Flow Repressors: enhancing Wound Healing of Infectious Diabetic Ulcers through stabilization of Polyubiquitinated Hypoxia-Inducible Factor‐1α by theranostic nitric oxide nanogenerators. Adv Mater. 2021;33:2103593.
Naves CC. The diabetic foot: a historical overview and gaps in current treatment. Adv Wound care. 2016;5:191–7.
Ren G, Peng Q, Fink T, Zachar V, Porsborg SR. Potency assays for human adipose-derived stem cells as a medicinal product toward wound healing. Stem Cell Res Ther. 2022;13:1–11.
McCarthy ME, Brown TA, Bukowska J, Bunnell BA, Frazier T, Wu X, Gimble JM. Therapeutic applications for adipose-derived stem cells in wound healing and tissue engineering. Curr Stem Cell Rep. 2018;4:127–37.
Xiao S, Zhang D, Liu Z, Jin W, Huang G, Wei Z, Wang D, Deng C. Diabetes-induced glucolipotoxicity impairs wound healing ability of adipose-derived stem cells-through the miR-1248/CITED2/HIF-1α pathway. Aging. 2020;12:6947.
Kosaraju R, Rennert RC, Maan ZN, Duscher D, Barrera J, Whittam AJ, Januszyk M, Rajadas J, Rodrigues M, Gurtner GC. Adipose-derived stem cell-seeded hydrogels increase endogenous progenitor cell recruitment and neovascularization in wounds. Tissue Eng Part A. 2016;22:295–305.
Kim W-S, Park B-S, Sung J-H. The wound-healing and antioxidant effects of adipose-derived stem cells. Expert Opin Biol Ther. 2009;9:879–87.
De Gregorio C, Contador D, Díaz D, Cárcamo C, Santapau D, Lobos-Gonzalez L, Acosta C, Campero M, Carpio D, Gabriele C. Human adipose-derived mesenchymal stem cell-conditioned medium ameliorates polyneuropathy and foot ulceration in diabetic BKS db/db mice. Stem Cell Res Ther. 2020;11:1–21.
Brem H, Tomic-Canic M. Cellular and molecular basis of wound healing in diabetes. J Clin Investig. 2007;117:1219–22.
Moradi A, Zare F, Mostafavinia A, Safaju S, Shahbazi A, Habibi M, Abdollahifar MA, Hashemi SM, Amini A, Ghoreishi SK, Chien S, Hamblin MR, Kouhkheil R, Bayat M. Photobiomodulation plus Adipose-derived stem cells improve Healing of Ischemic infected Wounds in type 2 Diabetic rats. Sci Rep. 2020;10:1206.
Ebrahimpour-Malekshah R, Amini A, Zare F, Mostafavinia A, Davoody S, Deravi N, Rahmanian M, Hashemi SM, Habibi M, Ghoreishi SK, Chien S, Shafikhani S, Ahmadi H, Bayat S, Bayat M. Combined therapy of photobiomodulation and adipose-derived stem cells synergistically improve healing in an ischemic, infected and delayed healing wound model in rats with type 1 diabetes mellitus. BMJ open diabetes research & care; 2020. p. 8.
Oyebode O, Houreld NN, Abrahamse H. Photobiomodulation in diabetic wound healing: a review of red and near-infrared wavelength applications. Cell Biochem Funct. 2021;39:596–612.
Park IS. Enhancement of Wound Healing by Conditioned Medium of adipose-derived stromal cell with Photobiomodulation in skin wound. Int J stem Cells. 2021;14:212–20.
Park IS, Chung PS, Ahn JC, Leproux A. Human adipose-derived stem cell spheroid treated with photobiomodulation irradiation accelerates tissue regeneration in mouse model of skin flap ischemia. Lasers Med Sci. 2017;32:1737–46.
Pouriran R, Piryaei A, Mostafavinia A, Zandpazandi S, Hendudari F, Amini A, Bayat M. The effect of combined pulsed wave low-level laser therapy and human bone marrow mesenchymal stem cell-conditioned medium on open skin wound healing in diabetic rats, photomedicine and laser surgery, 34 (2016) 345–54.
Viswanathan V, Pendsey S, Radhakrishnan C, Rege TD, Ahdal J, Jain R. Methicillin-Resistant Staphylococcus aureus in Diabetic Foot infection in India: a growing menace, the international journal of lower extremity wounds, 18 (2019) 236–46.
Naserzadeh P, Hafez AA, Abdorahim M, Abdollahifar MA, Shabani R, Peirovi H, Simchi A, Ashtari K. Curcumin loading potentiates the neuroprotective efficacy of Fe3O4 magnetic nanoparticles in cerebellum cells of schizophrenic rats. Biomed Pharmacother. 2018;108:1244–52.
Mizukami H, Yagihashi S. Exploring a new therapy for diabetic polyneuropathy–the application of stem cell transplantation. Front Endocrinol. 2014;5:45.
Kim W-S, Park B-S, Kim H-K, Park J-S, Kim K-J, Choi J-S, Chung S-J, Kim D-D, Sung J-H. Evidence supporting antioxidant action of adipose-derived stem cells: protection of human dermal fibroblasts from oxidative stress. J Dermatol Sci. 2008;49:133–42.
Caplan AI, Dennis JE. Mesenchymal stem cells as trophic mediators. J Cell Biochem. 2006;98:1076–84.
Prockop DJ, Oh JY. Mesenchymal stem/stromal cells (MSCs): role as guardians of inflammation, Molecular therapy, 20 (2012) 14–20.
Mazini L, Rochette L, Admou B, Amal S, Malka G. Hopes and limits of adipose-derived stem cells (ADSCs) and mesenchymal stem cells (MSCs) in wound healing. Int J Mol Sci. 2020;21:1306.
Kichenbrand C, Velot E, Menu P, Moby V. Dental pulp stem cell-derived conditioned medium: an attractive alternative for regenerative therapy. Tissue Eng Part B: Reviews. 2019;25:78–88.
Kunter U, Rong S, Boor P, Eitner F, Müller-Newen G, Djuric Z, van Roeyen CR, Konieczny A, Ostendorf T, Villa L. Mesenchymal stem cells prevent progressive experimental renal failure but maldifferentiate into glomerular adipocytes. J Am Soc Nephrol. 2007;18:1754–64.
Griffin MD, Ryan AE, Alagesan S, Lohan P, Treacy O, Ritter T. Anti-donor immune responses elicited by allogeneic mesenchymal stem cells: what have we learned so far? Immunol Cell Biol. 2013;91:40–51.
Eggenhofer E, Benseler V, Kroemer A, Popp F, Geissler E, Schlitt H, Baan C, Dahlke M, Hoogduijn M. Mesenchymal stem cells are short-lived and do not migrate beyond the lungs after intravenous infusion. Front Immunol. 2012;3:297.
Kato J, Kamiya H, Himeno T, Shibata T, Kondo M, Okawa T, Fujiya A, Fukami A, Uenishi E, Seino Y. Mesenchymal stem cells ameliorate impaired wound healing through enhancing keratinocyte functions in diabetic foot ulcerations on the plantar skin of rats. J Diabetes Complicat. 2014;28:588–95.
Zhao Q-S, Xia N, Zhao N, Li M, Bi C-L, Zhu Q, Qiao G-F, Cheng Z-F. Localization of human mesenchymal stem cells from umbilical cord blood and their role in repair of diabetic foot ulcers in rats. Int J Biol Sci. 2014;10:80.
Menasché P. Stem cells for clinical use in cardiovascular medicine. Thromb Haemost. 2005;94:697–701.
Zhang M, Methot D, Poppa V, Fujio Y, Walsh K, Murry CE. Cardiomyocyte grafting for cardiac repair: graft cell death and anti-death strategies. J Mol Cell Cardiol. 2001;33:907–21.
Moon KM, Park YH, Lee JS, Chae YB, Kim MM, Kim DS, Kim BW, Nam SW, Lee JH. The effect of secretory factors of adipose-derived stem cells on human keratinocytes. Int J Mol Sci. 2012;13:1239–57.
Safari S, Eidi A, Mehrabani M, Fatemi MJ, Sharifi AM. Conditioned medium of adipose-derived mesenchymal stem cells as a Promising candidate to protect high Glucose-Induced Injury in cultured C28I2 chondrocytes. Adv Pharm Bull. 2022;12:632.
Zhang C, Wang T, Zhang L, Chen P, Tang S, Chen A, Li M, Peng G, Gao H, Weng H. Combination of lyophilized adipose-derived stem cell concentrated conditioned medium and polysaccharide hydrogel in the inhibition of hypertrophic scarring. Stem Cell Res Ther. 2021;12:1–13.
Kim Y-J, Lee SH, Im J, Song J, Kim HY, Bhang SH. Increasing angiogenic efficacy of conditioned medium using light stimulation of human adipose-derived stem cells. Commun Biology. 2022;5:1–11.
Kouhkheil R, Fridoni M, Abdollhifar M-A, Amini A, Bayat S, Ghoreishi SK, Chien S, Kazemi M, Bayat M. Impact of photobiomodulation and condition medium on mast cell counts, degranulation, and wound strength in infected skin wound healing of diabetic rats, Photobiomodulation, photomedicine, and laser surgery, 37 (2019) 706–14.
Fridoni M, Kouhkheil R, Abdollhifar MA, Amini A, Ghatrehsamani M, Ghoreishi SK, Chien S, Bayat S, Bayat M. Improvement in infected wound healing in type 1 diabetic rat by the synergistic effect of photobiomodulation therapy and conditioned medium. J Cell Biochem. 2019;120:9906–16.
Si Z, Wang X, Sun C, Kang Y, Xu J, Wang X, Hui Y. Adipose-derived stem cells: sources, potency, and implications for regenerative therapies. Biomed Pharmacother. 2019;114:108765.
Hamblin MR. Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophys. 2017;4:337–61.
Bhang SH, Lee S, Shin J-Y, Lee T-J, Jang H-K, Kim B-S. Efficacious and clinically relevant conditioned medium of human adipose-derived stem cells for therapeutic angiogenesis. Mol Ther. 2014;22:862–72.
Funding
This study primarily received financial support from NIH grants R44DK133065 and R44DK105692.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical considerations
The protocols, methods, and tests employed in this study were approved by the Ethics Committee at the School of Medicine of Shahid Beheshti University of Medical Sciences (SBMU.MSP.REC.1400.456).
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Asadi, R., Mostafavinia, A., Amini, A. et al. Acceleration of a delayed healing wound repair model in diabetic rats by additive impacts of photobiomodulation plus conditioned medium of adipose-derived stem cells. J Diabetes Metab Disord 22, 1551–1560 (2023). https://doi.org/10.1007/s40200-023-01285-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-023-01285-3