Abstract
Purpose of Review
This systematic review aims to evaluate physical performance outcome tools that are used most frequently to assess rehabilitation interventions. The scope of this paper focused on outcomes used with established lower limb amputees when assessing interventions such as exercise programs or changes in prescription published in the last 5 years.
Recent Findings
The most recorded outcome measures used across all the papers were timed walk tests and the Activity Balance Confidence Scale. Many outcomes did not produce statistically significant results with established amputee cohorts. Understanding the minimal important clinical difference is key.
Summary
The use of outcome measures is essential. Training and education are likely to increase the use of outcome measures. Quality of life measures are important in conjunction with physical outcomes. Simple timed walk tests are commonly used. These are in general easy to administer requiring a small space, limited equipment, and a short time frame.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lower limb amputation is a life changing event. Approximately 185,000 amputations of the lower and upper limb are carried out each year in the USA [1]. The number of people living with an amputation is expected to increase given that life expectancy is increasing as is the rate of diabetes mellitus [2]. The level at which a limb is amputated impacts the potential for successful prosthetic rehabilitation. The Scottish Physiotherapy Amputee Rehabilitation Group (SPARG) found that of those undergoing an amputation only 66.9% at the transtibial level and 20.9% at the transfemoral level advance to prosthetic limb usage [3]. The use of a prosthesis is physically [4,5,6] and cognitively demanding [7], requiring a period of rehabilitation [8] and gait training to become a proficient prosthetic user.
Early rehabilitation following amputation varies depending on an individuals’ general health, physical fitness, and other comorbidities [9]. Rehabilitation aims to return the prosthetic user to their pre-amputation activity level, where this is physically possible. Finding valid and reliable ways to communicate this activity level both intradisciplinary and interdisciplinary has become increasingly important for practitioners. While the more simplistic options such as the Special Interest Group in Amputee Medicine (SIGAM) mobility grades provide a number of categories, this is not always representative of the individuals function and capabilities beyond basic locomotion [10]. Tools such as the Amputee Mobility Predictor (AMP) [11] can be used both with and without a prosthesis to try to quantify activity level. For the more active prosthetic user, the Comprehensive High Level Amputee Mobility Predictor (CHAMP) can be used [12]. Following amputation, rehabilitation can take many forms, and may be appropriate at a variety of intervals. In the early stages, post-surgery general conditioning and early weight bearing are key. However, as confidence and mobility increase, more advanced components may be appropriate. Additional gait training to improve gait symmetry or cosmesis, or additional therapy if there is a prescription change, or a change in health status may be required. The ability to quantify any change helps to support the ongoing use of interventions and provides evidence of improved outcomes [13].
The use of outcome measures (OMs) is becoming more prevalent in the field of prosthetics and orthotics with at least 43 different measuring tools being used [14]. Clinicians administer self-report measures and ask prosthetic users to record trips and falls, pain levels, and complete other validated outcomes such as the Prosthesis Evaluation Questionnaire (PEQ) [15]. With the use of smart watch activity monitors and “in device” step counters, such as that of the Ottobock C-Leg (Ottobock Healthcare, Duderstadt, Germany), remote activity monitoring is becoming increasingly possible. This may be useful for prosthetic users who are comfortable with technology but less applicable to the elderly, lower activity individual. Outcome measures are used to assess quality of life [16], depression [17], mobility prediction [11], and physical activity levels [18]. While some of these outcome measures are self-reported, others are measured within a clinical or community setting. Some clinicians report that outcome measures are not of benefit in clinical practice and do not use them regularly [19]. Many studies use quality of life (QoL) outcomes to demonstrate the importance of appropriate prosthetic prescription and the psychological benefits [20]; they may provide information beyond demonstrating an improvement in walking. Many QoL outcomes take the form of questionnaires. Physical outcome measures play an important role in assessing the functional outcome of a prosthetic intervention. The use of performance-based measures such as the 6-min walk test [21] has been proven to provide good reliability in a lower limb amputee population [22]. One of the main challenges is determining the difference between a statistically significant outcome and a clinically significant change. For some outcome measures, the minimum detectable change gives an indication of the improvement required to be classed as a higher activity level [18, 23••]. While steps are being taken to establish this, there are also the challenges of the reported practice effects in performance-based tests [24].
Recent reviews have focused on the use of outcomes in clinical practice, the barriers to their use [25•], physical activity measurement [26], and activity following lower limb amputation in free-living conditions rather than within a clinical or laboratory setting [27]. This review aims to assess the current use of physical performance outcomes in rehabilitation with established lower limb amputees through a systematic review of the literature.
Methodology
A systematic literature review was completed in September 2022 in the following databases: Cochrane Library, Embase, PubMed, and Science Direct. Relevant keywords (and combinations) were selected including “physical activity” and “outcome measure” or “tool” and “lower limb prosthesis” or “lower limb amputee”. Included articles had to have been published after January 1, 2017, be available in English, be peer reviewed, accessible in full text, and the studies to have been completed on humans. All included articles had to have a focus on physical rehabilitation outcomes and have a baseline or control to compare with the intervention. Articles were excluded if they were published outside of this time frame, focused on outcome measure validation, phantom limb pain, spinal cord injuries, trial products, or computational models.
The two authors ran the searches independently and applied the agreed inclusion and exclusion criteria. The Cohen’s Kappa level of rater agreement was calculated as 0.7978 showing a substantial agreement between raters. A third reviewer was not required for any articles as agreement was achieved between the two authors. The initial search returned 1177 results, and after review of title and abstract, this was reduced to 32. Once articles had been read in full and exclusion and inclusion criteria were applied, this left 15 articles included in the final review. Articles were assessed against the Credibility, Accuracy, Reasonableness, Support (CARS) checklist [28] to evaluate each information source. No further articles were removed on the basis of quality or credibility.
Results
A total of 15 articles were included in the final review. Eight of these used physical performance measures to assess the impact of a change in component prescription as part of ongoing rehabilitation. The remaining seven used physical outcomes measures to assess the suitability of rehabilitation interventions for established amputees.
Across the papers, the outcomes measured were not generally limited to only physical outcome tools. Researchers used a combination of self-reported and measured outcomes often in combination with other quality of life (QoL) measures. QoL was assessed using many outcomes including the Short Form 36- QoL [29] and the Prosthesis Evaluation Questionnaire [15]. The physical outcomes measured used across the included studies are presented in Table 1.
Several of the papers used physical performance outcomes as an assessment tool for comparing different prosthetic limb components. Çalışkan Uçkun et al. [30] used physical outcomes to compare pin locking vs vacuum socket suspension systems. Davie-Smith et al. [31], Jayaraman et al. [32], and Knight et al. [33] used physical outcome measures when comparing prosthetic knee prescriptions, specifically microprocessor (MPK) vs non-microprocessor (NMPK) or powered knees. Morgan et al. [34], Kim et al. [35], and Kaufman and Bernhardt [36] compared different designs of foot and ankle components, and Barnett et al. [37] compared MPK vs NMPK in combination with rigid and hydraulic ankles. Five of the studies used timed walk tests, two studies looked at the L-test, and two used the AMP.
Timed walk tests measure speed and distance and are a commonly used and easily administered outcome measure. The test only requires a stopwatch and a straight walking area of known length. The 2-min walk test (2MWT) is a reliable measure for use with unilateral lower limb amputees showing good interrater and intrarater reliability [38]. Similar results have been found with the 6-min walk test (6MWT) [22]. The outcomes of the 2MWT and the 6MWT have been shown to be comparable. The 2WMT was used in two studies [31, 37] and the 6MWT in three studies [32,33,34]. In the study by Davie- Smith et al. [31], the 2MWT was used to assess lower activity level, unilateral, transfemoral amputees comparing outcomes with a NMPK and an MPK 6 months post-delivery. A statistical improvement was found (p < 0.001) with an average improvement of 8 m when using the MPK. Barnett et al. [37] also found a statistically significant result from this test (p = 0.001) when comparing the combinations of NMPK, MPK, rigid ankle, and hydraulic ankle. The optimal prescription was found to be the MPK with a hydraulic ankle. Jayaraman et al. [32] also compared NMPK and MPK prescriptions in a group of dysvascular amputees. The 6MWT showed no statistically significant improvement between groups. Similarly, Knight et al. [33] found that veterans walked a shorter distance with the powered knee than the standard microprocessor knee. No significant improvement (p = 0.29) was found, in the distance walked, by Morgan et al. [34] in the 6MWT when comparing a standard energy storing foot and a cross-over style foot.
The L-test is an advancement of the timed up and go (TUG) test [39, 40]. It is easy to administer with the patient being asked to rise from a chair, walk 5 m, turn left and walk 5 m, turn right and walk 5 m, and walk a further 5 m to return to the chair. Given the additional complexity, when compared to the standard TUG, it is more appropriate for higher activity prosthetic users. When assessing performance 6 months post-delivery of a MPK, Davie-Smith et al. [31] found a significant improvement (p = 0.001) manifested by an average reduction in the time to perform the L-test by 5 s. When comparing combinations of knees and feet, Barnett et al. [37] found that the MPK with hydraulic ankle was on the threshold of significance (p = 0.05).
One of the other outcomes commonly selected by researchers was the Amputee Mobility Predictor (AMP) [11]. There are versions of the AMP available for assessment with and without a prosthesis. The AMP assesses prosthetic use across a number of tasks, and a higher score indicates a greater level of function. The AMP was used to determine current mobility, and only users who scored between 37 and 40 were selected for inclusion in the MPK assessment [31]; these would be deemed high K2 or low K3 on the Medicare activity classification scale. The participants achieved better outcomes when provided with an MPK. When comparing outcomes after randomized prescription of an NMPK and an MPK, Jayaraman et al. [32] found a statistically significant improvement (p = 0.008) following MPK prescription.
In the qualifying studies, balance was assessed using a number of outcomes, including the Activity Balance Confidence Scale (ABC) [41], Berg Balance Score (BBS) [42], and Four Square Step Test (FSST) [43]. Davie-Smith et al. [31] found a 61.9–77% improvement (p < 0.001) in ABC scores when participants were provided an MPK. Jayaraman et al. [32] looked at results in the BBS and FSST when comparing C-leg with NMPK. No significant differences were found between groups in either outcome.
The 7 other papers included in this review consider physical outcome measures to review the effectiveness of focused exercise programs. Many of these provide remote instruction and monitoring to the participants. Gaunaurd et al. [44] used mobile device outcome-based rehabilitation with the aim to improve mobility, and gait. Similarly, Christiansen et al. [45] considered the impact of a telehealth program on physical activity behaviour. Tao et al. [46] focused on balance and exercise therapy to impact walking capacity through interactive adaptive games. The Wii Fit® games and WiiNWalk-fit balance board is an exergaming platform where participants are able to complete games to enhance balance and exercise therapy. The Big Brain Academy: Wii Degree (Nintendo, Kyoto, Japan) was used as a control where participants complete activities focused on cognitive function. The WiiNWalk intervention did not improve balance or walking capacity. Godlwana, Stewart, and Musenge [47•] compared the effect of a home-based exercise programme with the standard outpatient follow up and used physical outcome measures to consider the effectiveness. Participants who completed the home exercise program had improved results. Wong and Gibbs [48] used physical outcome measures to study the impact of a “committed wellness-walking program.” Miller et al. [49] explored the effects of a supervised community-based exercise program on balance, confidence and gait. In a case study by Rosenblatt et al. [50], physical outcome measures were used to demonstrate the effect of non-limb wearing over a period of 4 weeks and limited use over a further 12 weeks. Four of these studies used the ABC, Activities-Specific Balance Confidence Scale; three studies made use of the 2MWT, and a further three made use of the Timed Up and Go (TUG).
The Activities-Specific Balance Confidence (ABC) Scale [41] is a self-reported outcome measure of balance confidence assessing vestibular, non-vestibular, and functional mobility. Participants rate balance confidence in performing 16 specific activities, with zero representing no confidence and 100 representing completed confidence in carrying out the task. In a population of older adults, Myers et al. [51] reported that results lower than 50% on the ABC scale are considered a low level of functioning and over 80% a high level of physical functioning. When analysed for relative reliability and internal consistency, they found “excellent relative reliability” within the population of people with lower extremity amputations [52].
The ABC was used in four of the papers reviewing exercise interventions [46, 48, 50, 53]. Tao et al. [46] reported a statistically significant group effect with the mean and (standard deviation) ABC improving from 83.3 (10.8) at baseline to 84.6 (12.4) at 12-month follow-up. This was using the WiiNWalk compared to the control group, using Big Brain Academy, who’s baseline was 82.7 (15.7) and reduced to 77.1 (18.2) at 12-month follow-up. The focus on balance and physical activity over cognitive training provided a positive improvement in balance. An increase from 2.4 to 2.8 in balance confidence was found by Wong and Gibbs [48] on the 4-point ABC scale (p = 0.074) when participants were noted to be committed to the wellness walking program (n = 30 participants). Participants were classified as committed when attending more than 3 sessions over the 3-year time period of the study. Miller et al. [53] demonstrated an increase in group mean score for ABC from 63.4 to 73.7% when taking part in a supervised community-based exercise program. Transtibial participants, as a group, improved by 14.3% and transfemoral participants by 18.7%. When considering the total group, 37.5% of the participants increased their mean score by more than 10%. Two participants had a reduction in mean score of 5%. Rosenblatt, Stachowiak, and Reddin [50] discuss the effects of non-limb wearing over short periods of time in a case study. Although objective balance measures were relatively unaffected, the self-reported ABC dropped from 79.4 at baseline to 60.9 at follow-up.
The 2-min walk test, as noted previously, is a reliable outcome measure for use with lower limb amputees. It was used in three of the papers [45, 46, 48]. The WiiNWalk group showed an improvement over the control. At baseline, the mean distance walked recorded as 125.6 m (42.6 standard deviation) and 130.8 m (39.8) at 12-month follow-up. The control group using Big Brain Academy demonstrated a reduction in walking distance from 126.5 m (30.4) at baseline and 125.5 m (30.8) at 12-month follow-up [46]. The wellness walking program reported by Wong and Gibbs [48] found that for one time, only participants (n = 220) walking speed was reported as 0.74 m/s ± 0.39 whereas for committed participants (n = 29) was reported as 0.88 m/s ± 0.27. The 2MWT was unable to prove a statistically significant change to average walking speed for participants of the wellness walking programme. Christiansen et al. [45] reviewed the effect of twelve, completed weekly, 20-min telehealth sessions of physical behaviour interventions. Baseline measures were carried out for both groups; Group 1 participated in the intervention during weeks 1–12 with no further intervention for the following 12 weeks. Group 2 had attention control during weeks 1–12 during which a therapist delivered a short health and safety talk related to age followed by a brief period of light range of motion tasks for both upper and lower extremities. This was followed by the 12-week intervention. Group 1 baseline was recorded as 97.7 m compared to 85.5 m at 12 weeks and 103.4 m at 24 weeks. Group 2 with the additional attention control input demonstrated a baseline of 101.8 m, 101.3 m at 12 weeks, and 103.3 m at 24 weeks.
The Timed Up and Go (TUG) was included in three papers [44, 45, 47•] and is applicable to participants with lower extremity amputations and has demonstrated validity in assessing functional mobility [40]. It has demonstrated high interreliability and intrareliability when used to examine elderly adults including amputees [54]. The Timed Up and Go measures functional mobility through a performance-based task which includes rising from a chair, walking 3 m at a comfortable pace, turning at the 3 m mark and returning to sitting in the chair. Participants who take longer than 30 s to complete the task have been shown to require more assistance, whereas if the test is completed in less than 20 s, the participant is likely to be independently mobile. Gaunaurd et al. [44] used a Mobile Device Outcomes-Based Rehabilitation Program (MDORP) to improve participants strength, mobility, and gait quality. To assess the outcomes of this, the researchers examined two course variants of the Timed Up and Go with the turn at 3 m both towards and away from the prosthetic side. Turning towards the prosthesis produced a baseline of 9.4 s (± 1.4 s) (range 5.9–11.2 s). Following intervention this reduced to 8.8 s ± 1.4 s (range 7.0–12.1). Turning away from the prosthesis at baseline was 9.6 s ± 1.6 s (range 7.0–12.6 s), and at 8 weeks post intervention, this reduced to 8.7 s ± 1.1 s (range 7.1–10.7 s). Neither of these showed a statistically significant difference. Christiansen et al. [45] reviewed TUG results in two groups following the use of the telehealth intervention, as previously described. The baseline of Group 1 was recorded as 19.4 s, at 12 weeks 18.0 s, and at 24 weeks 15.3 s. The Group 2 baseline was 14.9 s, at 12 weeks 14.8 s, and at 24 weeks 14.5 s. The authors noted that the intervention carried out with group 1 between weeks 1 and 12 did improve their time; however, the biggest improvement occurred between weeks 12 and 24 where there was no intervention. Group 2 remained consistent in their timings with the attention control during weeks 1 and 12 and intervention between weeks 12 and 24. No statistical analysis of the results was reported. Godlwana, Stewart, and Musenge [47•] did not report baseline measures for their control or intervention groups; however, there is a comparison of TUG results between post intervention at 3 months and then at 6 months. Both groups received the normal standard care; however, the intervention group received a home education and exercise programme alongside the standard care for 3 months. The control group at 3 months was reported as 45.078 s ± 41.516 s and at 6 months 36.077 s ± 36.186 s. Compared with the intervention group at 3 months 35.392 s ± 32.484 s and at 6 months 28.224 s ± 20.963 s, the intervention group at both 3 and 6 months is quicker than the control group; however, this was not statistically significant.
Discussion
In the reviewed papers, over thirty different outcome measures were used. Two-thirds of these related to physical performance outcome measures. The use of outcome measures has not routinely been integrated into clinical care for lower extremity amputees. Many prosthetic and orthotic clinicians report barriers such as lack of time, lack of understanding, or perceived clinical value [19]. Gaunaurd et al. [55] and Young, Rowley, and Lalor [56] reported “38% of prosthetic practitioners in the United States and 28.4% of prosthetics and orthotics (P&O) practitioners in the United Kingdom use OM’s routinely.” These low numbers exist despite the fact that there is clear evidence for the use of outcome measures in improving patient satisfaction, ensuring patient-centred decisions, recording patient progress, and ensuring evidence-based practice. Rapaport et al. [57••] provided an education program to prosthetic and orthotic practitioners and demonstrated an increase in confidence in the use of these measures and their monthly use doubled after this. Despite this, selecting an appropriate measure can be challenging.
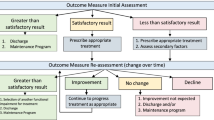
While the use of OMs is considered to be important, it is also vital to recognize and understand the results of these. For primary amputees or those early in rehabilitation, there will be less consideration for the ceiling effect exhibited. Some authors have noted that established amputees may have achieved their optimal gait speed and physical outcome measures would be less appropriate than QoL measures [20]. Objective, quantifiable results are only meaningful if there is evidence of a minimal clinically important difference (MCID) for the outcome measure you are working with. MCID is “…defined as the smallest change in an outcome that a patient would perceive as clinically meaningful” [58] equating to a change in quantifiable results that is large enough to make a difference to patient prescription or care. In the papers reviewed often, the selected outcomes produced a statistically significant result but this was not classed as a MCID [31]. The TUG test has been shown to have a ceiling effect for more active amputees and is likely not suitable for established walkers who are of moderate activity or above [39].
While physical outcome measures provide an important insight into amputee physical functioning, they do not provide a complete metric of rehabilitation success. Quality of life, social adaptation, and mental health are all relevant factors to consider. Multiple outcome measures have subscales specific to these elements. These should be administered in conjunction with physical performance outcomes to give a more rounded picture of achievement. Balance and falls incidence were considered by a number of researchers: these factors also relate to device user confidence [31, 44, 46]. MPKs have been well documented to reduce falls incidence and as such are an important outcome when reviewing these components [59, 60]. In many of the papers, physical performance was not greatly impacted by the rehabilitation intervention but patients still reported personal improvement.
While this research was completed by two authors, a select number of databases were used so some literature may have been omitted.
Conclusion
Across the included papers, over 30 different outcome measures were included. One of the challenges for researchers is identifying the correct outcome measure to use. The measure should, ideally, be validated for use with the desired cohort, be sensitive enough to measure the required outcome, and be reliable. Practitioners should be provided with continuous professional development opportunities, including training sessions and the opportunity for hands on practice to establish outcomes measures in daily use as a standard of care.
From the literature published in the past 5 years, the most used physical outcome assessment tools used to assess rehabilitation intervention are timed walk tests and the Activity Balance Confidence Scale. All of these have been validated for use with lower limb amputees and as such represent a good methodological approach to research in the field.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Owings M, Kozak LJ. Ambulatory and inpatient procedures in the United States, 1996. vol 139. US Department of Health and Human Services, Centers for Disease Control and …; 1998.
Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the Prevalence of Limb Loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89(3):422–9. https://doi.org/10.1016/j.apmr.2007.11.005.
Davie-Smith FH, J. Scott, H. A survey of the lower limb amputee population in Scotland 2016. BACPAR2019. p. 56.
Göktepe AS, Cakir B, Yilmaz B, Yazicioglu K. Energy expenditure of walking with prostheses: comparison of three amputation levels. Prosthet Orthot Int. 2010;34(1):31–6. https://doi.org/10.3109/03093640903433928.
Miller MJ, Jones J, Anderson CB, Christiansen CL. Factors influencing participation in physical activity after dysvascular amputation: a qualitative meta-synthesis. Disabil Rehabil. 2019;41(26):3141–50. https://doi.org/10.1080/09638288.2018.1492031.
Miller MJ, Cook PF, Kline PW, Anderson CB, Stevens-Lapsley JE, Christiansen CL. Physical function and pre-amputation characteristics explain daily step count after dysvascular amputation. Pm r. 2019;11(10):1050–8. https://doi.org/10.1002/pmrj.12121.
Moller S, Rusaw D, Hagberg K, Ramstrand N. Reduced cortical brain activity with the use of microprocessor-controlled prosthetic knees during walking. Prosthet Orthot Int. 2019;43(3):257–65.
Christiansen CL, Fields T, Lev G, Stephenson RO, Stevens-Lapsley JE. Functional outcomes after the prosthetic training phase of rehabilitation after dysvascular lower extremity amputation. PM&R. 2015;7(11):1118–26. https://doi.org/10.1016/j.pmrj.2015.05.006.
Darter BJ, Hawley CE, Armstrong AJ, Avellone L, Wehman P. Factors influencing functional outcomes and return-to-work after amputation: a review of the literature. J Occup Rehabil. 2018;28(4):656–65. https://doi.org/10.1007/s10926-018-9757-y.
Ryall NH, Eyres SB, Neumann VC, Bhakta BB, Tennant A. The SIGAM mobility grades: a new population-specific measure for lower limb amputees. Disabil Rehabil. 2003;25(15):833–44. https://doi.org/10.1080/0963828021000056460.
Gailey RS, Roach KE, Applegate EB, Cho B, Cunniffe B, Licht S, et al. The Amputee Mobility Predictor: An instrument to assess determinants of the lower-limb amputee’s ability to ambulate. Arch Phys Med Rehabil. 2002;83(5):613–27. https://doi.org/10.1053/apmr.2002.32309.
Gailey RS, Gaunaurd IA, Raya MA, Roach KE, Linberg AA, Campbell SM, et al. Development and reliability testing of the Comprehensive High-Level Activity Mobility Predictor (CHAMP) in male servicemembers with traumatic lower-limb loss. J Rehabil Res Dev. 2013;50(7):905–18. https://doi.org/10.1682/jrrd.2012.05.0099.
Resnik L, Borgia M. Reliability of outcome measures for people with lower limb amputation: distinguishing true change from statistical error. Phys Ther. 2011;91(4):1–11.
Heinemann AW, Connelly L, Ehrlich-Jones L, Fatone S. Outcome instruments for prosthetics: clinical applications. Phys Med Rehabil Clin N Am. 2014;25(1):179–98. https://doi.org/10.1016/j.pmr.2013.09.002.
Legro MW, Reiber GD, Smith DG, del Aguila M, Larsen J, Boone D. Prosthesis evaluation questionnaire for persons with lower limb amputations: assessing prosthesis-related quality of life. Arch Phys Med Rehabil. 1998;79(8):931–8.
World Health O. The World Health Organization quality of life (WHOQOL) - BREF. 2012 revision ed. Geneva: World Health Organization; 2004.
Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatr Ann. 2002;9(32):509–15.
Ries JD, Echternach JL, Nof L, Gagnon BM. Test-retest reliability and minimal detectable change scores for the timed “Up & Go” test, the six-minute walk test, and gait speed in people with Alzheimer disease. Phys Ther. 2009;89(6):569–79. https://doi.org/10.2522/ptj.20080258.
Hafner BJ, Spaulding SE, Salem R, Morgan SJ, Gaunaurd I, Gailey R. Prosthetists’ perceptions and use of outcome measures in clinical practice: long-term effects of focused continuing education. Prosthet Orthot Int. 2017;41(3):266–73.
Dunlop F, Aranceta-Garza A, Munjal R, McGarry A, Murray L. A retrospective review of psychosocial outcomes after microprocessor knee prescription. JPO: Journal of Prosthetics and Orthotics. 2022.
Butland RJ, Pang J, Gross ER, Woodcock AA, Geddes DM. Two-, six-, and 12-minute walking tests in respiratory disease. Br Med J (Clin Res Ed). 1982;284(6329):1607–8. https://doi.org/10.1136/bmj.284.6329.1607.
Lin S-J, Bose NH. Six-minute walk test in persons with transtibial amputation. Arch Phys Med Rehabil. 2008;89(12):2354–9. https://doi.org/10.1016/j.apmr.2008.05.021.
•• Carse B, Scott H, Davie-Smith F, Brady L, Colvin J. Minimal clinically important difference in walking velocity, gait profile score and two minute walk test for individuals with lower limb amputation. Gait Posture. 2021;88:221–4. https://doi.org/10.1016/j.gaitpost.2021.06.001. (This retrospective review provides important minimal clinically important differences for walking velocity, gait profile score, and the 2-min walk test)
Sawers A, Hafner BJ. Characterizing practice effects in performance-based tests administered to users of unilateral lower limb prostheses: a preliminary study. Pm r. 2021;13(9):969–78. https://doi.org/10.1002/pmrj.12513.
• Ostler C, Scott H, Sedki I, Kheng S, Donovan-Hall M, Dickinson A, et al. From outcome measurement to improving health outcomes after lower limb amputation—a narrative review exploring outcome measurement from a clinical practice perspective. Prosthet Orthot Int. 2022;46(4):e341–50. https://doi.org/10.1097/pxr.0000000000000100. (This literature review explores the barriers to outcome measure use and the appropriateness of these)
Jamieson.A.G ML, Buis.A. The use of physical activity outcomes in rehabilitation interventions for lower limb amputees: a systematic review. . Canadian Prosthetics & Orthotics Journal. 2020;3(1, No. 2). https://doi.org/10.33137/cpoj.v3i1.33931.
Jamieson A, Murray L, Stankovic L, Stankovic V, Buis A. Human activity recognition of individuals with lower limb amputation in free-living conditions: a pilot study. Sensors. 2021;21(24):8377.
Harris R: The C.A.R.S Checklst. . http://www.virtualsalt.com/evalu8it.htm (2013). Accessed 01/09/2022 2022.
Son S, Pyun SB, Kim SD. Assessment of quality of life in lower limb amputees using Short-Form 36. J Korean Acad Rehabil Med. 2001;25(3):505–13.
Çalışkan Uçkun A, Yurdakul FG, Almaz ŞE, Yavuz K, Koçak Ulucaköy R, Sivas F, et al. Reported physical activity and quality of life in people with lower limb amputation using two types of prosthetic suspension systems. Prosthet Orthot Int. 2019;43(5):519–27. https://doi.org/10.1177/0309364619869783.
Davie-Smith F, Carse B. Comparison of patient-reported and functional outcomes following transition from mechanical to microprocessor knee in the low-activity user with a unilateral transfemoral amputation. Prosthet Orthot Int. 2021;45(3):198–204. https://doi.org/10.1097/pxr.0000000000000017.
Jayaraman C, Mummidisetty CK, Albert MV, Lipschutz R, Hoppe-Ludwig S, Mathur G, et al. Using a microprocessor knee (C-Leg) with appropriate foot transitioned individuals with dysvascular transfemoral amputations to higher performance levels: a longitudinal randomized clinical trial. J Neuroeng Rehabil. 2021;18(1):88. https://doi.org/10.1186/s12984-021-00879-3.
Knight AD, Jayaraman C, Elrod JM, Schnall BL, McGuire MS, Sleeman TJ, et al. Functional performance outcomes of a powered knee-ankle prosthesis in service members with unilateral transfemoral limb loss. Mil Med. 2022. https://doi.org/10.1093/milmed/usac231.
Morgan SJ, McDonald CL, Halsne EG, Cheever SM, Salem R, Kramer PA, et al. Laboratory- and community-based health outcomes in people with transtibial amputation using crossover and energy-storing prosthetic feet: a randomized crossover trial. PLoS One. 2018;13(2):e0189652. https://doi.org/10.1371/journal.pone.0189652.
Kim J, Gardinier ES, Vempala V, Gates DH. The effect of powered ankle prostheses on muscle activity during walking. J Biomech. 2021;124:110573. https://doi.org/10.1016/j.jbiomech.2021.110573.
Kaufman KR, Bernhardt K. Functional performance differences between carbon fiber and fiberglass prosthetic feet. Prosthet Orthot Int. 2021;45(3):205–13. https://doi.org/10.1097/pxr.0000000000000004.
Barnett CT, Hughes LD, Sullivan AE, Strutzenberger G, Levick JL, Bisele M, et al. Exploring the interaction of knee and ankle component use on mobility test performance in people with unilateral transfemoral amputation. Prosthet Orthot Int. 2021;45(6):470–6. https://doi.org/10.1097/pxr.0000000000000042.
Brooks D, Hunter JP, Parsons J, Livsey E, Quirt J, Devlin M. Reliability of the two-minute walk test in individuals with transtibial amputation. Arch Phys Med Rehabil. 2002;83(11):1562–5. https://doi.org/10.1053/apmr.2002.34600.
Deathe AB, Miller WC. The L test of functional mobility: measurement properties of a modified version of the timed “up & go” test designed for people with lower-limb amputations. Phys Ther. 2005;85(7):626–35.
Schoppen T, Boonstra A, Groothoff JW, de Vries J, Goeken LN, Eisma WH. The Timed “up and go” test: reliability and validity in persons with unilateral lower limb amputation. Arch Phys Med Rehabil. 1999;80(7):825–8.
Miller WC, Deathe AB, Speechley M. Psychometric properties of the Activities-specific Balance Confidence scale among individuals with a lower-limb amputation11No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the author(s) or upon any organization with which the author(s) is/are associated. Arch Phys Med Rehabil. 2003;84(5):656–61. https://doi.org/10.1016/S0003-9993(02)04807-4.
Berg K. Measuring balance in the elderly: development and validation of an instrument. 1992.
Dite W, Temple VA. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil. 2002;83(11):1566–71.
Gaunaurd I, Gailey R, Springer B, Symsack A, Clemens S, Lucarevic J, et al. The effectiveness of the DoD/VA mobile device outcomes-based rehabilitation program for high functioning service members and veterans with lower limb amputation. Mil Med. 2020;185(Suppl 1):480–9. https://doi.org/10.1093/milmed/usz201.
Christiansen CL, Miller MJ, Kline PW, Fields TT, Sullivan WJ, Blatchford PJ, et al. Biobehavioral intervention targeting physical activity behavior change for older veterans after nontraumatic amputation: a randomized controlled trial. PM R. 2020;12(10):957–66. https://doi.org/10.1002/pmrj.12374.
Tao G, Miller WC, Eng JJ, Esfandiari E, Imam B, Lindstrom H, et al. Group-based telerehabilitation intervention using Wii Fit to improve walking in older adults with lower limb amputation (WiiNWalk): a randomized control trial. Clin Rehabil. 2022;36(3):331–41. https://doi.org/10.1177/02692155211061222.
• Godlwana L, Stewart A, Musenge E. The effect of a home exercise intervention on persons with lower limb amputations: a randomized controlled trial. Clin Rehabil. 2020;34(1):99–110. https://doi.org/10.1177/0269215519880295. (This randomised control trial provides good evidence of improvement following a home exercise intervention)
Wong CK, Gibbs WB. Factors associated with committed participation in a wellness-walking program for people with lower limb loss: a prospective cohort study. Prosthet Orthot Int. 2019;43(2):180–7. https://doi.org/10.1177/0309364618792943.
Miller MJ, Stevens-Lapsley J, Fields TT, Coons D, Bray-Hall S, Sullivan W, et al. Physical activity behavior change for older veterans after dysvascular amputation. Contemp Clin Trials. 2017;55:10–5. https://doi.org/10.1016/j.cct.2017.01.008.
Rosenblatt NJ, Stachowiak A, Reddin C. Prosthetic disuse leads to lower balance confidence in a long-term user of a transtibial prosthesis. Adv Wound Care. 2021;10(9):529–33. https://doi.org/10.1089/wound.2019.1086.
Myers AM, Fletcher PC, Myers AH, Sherk W. Discriminative and evaluative properties of the Activities-specific Balance Confidence (ABC) Scale. The Journals of Gerontology: Series A. 1998;53A(4):M287–94. https://doi.org/10.1093/gerona/53A.4.M287.
Fuller K, Omaña Moreno HA, Frengopoulos C, Payne MW, Viana R, Hunter SW. Reliability, validity, and agreement of the short-form Activities-specific Balance Confidence Scale in people with lower extremity amputations. Prosthet Orthot Int. 2019;43(6):609–17. https://doi.org/10.1177/0309364619875623.
Miller CA, Williams JE, Durham KL, Hom SC, Smith JL. The effect of a supervised community-based exercise program on balance, balance confidence, and gait in individuals with lower limb amputation. Prosthet Orthot Int. 2017;41(5):446–54.
Brooks D, Davis AM, Naglie G. Validity of 3 physical performance measures in inpatient geriatric rehabilitation. Arch Phys Med Rehabil. 2006;87(1):105–10. https://doi.org/10.1016/j.apmr.2005.08.109.
Gaunaurd I, Spaulding SE, Amtmann D, Salem R, Gailey R, Morgan SJ, et al. Use of and confidence in administering outcome measures among clinical prosthetists: results from a national survey and mixed-methods training program. Prosthet Orthot Int. 2015;39(4):314–21. https://doi.org/10.1177/0309364614532865.
Young J, Rowley L, Lalor S. Use of outcome measures among prosthetists and orthotists in the United Kingdom. JPO: Journal of Prosthetics and Orthotics. 2018;30(3):152–7.
•• Rapaport MS, Negri C, Pousett BM, Mathis S. Attitudes and behaviors toward using outcome measures in clinical practice: findings of a blended education program. Prosthet Orthot Int. 2022;46(5):477–83. https://doi.org/10.1097/pxr.0000000000000167. (This research provides clear evidence of the increase in use of outcome measures following additional training. Continuous professional development opportunities should be made available to prosthetic and orthotic clinicians)
Vetter TR, Chou R. 80 - Clinical trial design methodology for pain outcome studies. In: Benzon HT, Rathmell JP, Wu CL, Turk DC, Argoff CE, Hurley RW, editors. Practical management of pain. 5th ed. Philadelphia: Mosby; 2014. p. 1057- 65.e3.
Hafner BJ, Willingham LL, Buell NC, Allyn KJ, Smith DG. Evaluation of function, performance, and preference as transfemoral amputees transition from mechanical to microprocessor control of the prosthetic knee. Arch Phys Med Rehabil. 2007;88(2):207–17.
Berry D, Olson MD, Larntz K. Perceived stability, function, and satisfaction among transfemoral amputees using microprocessor and nonmicroprocessor controlled prosthetic knees: a multicenter survey. JPO: Journal of Prosthetics and Orthotics. 2009;21(1):32–42.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Murray, L., McGinty, G. Use of Physical Activity Measures in Rehabilitation Interventions Following Lower Extremity Amputation. Curr Phys Med Rehabil Rep 11, 25–34 (2023). https://doi.org/10.1007/s40141-023-00383-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-023-00383-w