Abstract
Introduction
There is little understanding of long-term treatment persistence in patients receiving anti-vascular endothelial growth factor (anti-VEGF) injections for diabetic macular edema (DME), particularly relating to treatment intervals. The aim of this study was to investigate the association between treatment interval and discontinuation rate after 24 months of unilateral anti-VEGF treatment in patients with DME under routine clinical care in the USA.
Methods
This was a non-interventional, retrospective cohort study to review the health insurance claims of adults with DME linked with the IBM MarketScan® Commercial and Medicare Supplemental databases, who were continuously enrolled in a health plan for at least 6 months prior to their first anti-VEGF treatment and for a duration of at least 24 months between July 2011 and June 2017. Patients were grouped on the basis of the injection interval they achieved at 24 months of treatment. Discontinuation rate beyond 24 months and its association with treatment intervals at 24 months was estimated using the Kaplan–Meier method and Cox proportional hazards models.
Results
The overall discontinuation rate among the 1702 eligible patients from 24 to 60 months after treatment initiation was 30%. At 60 months, patients were more likely to remain on treatment in shorter (75.3% [4-week interval group]) versus longer treatment interval groups (62.1% [> 12-week interval group], difference = 13.2%, [95% confidence interval (CI) 1.06, 2.06], p = 0.01). Patients on a > 12-week interval were twice as likely to discontinue treatment compared with those on an 8-week interval (hazard ratio = 2.01 [95% CI 1.43, 2.82], p < 0.001).
Conclusion
Patients with DME on longer anti-VEGF treatment intervals at 24 months consistently had higher discontinuation rates in the following years than those on shorter treatment intervals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Evidence suggests that patients with diabetic macular edema (DME) who do not adhere to therapy have a higher rate of clinically significant visual loss than patients who adhere to standard clinical practice. |
This study aimed to assess the association between treatment interval and a later possibility of discontinuing anti-vascular endothelial growth factor treatment in patients with DME in a real-world setting in the USA. |
What was learned from the study? |
In this cohort study, the overall discontinuation rate from 24 months until 60 months after initiation of therapy was 30%. At 60 months, patients were 13% more likely to remain on treatment when they belonged to the 4-week interval group versus the > 12-week interval group. |
The findings of this study support the need to investigate the reasons why patients with DME on long treatment intervals at 24 months tend to be less persistent with their treatment in the following years. |
Attention should be paid to encourage follow-up in this group of patients with long treatment intervals. |
Introduction
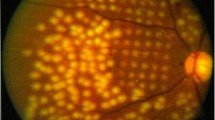
Diabetic macular edema (DME) is the most common ocular complication associated with type 1 and type 2 diabetes [1,2,3]. DME burden may see an upsurge as the global prevalence of diabetes is predicted to rise by more than 50% from 2000 to 2030, reaching an estimated 300 million cases by 2025 [4, 5]. In the United States (USA) and Europe, the prevalence of DME among patients with diabetes has been found to be 3.8% and 3.7%, respectively [6,7,8].
Over the last few decades, treatment options for DME have evolved considerably with intravitreal anti-vascular endothelial growth factor (anti-VEGF) injections becoming first-line therapy over focal/grid lasers or steroid injections [9,10,11]. Patients with DME are typically younger than those with other common forms of visual impairment, such as neovascular age-related macular degeneration and belong to the working-age population (average age at diagnosis is 50 years) [12]. Managing multiple health comorbidities and concomitant medications can result in suboptimal persistence to treatment and outcomes in DME, and increased healthcare resource utilization [13,14,15].
Treatment persistence with regular follow-up is crucial for better long-term visual outcomes. However, persistence can be difficult to achieve because of the need for frequent intravitreal injections at specialized sites. Evidence suggests that patients with DME who are not persistent to treatment experience a higher rate of clinically significant vision loss compared with patients who are persistent in routine clinical practice [16].
To date, there is little understanding of treatment persistence in patients receiving anti-VEGF injections for DME, particularly in relation to treatment intervals. The purpose of this study was to assess the association between treatment interval and the later likelihood of anti-VEGF treatment discontinuation among patients with DME under routine clinical care in the USA.
Methods
Study Design and Population Selection
We conducted a non-interventional, retrospective cohort analysis of health insurance claims data of patients from the USA who received anti-VEGF treatment for DME for the first time between 1 July 2011 and 30 June 2017 (inclusive). The study period was from 1 January 2011 to 30 June 2020 and data analysis was conducted from October 2021 to February 2022. This study followed Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
Data for this analysis were extracted from the IBM MarketScan® Commercial and Medicare Supplemental databases [17]. Authors received permission to use and access the database from the database owner. These databases provide unique identifiers that allow enrollees to be followed up across institutions and clinicians, and over time, while preserving their full anonymity. All enrollment records and inpatient, outpatient, ancillary, and drug claims were collected in accordance with the Health Insurance Portability and Accountability Act (https://www.cdc.gov/phlp/publications/topic/hipaa.html). As this study constituted of secondary analyses on fully anonymized data, institutional review board or additional informed consent was not required (https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/index.html). Patients with DME were identified, and comorbidities were assessed using International Classification of Diseases 9th/10th Revision Clinical Modification (ICD-9/10-CM) codes and anti-VEGFs (ranibizumab, aflibercept, or bevacizumab) were identified using National Drug Codes published by the US Food and Drug Administration (Supplementary Material Table S1) [18, 19].
Adults with DME, who were continuously enrolled in a health plan for at least 6 months prior to the date of their first anti-VEGF treatment (cohort entry date) and for a duration of at least 24 months following cohort entry (exposure assessment window; Study Design in Fig. 1; adapted from Schneeweiss et al. 2019) were included [20]. The cohort was restricted to patients with DME who did not receive anti-VEGF treatment at any time (at least 6 months) prior to cohort entry. This ensured the exclusion of heterogeneous data from patients who had received multiple lines of treatment over the long term [21]. Time was counted from the first anti-VEGF injection. Patients were grouped on the basis of their injection interval at 24 months. Covariates (age at first anti-VEGF injection, sex, treatment interval group, Charlson Comorbidity Index [CCI] score [0, 1, 2, 3+], treatment type [bevacizumab, aflibercept, or ranibizumab]), and baseline conditions were assessed within the 6 months prior to or at cohort entry. Sex was defined as the gender of the patient on admissions, services, outpatient claims and prescription drug claims, of covered life on populations.
Study design. The study design is adapted from Schneeweiss et al. 2019 [20]. The study period was from 1 January 2011 to 30 June 2020. Eligibility criteria and data on covariates and baseline characteristics were assessed in the 6 months prior to the cohort entry date (date of the first anti-VEGF injection). Treatment interval groups and evidence of bilateral treatment were assessed during the 24-month exposure assessment window. The follow-up window began on the day following the exposure assessment window and continued until the end of the study period, end of continuous health plan enrollment, or discontinuation of anti-vascular endothelial growth factor treatment. DME, diabetic macular edema; VEGF, vascular endothelial growth factor
Evidence of bilateral treatment and treatment interval groups were assessed during the 24-month exposure assessment window. Medication is attributed to a patient in the database, not to an eye, so it is not possible to assess treatment interval for patients treated bilaterally. Consequently, patients with evidence of bilateral use of anti-VEGF within 24-month exposure assessment window, defined as the presence of at least one period of ≤ 15 days between any two anti-VEGF injections, were excluded from the analysis. Treatment interval at 24 months was defined in the remaining unilateral patients as the average treatment interval over the last three intervals in the exposure assessment window.
Follow-up began on the day following the 24-month exposure assessment window and continued until the earliest of the following censoring events: end of the study period (30 June 2017); end of continuous health plan enrollment; or discontinuation of any anti-VEGF treatment. Patients were considered to have discontinued treatment if they did not receive anti-VEGF injection(s) for at least 12 months in any healthcare setting while still enrolled in a health plan, regardless of any subsequent injection after the 12-month period.
Study Outcomes
The first study aim was to report the discontinuation rate after 24 months of anti-VEGF treatment until 36, 48, and 60 months and time-to-discontinuation based on treatment interval groups at 24 months (4-week [16–34 days], 6-week [35–48 days], 8-week [49–62 days], 10-week [63–76 days], 12-week [77–90 days], and > 12-week [> 90 days]).
The second aim was to assess the characteristics of patients with DME within each treatment interval group: demographic (sex, age at cohort entry [continuous], calendar year of cohort entry, age group [18–39, 40–64, 65–74, and 75+], region of residence, employment status, and payer type) and clinical characteristics (CCI score and specific comorbidities [Supplementary Material Table S2]) at cohort entry; and to assess discontinuation rates and time-to-discontinuation based on injection number (1–3, 4–8, 9–13, 14–18, 19–23, and ≥ 24 injections) in the 24 months following cohort entry.
The following sensitivity analyses were defined a priori and performed simultaneously to the primary analysis to support findings: (1) time-to-discontinuation in patients that discontinued treatment permanently (i.e., no further injections observed following the 12-month discontinuation period); (2) time-to-discontinuation in patients for whom further injections were observed following the 12-month period without anti-VEGF use; (3) an analysis using a discontinuation period of 6 months as opposed to 12 months (including both patients that discontinued permanently and those who received further injections following the discontinuation period); and (4) analysis using periods of ≤ 21 days and ≤ 25 days (as opposed to 15 days) to define bilateral anti-VEGF treatment.
Statistical Analyses
Demographic and clinical characteristics were descriptively summarized. The Kaplan–Meier method was used to estimate time-to-discontinuation and the log-rank test to analyze the differences between treatment interval groups. p values were based on two-sided tests and were not adjusted for multiple analyses. Mean time-to-discontinuation was estimated, and multivariable-adjusted Cox proportional hazard models were used to identify the factors associated with the likelihood of discontinuation. The primary model used treatment interval at 24 months as the predictor of interest with adjustment made for the sex, age at first anti-VEGF injection, CCI score, injection type, and year of cohort entry.
Several alternative model analyses were also performed to examine the robustness of the primary model (Supplementary Material Table S3). Alternative models 1 and 2 did not include adjustment for CCI score and models 2 and 3 included a set of two-way interactions allowing the impact of treatment intervals to vary across type of anti-VEGF agent. Statistical analyses were conducted using R software version 3.4.3 (2017-11-30) [22].
Additional sensitivity analyses to evaluate the impact on treatment discontinuation of being of working/retirement age (defined as 18–65/> 65 years old) and presence/absence of vitrectomy or focal/grid laser procedures were performed using Cox proportional hazard models (Supplementary Material Table S4).
Results
The analysis cohort included 1702 continuously enrolled patients who had a DME diagnosis in the 6 months prior to the first anti-VEGF injection and were on continuous unilateral anti-VEGF treatment for at least 24 months following the first anti-VEGF injection. Of 13,155 eligible patients continuously enrolled in a health plan for 24 months following their first anti-VEGF injection, 9726 (74%) patients discontinued treatment in the first 24 months and were not included in the final analysis cohort: 47% of patients who discontinued within 24 months did so within the first 3 months, 79% did so within the first year, and 21% discontinued in the second year. Among patients with continuous treatment for 24 months, 49.7% had evidence of bilateral anti-VEGF use and were also excluded from the analysis cohort (Supplementary Material Fig. S1).
Baseline demographics and clinical characteristics of the analysis cohort were well balanced between treatment interval groups (Supplementary Material Table S2). Briefly, the mean (SD [standard deviation]) age of the analysis population was 60.7 (12.0) years with the majority (66%) in the 40–65 years age group; most patients were men (55%). At cohort entry, 53%, 25%, and 22% had been treated with bevacizumab, ranibizumab, and aflibercept, respectively. The mean (SD) CCI score at the time of the first anti-VEGF injection was 2.4 (2). The most prevalent comorbidities were hypertension (66%) and elevated cholesterol (58%; Supplementary Material Table S2). The ICD-9/10-CM diagnoses codes used for diagnosis of comorbidities “hypertension” and “elevated cholesterol” are detailed in Supplementary Material Table S5.
As per assignment to treatment interval group at 24 months, the majority of patients were on a longer (> 12 weeks) treatment regimen: 4-week group (n = 116); 6-week group (n = 352); 8-week group (n = 333); 10-week group (n = 248); 12-week group (n = 186); and > 12-week group (n = 467). The mean (SD) numbers of injections during the first and second year of treatment were 7 (2.7) and 6 (2.6), respectively.
The overall discontinuation rate at 60 months, including 24 months of continuous anti-VEGF treatment (i.e., primary outcome measure), was 30.0%. Kaplan–Meier survival analysis of time-to-discontinuation suggested that patients were more likely to discontinue treatment in the longer versus shorter treatment interval groups (p < 0.001; Fig. 2) beyond 24 months. At 60 months, fewer patients remained on anti-VEGF treatment in the > 12-week interval group (62.1%) compared with the 4-week interval (75.3%) group (Table 1), difference = 13.2%, 95% confidence interval (CI) 1.06, 2.06; p = 0.01. Similarly, an increase in discontinuation with treatment interval was also evidenced from 24 to 36 months (11% fewer patients remaining in the > 12-week vs 4-week interval group; 95% CI 0.91, 1.46; p = 0.01) and 48 months (12% fewer patients remaining in the > 12-week vs 4-week interval group; 95% CI 1.00, 1.77; p = 0.005).
Primary outcome measure: Time-to-discontinuation following 24 months of treatment based on treatment interval (4-week [16–34 days], 6-week [35–48 days], 8-week [49–62 days], 10-week [63–76 days], 12-week [77–90 days], and > 12-week [> 90 days]). Kaplan–Meier survival curve of time-to-discontinuation by average treatment interval over the three injections prior to and including the 24-month visit of the exposure assessment window. The log-rank test for equality of survival functions indicates differences between treatment interval groups. VEGF, vascular endothelial growth factor
This result held true after correction for sex, age at first anti-VEGF injection, CCI score, injection type, and year of cohort entry. Estimated hazard ratios (HR) from the primary multivariable-adjusted Cox proportional hazard model demonstrated that patients on longer treatment intervals beyond 24 months had an increased risk of discontinuation (10-week interval group, HR [95% CI)] 1.17 [0.79, 1.77]; 12-week interval group, HR [95% CI] 1.97 [1.27, 3.04], p = 0.002; reference, 8-week interval group) (Table 2). Patients from the > 12-week interval group were twice as likely to discontinue treatment compared with those in the 8-week interval group (HR [95% CI] 2.01 [1.43, 2.82], p < 0.001) (Table 2).
The result on discontinuation increasing with injection interval also held true regardless of whether patients were of retirement age (defined here as > 65 years old) or not, although the findings were not significant (HR [95% CI] 1.20 [0.81–1.79], p < 0.345] (Supplementary Material Table S4). Sensitivity analyses of the subset of 866 patients who never received vitrectomy and/or focal/grid laser interventions reported hazard ratios for the treatment interval groups 10, 12, and > 12 weeks as 1.94, 3.54, and 2.74, respectively, with significant p values of 0.04, 0.0004, and 0.0012.
Additional modelling confirmed that the observed effects were robust. We re-ran the analysis using alternative models with different model specifications. The results from the three models supported the main model that patients on longer treatment intervals have an increased risk of treatment discontinuation (Supplementary Material Table S3).
Sensitivity analyses supported the outcomes of the primary analysis. Namely, the same finding of increased discontinuation in patients with longer treatment intervals beyond 24 months was observed in sensitivity analyses conducted for (a) patients that discontinued treatment permanently, (b) patients for whom further injections were observed following the 12-month discontinuation period, (c) a discontinuation period of 6 months, (d, e) and bilateral disease periods of ≤ 21 days and ≤ 25 days (Supplementary Material Fig. S2).
Results of the association between the number of injections within the 24-month exposure assessment period and anti-VEGF treatment discontinuation beyond 24 months of treatment were consistent with the primary analysis (Fig. 3). For patients stratified into groups of 1–3, 4–8, 9–13, 14–18, 19–23, and ≥ 24 injections in the first 24 months of treatment, time-to-discontinuation was shorter for patients with fewer injections.
Time-to-discontinuation based on number of injections (1–3, 4–8, 9–13, 14–18, 19–23, and ≥ 24 injections) in the 24-month exposure assessment window. Kaplan–Meier survival curve of time-to-discontinuation. The log-rank test for equality of survival functions indicates differences between treatment interval groups. VEGF, vascular endothelial growth factor
Discussion
This retrospective, non-interventional cohort study of the US claims data from patients with DME treated with anti-VEGF treatments in a routine clinical care setting indicated that patients with DME on longer treatment intervals (≥ 12 weeks) at the end of their first 24 months of treatment had an increased likelihood of anti-VEGF treatment discontinuation in the years beyond. The results were supported by analyses on an alternative variable to define treatment intensity in the first 24 months (number of injections instead of last treatment interval) and were robust to sensitivity analyses around patients that discontinued treatment permanently, and to population adjustments based on patient demographic and clinical characteristics at the start of anti-VEGF treatment. To our knowledge, this is the first analysis investigating the association between anti-VEGF injection interval and discontinuation in patients with DME. This is also the first time such a result is reported, and it is contrary to the popular belief that a high treatment burden leads to increased discontinuation in patients with DME.
The overall discontinuation rate of 30% from 24 to 60 months observed in our study corresponded well with another study of patients with DME in a similar setting, which reported 28% discontinuation during the first 24 months of anti‐VEGF therapy [23]. In the Fight Retinal Blindness! Study, comparing 12-month anti-VEGF treatment outcomes in routine clinical practice, the discontinuation rate in treatment-naïve patients with DME was lower (16%); however, the sample size (n = 383) was smaller than for the current study [24]. A more recent analysis that included clinical trials of anti-VEGFs for the treatment of DME reported a mean discontinuation rate of 14% over a median study duration of 1 year (range 12 weeks–3 years) [25]; however, these rates are expected to be lower than those in a real-world scenario because clinical trials are often designed to include homogenous and highly specific patient populations with many resources to reduce patient dropout.
Identification of factors associated with treatment persistence and reasons for discontinuation (e.g., treatment burden, lack of continued efficacy) and the associated exit strategies (e.g., switch to corticosteroid therapy) can be helpful in developing strategies to improve the visual function of patients with diabetes. As reasons for discontinuations were not available from our database, we investigated instead factors associated with treatment persistence.
Treatment interval patterns during the last three intervals before 24 months show that 27.4% patients from our study were on a longer (> 12 weeks) treatment regimen at 24 months after the start of the anti-VEGF treatment. Patients in this > 12-week interval subgroup were twice as likely to discontinue treatment compared with the 8-week interval group. The higher discontinuation observed for this subgroup could partly be attributable to patients not fully recognizing the usefulness of treatment when they have longer treatment intervals, lower disease activity, and a lack of noticeable improvement after every injection—which taken together could lead to the perception among patients that treatment is no longer required.
Patients with diabetes have complex comorbidity profiles, which might not allow injections to be given at regular intervals [15]. Overall healthcare utilization is also reported to be high for patients with DME [26]. In patients with more active disease, frequent treatment (e.g., monthly) can lead to treatment fatigue resulting in lack of treatment persistence, which can be minimized through adaptive treatment regimens such as treat and extend or pro re nata. Owing to the heterogeneity of the claims data, it was not possible to determine whether treat and extend or pro re nata regimens were applied.
Overall, the proportion of patients still receiving either monthly or bimonthly treatment at 24 months was approximately 47%, highlighting a high proportion of patients with “high treatment burden”, i.e., being treated at most every 8 weeks. The burden of treatment would be less if longer injection intervals correlated with longer visit intervals, enabling patients to travel less to their treatment site. Data on patient visits without an injection versus with an injection were not explored in this analysis, however, and would make an interesting topic for further study.
The burden of frequent injections for DME treatment is often particularly felt for working age patients (approximately 70% of patients in this analysis), given the need for frequent absences from work to attend appointments. Longer treatment intervals would be expected to have a favorable impact on continuing treatment in this population. However, our analyses did not detect any impact of being of working age on discontinuation between 24 and 60 months after treatment initiation.
The patients with DME receiving the most frequent injections had the highest persistence with treatment in this analysis. As a result of a lack of visual acuity and anatomical data, however, it was not possible to discriminate between patients who were lost to follow-up and intentional discontinuation by patients and their physicians because of treatment futility or resolution of disease activity. Interventions like vitrectomy and/or focal/grid laser procedures may provide longer-lasting resolution of DME potentially leading to treatment discontinuation [27]. Again, in this analysis, we observed that patients without vitrectomy and/or focal/grid laser procedures also reported a higher discontinuation rate with longer injection interval at 24 months, so that possible resolution of DME following vitrectomy and/or focal/grid laser procedure does not appear to be the driver of increased discontinuation in the longer injection interval group. Further research should be conducted in databases that contain clinical and/or patient-reported outcomes, and/or treatment strategies, to determine the reasons for greater treatment discontinuation in patients with longer treatment intervals, which was not possible in the current analysis.
The strength of our study includes an analysis population from a large database with over 1700 patients with DME receiving anti-VEGFs in a routine clinical care setting from the USA with a long follow-up time of several years. However, a few limitations of this study should also be considered. MarketScan is a US-based claims database that contains information on patients enrolled in health insurance programs [17, 28]. This makes it reliant upon the accuracy of the medical coding and billing information. Thus, medication use may be overestimated in such databases, since drug prescriptions are used as a proxy for medication use; furthermore, the analysis may also be affected by unobserved differences between patients, and deceased patients may remain in the dataset for a certain period. Also, in our analysis it was not possible to distinguish between patients treated unilaterally or bilaterally, which was addressed through the exclusion of patients with consecutive treatments within 15 days. The proportion of patients with evidence of bilateral injections in the first 24 months was 49.7%, which is in line with proportions reported in previous studies for patients with DME [29, 30]. These patients were excluded from the analysis; only patients who had unilateral anti-VEGF in the first 24 months were studied. Another area of future investigation could be whether the change in visual acuity from the onset of anti-VEGF treatment is predictive of risk of discontinuation.
Conclusion
Our results emphasize that patients are able to tolerate a higher treatment burden. These findings should encourage physicians to continue to treat patients in accordance with their disease activity without the worry that patients will “burn out”. Also, patients on longer injection intervals can still be seen regularly in clinic in between injection visits. Reinforcing the need for ongoing treatment may be important for patients on longer intervals, who may feel complacent or that treatment is no longer effective, particularly if newer agents become widely available that are longer lasting without sacrificing visual acuity outcomes noted with current available agents.
References
Rose MA, Vukicevic M, Koklanis K. Adherence of patients with diabetic macular oedema to intravitreal injections: a systematic review. Clin Exp Ophthalmol. 2020;48(9):1286–98.
Salem W, Fraser-Bell S, Gillies M. Clinical development of new treatments for diabetic macular oedema. Clin Exp Optom. 2012;95(3):297–305.
Lee R, Wong TY, Sabanayagam C. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis. 2015;2:17.
Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–53.
King H, Aubert RE, Herman WH. Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998;21(9):1414–31.
Chen E, Looman M, Laouri M, et al. Burden of illness of diabetic macular edema: literature review. Curr Med Res Opin. 2010;26(7):1587–97.
Varma R, Bressler NM, Doan QV, et al. Prevalence of and risk factors for diabetic macular edema in the United States. JAMA Ophthalmol. 2014;132(11):1334–40.
Li JQ, Welchowski T, Schmid M, et al. Prevalence, incidence and future projection of diabetic eye disease in Europe: a systematic review and meta-analysis. Eur J Epidemiol. 2020;35(1):11–23.
Ho AC, Scott IU, Kim SJ, et al. Anti-vascular endothelial growth factor pharmacotherapy for diabetic macular edema: a report by the American Academy of Ophthalmology. Ophthalmology. 2012;119(10):2179–88.
Jusufbegovic D, Mugavin MO, Schaal S. Evolution of controlling diabetic retinopathy: changing trends in the management of diabetic macular edema at a single institution over the past decade. Retina. 2015;35(5):929–34.
Lally DR, Shah CP, Heier JS. Vascular endothelial growth factor and diabetic macular edema. Surv Ophthalmol. 2016;61(6):759–68.
Petrella RJ, Blouin J, Davies B, Barbeau M. Prevalence, demographics, and treatment characteristics of visual impairment due to diabetic macular edema in a representative Canadian cohort. J Ophthalmol. 2012;2012: 159167.
Weiss M, Sim DA, Herold T, et al. Compliance and adherence of patients with diabetic macular edema to intravitreal anti-vascular endothelial growth factor therapy in daily practice. Retina. 2018;38(12):2293–300.
Zhou B, Mitchell TC, Rusakevich AM, Brown DM, Wykoff CC. Noncompliance in prospective retina clinical trials: analysis of factors predicting loss to follow-up. Am J Ophthalmol. 2020;210:86–96.
Kiss S, Chandwani HS, Cole AL, Patel VD, Lunacsek OE, Dugel PU. Comorbidity and health care visit burden in working-age commercially insured patients with diabetic macular edema. Clin Ophthalmol. 2016;10:2443–53.
Ehlken C, Helms M, Böhringer D, Agostini HT, Stahl A. Association of treatment adherence with real-life VA outcomes in AMD, DME, and BRVO patients. Clin Ophthalmol. 2017;12:13–20.
Butler AMNK, Overman RA, Brookhart MA. IBM MarketScan research databases. In: Sturkenboom MST, editor. Databases for pharmacoepidemiological research springer series on epidemiology and public health. Cham: Springer; 2021. p. 243–51.
National Center for Health Statistics. Centers for Disease Control and Prevention. Classification of diseases, functioning, and disability. https://www.cdc.gov/nchs/icd/. Accessed 24 Nov 2021.
U.S. Food & Drug Administration. National Drug Code Directory. https://www.fda.gov/drugs/drug-approvals-and-databases/national-drug-code-directory. Accessed 24 Nov 2021.
Schneeweiss S, Rassen JA, Brown JS, et al. Graphical depiction of longitudinal study designs in health care databases. Ann Intern Med. 2019;170(6):398–406.
Danaei G, Tavakkoli M, Hernan MA. Bias in observational studies of prevalent users: lessons for comparative effectiveness research from a meta-analysis of statins. Am J Epidemiol. 2012;175(4):250–62.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna; 2017. https://www.r-project.org/.
Peto T, Akerele T, Sagkriotis A, Zappacosta S, Clemens A, Chakravarthy U. Treatment patterns and persistence rates with anti-VEGF treatment for diabetic macular edema in the UK: a real-world study. Diabet Med. 2022;39(4):e14746.
Bhandari S, Nguyen V, Fraser-Bell S, et al. Ranibizumab or aflibercept for diabetic macular edema: comparison of 1-year outcomes from the Fight Retinal Blindness! registry. Ophthalmology. 2020;127(5):608–15.
Rosenblatt TR, Rayess N, Al-Moujahed A, Khurana RN, Mruthyunjaya P. Discontinuation and loss to follow-up rates in clinical trials of intravitreal anti-vascular endothelial growth factor injections. Graefes Arch Clin Exp Ophthalmol. 2022;260(1):93–100.
Wallick CJ, Hansen RN, Campbell J, Kiss S, Kowalski JW, Sullivan SD. Comorbidity and health care resource use among commercially insured non-elderly patients with diabetic macular edema. Ophthalmic Surg Lasers Imaging Retina. 2015;46(7):744–51.
Kim EJ, Lin WV, Rodriguez SM, Chen A, Loya A, Weng CY. Treatment of diabetic macular edema. Curr Diab Rep. 2019;19(9):68.
The Henry J. Kaiser Family Foundation. Health insurance coverage of the total population. http://kff.org/other/state-indicator/total-population/. Accessed 24 Nov 2021.
Giocanti-Auregan A, Tadayoni R, Grenet T, et al. Estimation of the need for bilateral intravitreal anti-VEGF injections in clinical practice. BMC Ophthalmol. 2016;16:142.
Ness S, Green M, Loporchio D, et al. Risk factors for fellow eye treatment in protocol T. Graefes Arch Clin Exp Ophthalmol. 2021;259(8):2203–12.
Acknowledgements
Funding
This research was funded by Novartis Pharma A.G., Basel, Switzerland. The funder participated in the study design, data analysis, interpretation of the data, preparation, review, and approval of the manuscript, and funded the journal’s Rapid Service Fee.
Medical Writing, Editorial, and Other Assistance
The authors would like to thank Patrick Ward, PhD, Abhishek Srivastava, BTech. and Sourav Biswas, MTech, in the Real-World Evidence team, Novartis Business Services CONEXTS for data analyses; Ashwini Patil, PhD of Novartis Healthcare Pvt. Ltd., India, Susan Browne, PhD, of Novartis Ireland, Ltd., and Divya Sharma, MDS of Novartis Healthcare Pvt. Ltd., India for medical writing support, under the guidance of the authors and in accordance with Good Publication Practice (GPP2022) guidelines (https://www.ismpp.org/gpp-2022). The funding for data analysis and writing support was provided by Novartis Pharma AG.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Sophie J. Bakri, Marie-Noelle Delyfer and Jakob Grauslund contributed to the research design, data analysis and/or interpretation and manuscript preparation. Helene Karcher and Steffen Andersen contributed to the research design, data acquisition and/or research execution, data analysis and/or interpretation, and manuscript preparation.
Disclosures
Sophie J. Bakri’s institution received research grants from Lowy Medical Foundation and Regenexbio. She also received consultancy fees from Adverum, Abbvie, Allergan, Apellis, Eyepoint, iLumen, Kala, Novartis, Iveric Bio, Roche and Zeiss. She also serves on the board for American Society of Retina Specialists. Marie-Noëlle Delyfer received honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Abbvie, Bayer, Horus Pharma, Novartis, and Roche. She also serves on a Data Safety Monitoring Board for Horama, Abbvie, Bayer, Horus Pharma, Novartis, Roche and Théa. She is Vice President of the French Society of Ophthalmology. Jakob Grauslund received personal fees from Novartis, Bayer, Allergan, and Roche for participation on a Data Safety Monitoring Board/advisory board. Helene Karcher is an employee and a shareholder of Novartis Pharma AG, Switzerland. Steffen Andersen is currently an employee of Novo Nordisk A/S, Denmark. All authors attest that they meet the current ICMJE criteria for authorship.
Compliance with Ethics Guidelines
Data for this analysis were extracted from the IBM MarketScan® Commercial and Medicare Supplemental databases. All enrollment records and inpatient, outpatient, ancillary, and drug claims were collected in accordance with the Health Insurance Portability and Accountability Act (https://www.cdc.gov/phlp/publications/topic/hipaa.html). As this study constituted of secondary analyses on fully anonymized data, institutional review board or additional informed consent was not required (https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/index.html).
Data Availability
The datasets generated and analyzed during the current study can be made available upon reasonable request, which may require a data access fee paid to Merative (Healthcare Data, Technology and Analytics|Merative). The data for this study consisted of anonymised patient-level data taken from the Merative MarketScan® Commercial and Medicare Supplemental databases https://www.ibm.com/products/marketscan-research-databases/databases. Data were stored and analyzed securely in Novartis’ in-house Data42 platform under a license from Merative.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bakri, S.J., Delyfer, MN., Grauslund, J. et al. Real-World Persistence and Treatment Interval in Patients with Diabetic Macular Edema Treated with Anti-Vascular Endothelial Growth Factors in the USA. Ophthalmol Ther 12, 2465–2477 (2023). https://doi.org/10.1007/s40123-023-00750-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00750-9