Abstract
Purpose of Review
The main objective of the 1st part of this review is to demonstrate that a better understanding of comorbidities such as COPD, obstructive sleep apnea, thyroid dysfunction, cardiorenal syndrome, its pathophysiological and therapeutic implications, impact on the management of FH by interfering with its survival, and quality of life of patients.
Recent Findings
The prevalence of heart failure will increase 46% from 2012 to 2030, resulting in > 8 million people ≥ 18 years of age. This disease has a large burden of noncardiovascular comorbidities, which may increase the risk of mortality and decrease quality of life. There is a perception that patients hospitalized for HF are also becoming more medically complex. In this review, we highlight important comorbidities often found in patients with heart failure.
Summary
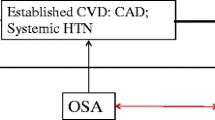
Approximately one-third of patients with heart failure also have chronic obstructive pulmonary disease. Obstructive sleep apnea syndrome is a highly prevalent disorder in HF patients, occurring in 46–80% of patients. It is known that changes in thyroid metabolism have been associated as an independent risk factor regarding the progression and development of heart failure (HF). Understanding cardiorenal syndrome facilitates the management of FH.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart Disease and Stroke Statistics-2019 Update: a report from the American Heart Association. Circulation. 2019;139(10):e56–e528. https://doi.org/10.1161/CIR.0000000000000659. The most up-to-date statistics related to heart disease, stroke, and the cardiovascular risk factors.
Luscher TF. Heart failure: focus on comorbidities, inflammation, and heart rate. Eur Heart J. 2015;36(11):635–7. https://doi.org/10.1093/eurheartj/ehv037.
Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–19. https://doi.org/10.1161/HHF.0b013e318291329a.
Mentz RJ, Kelly JP, von Lueder TG, Voors AA, Lam CS, Cowie MR, et al. Noncardiac comorbidities in heart failure with reduced versus preserved ejection fraction. J Am Coll Cardiol. 2014;64(21):2281–93. https://doi.org/10.1016/j.jacc.2014.08.036.
van Deursen VM, Urso R, Laroche C, Damman K, Dahlstrom U, Tavazzi L, et al. Co-morbidities in patients with heart failure: an analysis of the European heart failure pilot survey. Eur J Heart Fail. 2014;16(1):103–11. https://doi.org/10.1002/ejhf.30.
Mascarenhas J, Azevedo A, Bettencourt P. Coexisting chronic obstructive pulmonary disease and heart failure: implications for treatment, course and mortality. Curr Opin Pulm Med. 2010;16(2):106–11. https://doi.org/10.1097/MCP.0b013e328335dc90.
Chhabra SK, Gupta M. Coexistent chronic obstructive pulmonary disease-heart failure: mechanisms, diagnostic and therapeutic dilemmas. Indian J Chest Dis Allied Sci. 2010;52(4):225–38.
de Groote P, Isnard R, Clerson P, Jondeau G, Galinier M, Assyag P, et al. Improvement in the management of chronic heart failure since the publication of the updated guidelines of the European Society of Cardiology. The Impact-Reco Programme. Eur J Heart Fail. 2009;11(1):85–91. https://doi.org/10.1093/eurjhf/hfn005.
Schefold JC, Filippatos G, Hasenfuss G, Anker SD, Von Haehling S. Heart failure and kidney dysfunction: epidemiology, mechanisms and management. Nat Rev Nephrol. 2016;12:610–23. https://doi.org/10.1038/nrneph.2016.113.
• Rangaswami J, Bhalla V, Blair JEA, Chang TI, Costa S, Lentine KL, et al. Cardiorenal syndrome: classification, pathophysiology, diagnosis, and treatment strategies: a scientific statement from the American Heart Association. Circulation. 2019;139:E840–E78. https://doi.org/10.1161/CIR.0000000000000664. Describe the epidemiology and pathogenesis of cardiorenal syndrome in the context of the continuously evolving nature of its clinicopathological description over the past decade.
• Clase CM, Carrero J-J, Ellison DH, Grams ME, Hemmelgarn BR, Jardine MJ, et al. Potassium homeostasis and management of dyskalemia in kidney diseases: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2020;97:42–61. https://doi.org/10.1016/j.kint.2019.09.018. To identify key issues relevant to the optimal prevention, management, and treatment of arrhythmias and their complications in patients with kidney disease.
Matsushita K, Sang Y, Yang C, Ballew SH, Grams ME, Coresh J, et al. Dyskalemia, its patterns, and prognosis among patients with incident heart failure: a nationwide study of US veterans. PLoS One. 2019;14:1–12. https://doi.org/10.1371/journal.pone.0219899.
Linde C, Qin L, Bakhai A, Furuland H, Evans M, Ayoubkhani D, et al. Serum potassium and clinical outcomes in heart failure patients: results of risk calculations in 21 334 patients in the UK. ESC Heart Fail. 2019;6:280–90. https://doi.org/10.1002/ehf2.12402.
Bianchi S, Regolisti G. Pivotal clinical trials, meta-analyses and current guidelines in the treatment of hyperkalemia. Nephrol Dialysis Transplant. 2019;34:iii51–61. https://doi.org/10.1093/ndt/gfz213.
Li L, Harrison SD, Cope MJ, Park C, Lee L, Salaymeh F, et al. Mechanism of action and pharmacology of patiromer, a nonabsorbed cross-linked polymer that lowers serum potassium concentration in patients with hyperkalemia. J Cardiovasc Pharmacol Ther. 2016;21:456–65. https://doi.org/10.1177/1074248416629549.
Pitt B, Anker SD, Bushinsky DA, Kitzman DW, Zannad F, Huang IZ. Evaluation of the efficacy and safety of RLY5016, a polymeric potassium binder, in a double-blind, placebo-controlled study in patients with chronic heart failure (the PEARL-HF) trial. Eur Heart J. 2011;32:820–8. https://doi.org/10.1093/eurheartj/ehq502.
Bakris GL, Pitt B, Weir MR, Freeman MW, Mayo MR, Garza D, et al. Effect of patiromer on serum potassium level in patients with hyperkalemia and diabetic kidney disease the AMETHYST-DN randomized clinical trial. J Am Med Assoc. 2015;314:151–61. https://doi.org/10.1001/jama.2015.7446.
Weir MR, Bakris GL, Bushinsky DA, Mayo MR, Garza D, Stasiv Y, et al. Patiromer in patients with kidney disease and hyperkalemia receiving RAAS inhibitors. N Engl J Med. 2015;372:211–21. https://doi.org/10.1056/NEJMoa1410853.
NCT03888066 CgI. Patiromer for the management of hyperkalemia in subjects receiving RAASi medications for the treatment of heart failure (DIAMOND). 2020.
Kosiborod M, Rasmussen HS, Lavin P, Qunibi WY, Spinowitz B, Packham D, et al. Effect of sodium zirconium cyclosilicate on potassium lowering for 28 days among outpatients with hyperkalemia: the HARMONIZE randomized clinical trial. J Am Med Assoc. 2014;312:2223–33. https://doi.org/10.1001/jama.2014.15688.
Roger SD, Spinowitz BS, Lerma EV, Singh B, Packham DK, Al-Shurbaji A, et al. Efficacy and safety of sodium zirconium cyclosilicate for treatment of hyperkalemia: an 11-month open-label extension of HARMONIZE. Am J Nephrol. 2019;50:473–80. https://doi.org/10.1159/000504078.
Yumino DAI, Wang H, Floras JS, Newton GE, Mak S, Ruttanaumpawan P, et al. Prevalence and physiological predictors of sleep apnea in patients with heart failure and systolic dysfunction. 2009;15:279–85. https://doi.org/10.1016/j.cardfail.2008.11.015.
• Borrelli C, Gentile F, Sciarrone P, Mirizzi G, Vergaro G, Ghionzoli N, et al. Central and obstructive apneas in heart failure with reduced, mid-range and preserved ejection fraction. Front Cardiovas Med. 2019;6. https://doi.org/10.3389/fcvm.2019.00125. A comparison of apnea prevalence, predictors and clinical correlates in the whole HF spectrum.
Arzt M, Woehrle H, Oldenburg O, Graml A, Suling A, Erdmann E, et al. Prevalence and predictors of sleep-disordered breathing in patients with stable chronic heart failure: the SchlaHF registry. JACC: Heart Failure. 2016;4:116–25. https://doi.org/10.1016/j.jchf.2015.09.014.
Foley RN, Curtis BM, Randell EW, Parfrey PS. Left ventricular hypertrophy in new hemodialysis patients without symptomatic cardiac disease. Clin J Am Soc Nephrol. 2010;5:805–13. https://doi.org/10.2215/CJN.07761109.
• Anker MS, von Haehling S, Landmesser U, Coats AJS, Anker SD. Cancer and heart failure-more than meets the eye: common risk factors and co-morbidities. Eur J Heart Fail. 2018;20(10):1382–4. https://doi.org/10.1002/ejhf.1252. Worldwide more than 32 million patients suffer from cancer, and more than 23 million from heart failure. Estimates for frequency of cardiovascular deaths in 1.2 million cancer patients. Researches in the field of cardio‐oncology has markedly increased in the last few years and are rapidly gaining a better understanding of the underlying mechanisms and possible clinical targets.
Arzt M, Floras JS, Logan AG, Kimoff RJ, Series F, Morrison D, et al. Suppression of central sleep apnea by continuous positive airway pressure and transplant-free survival in heart failure: a post hoc analysis of the Canadian Continuous Positive Airway Pressure for Patients with Central Sleep Apnea and Heart Failure. Trial Circul. 2007;115:3173–80. https://doi.org/10.1161/CIRCULATIONAHA.106.683482.
Gottlieb DJ, Yenokyan G, Newman AB, O'Connor GT, Punjabi NM, Quan SF, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122:352–60. https://doi.org/10.1161/CIRCULATIONAHA.109.901801.
Gupta A, Quan SF, Oldenburg O, Malhotra A, Sharma S. Sleep-disordered breathing in hospitalized patients with congestive heart failure: a concise review and proposed algorithm. Heart Fail Rev. 2018;23:701–9. https://doi.org/10.1007/s10741-018-9715-y.
• Yoshihisa A, Takeishi Y. Heart failure and sleep disordered breathing. J Med Sci. 2017. This review explores emerging data on the cost effectiveness and outcome of early intervention with PAP in hospitalized CHF patients.
Sin DD, Logan AG, Fitzgerald FS, Liu PP, Bradley TD. Effects of continuous positive airway pressure on cardiovascular outcomes in heart failure patients with and without Cheyne-Stokes respiration. Circulation. 2000;102:61–6. https://doi.org/10.1161/01.CIR.102.1.61.
Khayat R, Jarjoura D, Porter K, Sow A, Wannemacher J, Dohar R, et al. Sleep disordered breathing and post-discharge mortality in patients with acute heart failure. Eur Heart J. 2015;36:1463–9. https://doi.org/10.1093/eurheartj/ehu522.
Mechanisms of reduced sleepiness symptoms in heart failure and obstructive sleep apnea, (2019).
Emdin M, Mirizzi G, Giannoni A, Poletti R, Iudice G, Bramanti F et al., editors. Prognostic significance of central apneas throughout a 24-hour period in patients with heart failure 2017.
Daubert MA, Whellan DJ, Woehrle H, Tasissa G, Anstrom KJ, Lindenfeld JA, et al. Treatment of sleep-disordered breathing in heart failure impacts cardiac remodeling: insights from the CAT-HF Trial. Am Heart J. 2018;201:40–8. https://doi.org/10.1016/j.ahj.2018.03.026.
Cowie MR, Gallagher AM, editors. Sleep disordered breathing and heart failure what does the future hold? 2017.
• Seferovic PM, Ponikowski P, Anker SD, Bauersachs J, Chioncel O, Cleland JGF, et al. Clinical practice update on heart failure 2019: pharmacotherapy, procedures, devices and patient management. In: An expert consensus meeting report of the Heart Failure Association of the European Society of Cardiology. New York: John Wiley and Sons Ltd; 2019. The report describes how these guidance statements are supported by evidence, it makes some practical comments, and it highlights new research areas and how progress might change the clinical management of HF.
Design of the effect of adaptive servo-ventilation on survival and cardiovascular hospital admissions in patients with heart failure and sleep apnoea: the ADVENT-HF trial, (2017).
Abraham WT, Jagielski D, Oldenburg O, Augostini R, Krueger S, Kolodziej A, et al. Phrenic nerve stimulation for the treatment of central sleep apnea. JACC: Heart Failure. 2015;3:360–9. https://doi.org/10.1016/j.jchf.2014.12.013.
Costanzo MR, Ponikowski P, Javaheri S, Augostini R, Goldberg L, Holcomb R, et al. Transvenous neurostimulation for central sleep apnoea: a randomised controlled trial. Lancet. 2016;388:974–82. https://doi.org/10.1016/S0140-6736(16)30961-8.
Fox H, Oldenburg O, Javaheri S, Ponikowski P, Augostini R, Goldberg LR, et al. Long-term efficacy and safety of phrenic nerve stimulation for the treatment of central sleep apnea. Sleep. 2019;42:1–9. https://doi.org/10.1093/sleep/zsz158.
Thyroid hormone and heart failure, (2006).
Kannan L, Shaw PA, Morley MP, Brandimarto J, Fang JC, Sweitzer NK, et al. Thyroid dysfunction in heart failure and cardiovascular outcomes. Circ Heart Fail. 2018;11:e005266. https://doi.org/10.1161/CIRCHEARTFAILURE.118.005266.
Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC), (2010).
Siu CW, Jim MH, Zhang X, Chan YH, Pong V, Kwok J, et al. Comparison of atrial fibrillation recurrence rates after successful electrical cardioversion in patients with hyperthyroidism-induced versus non-hyperthyroidism-induced persistent atrial fibrillation. Am J Cardiol. 2009;103:540–3. https://doi.org/10.1016/j.amjcard.2008.10.019.
Mechanisms in endocrinology: heart failure and thyroid dysfunction., (2012).
Moruzzi P, Doria E, Agostoni PG. Medium-term effectiveness of L-thyroxine treatment in idiopathic dilated cardiomyopathy. Am J Med. 1996;101:461–7. https://doi.org/10.1016/s0002-9343(96)00281-1.
Jessup M, Abraham WT, Casey DE, Feldman AM, Francis GS, Ganiats TG, et al. Focused update: ACCF/AHA guidelines for the diagnosis and management of heart failure in adults. Circulation. 2009;119:1977–2016. https://doi.org/10.1161/CIRCULATIONAHA.109.192064.
Alagiakrishnan K, Mah D, Ahmed A, Ezekowitz J. Cognitive decline in heart failure. Heart Fail Rev. 2016;21(6):661–73. https://doi.org/10.1007/s10741-016-9568-1.
Cameron J, Gallagher R, Pressler SJ. Detecting and managing cognitive impairment to improve engagement in heart failure self-care. Curr Heart Fail Rep. 2017;14(1):13–22. https://doi.org/10.1007/s11897-017-0317-0.
Agarwal KS, Kazim R, Xu J, Borson S, Taffet GE. Unrecognized cognitive impairment and its effect on heart failure readmissions of elderly adults. J Am Geriatr Soc. 2016;64(11):2296–301. https://doi.org/10.1111/jgs.14471.
van der Wal HH, van Deursen VM, van der Meer P, Voors AA. Comorbidities in heart failure. Handbook of experimental pharmacology: Springer New York LLC; 2017. p. 35–66.
Cuomo A, Rodolico A, Galdieri A, Russo M, Campi G, Franco R, et al. Heart failure and cancer: mechanisms of old and new cardiotoxic drugs in cancer patients. Card Fail Rev. 2019;5(2):112–8. https://doi.org/10.15420/cfr.2018.32.2.
• Bertero E, Ameri P, Maack C. Bidirectional relationship between cancer and heart failure: old and new issues in cardio-oncology. Card Fail Rev. 2019;5(2):106–11. https://doi.org/10.15420/cfr.2019.1.2. It has been proposed that HF might represent an oncogenic condition. This hypothesis is supported by preclinical studies demonstrating that hyperactivation of the sympathetic nervous system and renin–angiotensin–aldosterone system, which is a hallmark of HF, promotes cancer growth and dissemination.
Banke A, Schou M, Videbaek L, Moller JE, Torp-Pedersen C, Gustafsson F, et al. Incidence of cancer in patients with chronic heart failure: a long-term follow-up study. Eur J Heart Fail. 2016;18(3):260–6. https://doi.org/10.1002/ejhf.472.
Hasin T, Gerber Y, Weston SA, Jiang R, Killian JM, Manemann SM, et al. Heart failure after myocardial infarction is associated with increased risk of cancer. J Am Coll Cardiol. 2016;68(3):265–71. https://doi.org/10.1016/j.jacc.2016.04.053.
Levis BE, Binkley PF, Shapiro CL. Cardiotoxic effects of anthracycline-based therapy: what is the evidence and what are the potential harms? Lancet Oncol. 2017;18(8):e445–e56. https://doi.org/10.1016/S1470-2045(17)30535-1.
Snipelisky D, Park JY, Lerman A, Mulvagh S, Lin G, Pereira N, et al. How to develop a cardio-oncology clinic. Heart Fail Clin. 2017;13(2):347–59. https://doi.org/10.1016/j.hfc.2016.12.011.
Totzeck M, Mincu RI, Heusch G, Rassaf T. Heart failure from cancer therapy: can we prevent it? ESC Heart Fail. 2019;6(4):856–62. https://doi.org/10.1002/ehf2.12493.
Bertero E, Canepa M, Maack C, Ameri P. Linking heart failure to Cancer. Circulation. 2018;138(7):735–42. https://doi.org/10.1161/CIRCULATIONAHA.118.033603.
Canli O, Nicolas AM, Gupta J, Finkelmeier F, Goncharova O, Pesic M, et al. Myeloid cell-derived reactive oxygen species induce epithelial mutagenesis. Cancer Cell. 2017;32(6):869–83 e5. https://doi.org/10.1016/j.ccell.2017.11.004.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors of this article declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardiovascular Care
Rights and permissions
About this article
Cite this article
Duraes, A.R., Filho, C.R.H., de Souza Lima Bitar, Y. et al. Heart Failure and Comorbidities—Part 1. Curr Emerg Hosp Med Rep 8, 60–68 (2020). https://doi.org/10.1007/s40138-020-00210-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40138-020-00210-9