Abstract
Retinal vein occlusion (RVO) is the second most common retinal vascular disease. Central RVO (CRVO), in which obstruction occurs posterior to the lamina cribrosa due to various causes, manifests with extensive venous tortuosity, dilatation of blood vessels in the four quadrants, and retinal hemorrhage. The presence of macular edema decreases visual acuity in patients with CRVO, especially in elderly patients with hypertension, hyperlipidemia, and diabetes. In the last decade, treatment modalities for CRVO have improved, with anti-vascular endothelial growth factor agents being widely used as treatment. However, there are cases of refractory or recurrent macular edema. Moreover, CRVO also occurs in young patients. This article reviews previous studies and case reports and summarizes the differences in etiological factors, clinical manifestations, treatment, and prognosis between young and elderly patients. Due to the low incidence of CRVO in young patients, clinical data from these age groups are limited. Hence, further studies are warranted to explore the differences between age groups to improve individualization of treatment of young patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This article aimed to review the relevant literature regarding central retinal vein occlusion (CRVO) and summarize the differences in pathogenesis, risk factors, clinical manifestations, treatment, and prognosis between CRVO in young and elderly patients. |
Young patients having more risk factors compared with elderly patients, and inflammation, which was previously suggested as a cause for CRVO in young patients, may not necessarily be a cause of CRVO. |
Although the clinical manifestations are mostly similar between young and elderly patients with CRVO, the effectivity of treatment as well as the prognosis significantly differs between both age groups. |
Intraocular anti-vascular endothelial growth factor (VEGF) injections in elderly patients are more frequent; however, this may not translate to a better prognosis. |
Treatment of patients with CRVO should be individualized, and careful monitoring of visual acuity and regular follow-ups must be performed to improve visual outcomes in all patients. |
Introduction
Central retinal vein occlusion (CRVO) is a common retinal vascular disease, and its incidence increases with age. The primary risk factors for CRVO are hypertension, hyperlipidemia, and diabetes, and it mostly affects individuals > 60 years old. CRVO causes varying degrees of visual impairment. Currently, the literature defines CRVO cases in patients < 50 years old as CRVO in the young [1,2,3,4,5,6]. However, some studies have defined CRVO in the young as that occurring in patients either < 40 [7] or < 55 [8] years old. Regardless, no age limit has been set to define CRVO in the young. According to previous studies, the incidence of CRVO in patients < 50 years old is 0.23/1000, whereas that in patients ≥ 50 years old is 1.95/1000 [9]. CRVO in young patients accounts for 10–15% of the total number of CRVO cases [10], and most studies have shown that CRVO in young patients is more prevalent in men than in women [1, 5, 11, 12]. Young people are more sensitive to vision loss, and due to the rarity of the condition in these patients, CRVO in young patients is often reported, resulting in the overestimation of the number of cases. Due to the limited clinical data on CRVO in young patients, the understanding of this condition in this age group is also limited, and treatment of these patients may be different from that of elderly patients. Thus, this article reviews the relevant literature and mainly elaborates the differences in pathogenesis, risk factors, clinical manifestations, treatment, and prognosis between CRVO in young and elderly patients.
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Etiological Differences
The pathogenesis of CRVO can be summarized by Virchow's triad as follows: hemodynamic changes, vascular endothelial damage, and a hypercoagulable state [13]. In CRVO, retinal hypoperfusion and hemorrhage result in ischemia and hypoxia, which increase the expression of angiogenic cytokines such as vascular endothelial growth factor (VEGF) and placental growth factor, which act on VEGF receptors. Inflammatory cytokines, such as monocyte chemoattractant protein-1 and intercellular adhesion molecule-1, further reduce blood flow in the retina by enhancing chemotaxis and adhesion of leukocytes to the vascular endothelium. The continuous destruction of the blood-retinal barrier causes fluid leakage and macular edema, resulting in decreased visual acuity [14].
In the 1960s, Lyle et al. first reported CRVO in young patients without a clear etiology and compared it with Eales disease; they argued that the pathogenesis of CRVO in this population was caused by vasculitis [15]. Meanwhile, Lonn et al. observed a white layer of peripapillary veins after resolution of optic disc swelling; supporting the theory of an inflammatory mechanism for CRVO, they termed this condition papillophlebitis [16]. However, a histopathological study of CRVO in a young patient did not reveal vasculitic changes. Instead, proliferation of vascular endothelial cells and surrounding cell infiltration were similar to those of chronic inflammation [17]. Additionally, inflammation was not confined to the area of the vein of the optic nerve head. In contrast, inflammation may be a result of disease development in CRVO in young patients. Some young patients with CRVO are clinically treated with intravitreal injection of steroids such as Ozudex, as these patients respond more acutely to ischemia-hypoxia injury, which may manifest as increased levels of intraocular inflammatory factors. However, there is no straightforward evidence that inflammation is the cause of CRVO in young patients, and the condition may be a result of multifactorial interactions. Hence, the pathogenesis should not be based on the patient’s age alone. Intraocular fluid detection is an advanced diagnostic technique that was developed recently for intraocular pathogenic microorganisms and cytokines and has been widely used in clinical research. Intraocular cytokine detection may not only clarify whether there are differences in the types and contents of intraocular inflammatory factors, such as interleukin-6 and interleukin-8, between young and elderly patients but also explore the role of inflammation in the progression of CRVO in young patients.
Compared with CRVO in the elderly, the etiological factors of CRVO in young patients are more diverse. We reviewed relevant literatures on possible predisposing factors for CRVO in 413 young patients and summarize them in Table 1. In both young and elderly patients, traditional cardiovascular risk factors are closely related to the development of CRVO. Anatomically, the central retinal artery and vein run in a common fibrous sheath when they cross the optic nerve. Cardiovascular diseases, such as hypertension, damage the retinal artery endothelium, and alter the hemodynamics of adjacent veins, resulting in blood flow stasis and venous occlusion. In 485 patients, Rothman et al. reported that among young patients with CRVO, 33% had hypertension, 22% had diabetes, and 5.6% had hyperlipidemia; however, the prevalence of these diseases was higher in elderly patients (79%, 34%, and 20%, respectively) [2]. Similarly, in a retrospective study by Eah et al. that included 263 patients, hypertension, diabetes, and hyperlipidemia affected 13%, 14.5%, and 7.2% of young patients with CRVO compared with 52.6%, 25.8%, and 13.9% of elderly patients, respectively [18]. In another study, Chen et al. reported that hyperlipidemia is the most important etiological factor of CRVO in young patients [7]. This may be due to the fact that early atherosclerosis caused by hypertension and diabetes in young patients is not sufficient to cause severe CRVO. Although traditional risk factors are the main causes of CRVO in the elderly, this may not be true for young patients; however, they remain important factors in the development of CRVO this age group. Thus, traditional risk factors should be the primary considerations when determining the etiology of CRVO in young patients despite non-traditional risk factors being more common in this age group.
In young patients with CRVO, hyperviscosity syndrome (HVS) caused by certain diseases is a risk factor for thrombosis. Additionally, macroglobulinemia, multiple myeloma, iron deficiency anemia, leukemia, and hereditary spherocytosis have been reported to cause CRVO in young patients because of secondary HVS [19,20,21,22]. Furthermore, dehydration caused by high-intensity exercise in young people can increase blood viscosity and contribute to the development of CRVO [23,24,25].
Thrombophilic risk factors include hyperhomocysteinemia, elevated levels of antiphospholipid antibodies (lupus anticoagulants, anticardiolipin antibodies, anti-β2GPI antibodies), antithrombin III deficiency, activated protein C resistance, protein C deficiency, protein S deficiency, Leiden factor V, 5,1-methylenetetra-hydrofolate reductase (MTHFR), plasminogen activator inhibitor 1, prothrombin G20210A, platelet glycoprotein IIIa PIA1/A2 and I/IIa, and C807T and G873A mutations [8, 12, 26,27,28,29,30]. Bucciarelli et al. reported that elderly patients with CRVO had a higher number of risk factors associated with hyperhomocysteinemia than young patients [28]. Lahey et al. proposed that hyperhomocysteinemia is more common in young patients with CRVO than in healthy controls [31]. Hyperhomocysteinemia impairs vascular endothelial function and promotes proliferation of vascular smooth muscle cells, which may explain the association of hyperhomocysteinemia with CRVO [32]. Parodi et al. concluded that homocysteine levels are more likely to be an indicator of endothelial injury caused by cardiovascular diseases, such as hypertension and coronary heart disease, instead of being an independent risk factor for CRVO [33]. Antiphospholipid syndrome is an autoimmune disorder characterized by recurrent thrombosis, morbid pregnancy, and positive antiphospholipid antibodies. Lahey and Hernández suggested that antiphospholipid antibodies are associated with the development of CRVO [31, 34]. However, Vieira and Ahluwalia concluded that antiphospholipid antibodies are not associated with CRVO [12, 26]. Although a correlation between prothrombin mutation or factor V Leiden and CRVO in young patients has been reported [35], some studies have suggested otherwise [28, 36]. A study by Bertram et al. shows that RVO in young patients was significantly correlated with protein C, protein S, and antithrombin deficiency [37]; however, other authors have failed to demonstrate the relevance of these proteins in RVO [38]. Whether the association between blood hypercoagulability factors and CRVO in young patients is statistically significant remains controversial; however, since relevant laboratory tests are not routinely performed in patients with CRVO, these risk factors are often underestimated. Although a detailed laboratory examination of hypercoagulable factors in CRVO patients is impractical, screening for tests familial or personal thrombotic history of CRVO patients < 40 years of age is warranted if a patient has no traditional risk factors [3, 8, 39].
Meanwhile, numerous studies have shown that systemic diseases such as systemic lupus erythematosus, sarcoidosis, systemic vasculitis, rheumatoid arthritis, or infectious diseases such as acquired immunodeficiency syndrome, syphilis infection, and immune hepatitis are associated with the development of CRVO in young patients [1,2,3,4, 11]. Recently, the Coronavirus Disease-19 (COVID-19) pandemic has allowed us to gain a new perspective and further understand the risk factors for CRVO in young patients as cases of secondary CRVO after COVID-19 in healthy young men have been reported wherein pseudovasculitis or disseminated intravascular coagulation caused by viral invasion of endothelial cells may have caused CRVO [40, 41]. Association between pseudotumor cerebri and CRVO in young patients has been previously reported [7]. While the pathophysiology is not entirely understood, it is hypothesized that optic nerve swelling secondary to increased intracranial pressure impedes retinal venous return and can precipitate CRVO. Migraine headache has also been associated with young CRVO patients [7]. It has been speculated that platelet abnormalities related to migraine may predispose to CRVO.
The occurrence of CRVO in young patients is also associated with the use of certain drugs. Oral contraceptives (OCC) are associated with CRVO in women of childbearing age, and progesterone in OCC may lead to vascular endothelium proliferation and hypercoagulability [42,43,44]. To some extent, diuretics may also contribute to the development of CRVO [11]. However, because patients taking diuretics usually have systemic diseases such as hypertension, the effects of diuretics may be overestimated. Antipsychotics, such as piperidone, can also contribute to the development of CRVO by increasing the levels of antiphospholipid antibodies, thereby increasing the risk of thrombosis [45, 46].
Glaucoma, local ocular inflammatory diseases, and congenital abnormalities can also induce the development of CRVO through different mechanisms [11, 47,48,49]. The results of a recent study showed that primary open-angle glaucoma (POAG) was the most significant risk factor for CRVO in young patients [7]. There are various risk factors for CRVO in young patients; however, there are also cases of young patients with idiopathic CRVO without a clear cause. Therefore, young patients should undergo more detailed and comprehensive history taking and physical examination. Walters et al. recommended screening of the following indicators for young patients with CRVO: complete blood count, erythrocyte sedimentation rate, plasma viscosity, levels of fibrinogen, urea, electrolytes, plasma protein, and random serum glucose, fasting lipid profile, infectious disease screening, autoantibody screening, electrocardiogram, and chest radiography [50]. The results of these examinations may help clinicians better understand the etiology of CRVO in young patients and guide clinical treatment. Table 2 provides a guide for performing the work-up for CRVO in young patients.
Differences in Clinical Manifestations
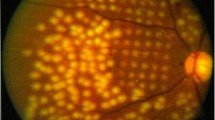
Similar to elderly patients with CRVO, the fundus of young patients with CRVO may also present with venous tortuosity and dilatation, cystoid macular edema, multiple retinal hemorrhages, optic disc edema, collateral formation, neovascularization, vitreous hemorrhage, and a prolonged venous filling period on fluorescein fundus angiography. The diagnosis of ischemic versus non-ischemic CRVO is important. Clinical manifestations of ischemic CRVO include significant visual acuity loss (< 20/200), visual field abnormalities, significant retinal hemorrhage and edema, cotton wool spots, relative afferent pupillary disorder, FFA showing extensive capillary non-perfused areas, and decreased b-wave amplitude on electroretinogram [51].
At present, most studies have shown that the baseline clinical manifestations in young patients are milder than those in elderly patients. Compared with elderly patients with CRVO, at the first visit, young patients with CRVO are less likely to have ischemic CRVO, have higher best corrected visual acuity (BCVA), have lower incidence of cystoid macular edema (CME) and subretinal fluid (SRF), have thinner central retinal thickness (CRT), and have better integrity of the external limiting membrane, elliptical zone, and retinal pigment epithelium [2, 6, 18]. As young patients are more sensitive to decreased visual acuity, the milder presentation of CRVO at baseline in these patients may be attributed to a shorter duration of symptoms prior to consult and treatment. In addition, the presence of age-related lens opacities in elderly patients may be partly responsible for the difference in baseline BCVA compared with young patients.
A study has shown that retinal vascular density, venous blood flow velocity, and inner retinal thickness in healthy people gradually decrease with age [52]. Additionally, an autoregulatory system in the retinal microcirculation exists; the presence of major risk factors in elderly patients, such as hypertension, diabetes, and other diseases, will accelerate the deterioration of the retinal microcirculation and destroy the autoregulatory system. Alternatively, age is negatively correlated with choroidal thickness [53], and a thicker choroid in young patients may reflect better perfusion of the outer retina. Therefore, when ischemia-hypoxia injury caused by CRVO occurs in young patients, there is greater resistance against the initial insult, resulting in a faster recovery, less retinal pigment epithelial and retinal capillary endothelial cell injury, a more intact blood–retinal barrier, and less release of factors such as VEGF. A study regarding the composition of the lamina cribrosa showed that the proportion of extracellular matrix components, such as collagen, elastin, sulfated glycosaminoglycans, and lipids, in the lamina cribrosa changes with age, resulting in reduced lamina cribrosa elasticity and mechanical compliance [54]. Thus, it can be speculated that the severity of obstruction may vary in patients of different ages. In the future, the difference in the degree of occlusion can be assessed by measuring the central retinal vein pressure in patients to clarify this point.
Interestingly, a retrospective study by Eah et al. showed that the incidence of paracentral acute middle maculopathy (PAMM) in young patients with CRVO is higher than that in elderly patients [18]. Rahimy’s research also confirms Eah et al.’s findings as his study revealed that 25 of 484 patients with CRVO were diagnosed with PAMM, with an average age of 51 years at diagnosis [55]. PAMM is an abnormal hyperreflective band lesion in optical coherence tomography (OCT) caused by ischemic injury at the level of the inner nuclear layer, which histologically corresponds to the middle and deep capillary plexus [56, 57]. The para-retinal fovea is a structure that has a high demand for oxygen. When CRVO occurs, the deep capillary plexus is initially affected, and ischemic changes occur. Therefore, PAMM can be regarded as an indicator of ischemic injury. It seems paradoxical that PAMM is more common in young patients as this population has a low incidence of ischemic CRVO. However, this paradox could be due to the following reasons: first, young patients have less retinal fluid leakage and relatively high venous pressure, and the unstable medial and deep capillary plexuses are more likely to be affected. Second, blood flow in the retinal vascular plexus is driven by the difference in the mean arterial and venous pressures; as the pulse pressure difference is lower in young patients with CRVO, the deep capillary plexus is more susceptible to hypoperfusion [58]. However, sampling error caused by the small sample size cannot be ignored, and the sample size needs to be further expanded in the future to prove this finding.
Young patients with CRVO are more likely to develop optic disc swelling [50]. Papilloedema was also reported to be a good predictor of visual prognosis in CRVO [1, 59]. The location of obstruction, inflammatory factors, and VEGF levels may play a role in the pathophysiology of swelling of the optic nerve head in young patients. Papillophlebitis is a rare condition that may present clinically like an incomplete CRVO and typically occurs in young, healthy females with acute, painless unilateral visual loss, optic disc edema, retinal vein engorgement, and varying amounts of intraretinal hemorrhage. The pathophysiology of papillophlebitis remains ill defined, and some authors have suggested that the condition stems from idiopathic “inflammation of the optic disc,” which then compresses the central retinal vein and causes secondary mechanical fundus findings of venous insufficiency and intraretinal hemorrhage [60]. The visual acuity in papillophlebitis patients is typically normal or near normal, and OCT may show a normal macula as opposed to the macular edema of CRVO. In contrast to CRVO, papillophlebitis is a self-limiting disease, usually with good prognosis, and benefits from treatment with corticosteroids; some authors consider papillophlebitis to be a diagnosis of exclusion [61].
Since the pathogenesis and risk factors are more diverse in young patients than in the elderly, young patients with local and systemic diseases will also show corresponding clinical manifestations. Optical coherence tomography angiography (OCTA), which produces high-resolution images of the retina and choroid at different levels, is an emerging imaging method and a novel technique for observing the retinal microvascular structure. OCTA can be used to further explore the differences in baseline manifestations, retinal microcirculation, and blood flow changes between young and elderly patients.
Differences in Treatment
There are no definitive treatment guidelines for young patients with CRVO. Although the treatment options for young and elderly patients are essentially similar, the treatment process, efficacy, and outcomes are not identical. Due to the differences in risk factors between young and elderly patients, local and systemic causes of CRVO should be explored, diagnosed, and treated promptly.
Generally, treatment for young patients with non-ischemic CRVO with preserved vision and without macular edema is watchful observation only with regular follow-ups. Macular edema with decreased visual acuity is an optimal indication for intravitreal injection of anti-VEGF drugs, such as ranibizumab, aflibercept, or bevacizumab, or intraocular injection of steroids, such as triamcinolone acetonide or sustained-release dexamethasone implantation. Many studies have shown that young patients require fewer intravitreal anti-VEGF injections than their older counterparts. Larsen et al. showed that CRVO patients with macular edema had a mean age of 65.5 years and received a mean of 8.1 ± 2.8 injections of anti-VEGF therapy injections (ranibizumab 0.5 mg) in the first 12 months of treatment [62]. Meanwhile, Koh et al. reported that young patients with CRVO had a mean age of 37.6 ± 8.5 years; 34% of eyes did not require anti-VEGF therapy injections, and 75% of the remaining eyes only required ≤ 3 injections [1]. Rothman’s study showed that the number of anti-VEGF injections was lower in young patients than in elderly patients during the same time period (3.0 ± 4.5 vs. 7.7 ± 5.5) [2]. Although young patients have a lower tolerance for vision loss, fewer anti-VEGF treatments are required in these patients to alleviate macular edema, possibly because the pathophysiology of macular edema in young patients with CRVO is different from that in elderly patients, the baseline clinical manifestations in young patients are milder, and young patients respond well to therapy compared with elderly patients.
In anti-VEGF-refractory cases, steroids can be used as a feasible option. Compared with patients ≥ 55 years, patients < 55 years have a longer median time to undergo a second dexamethasone implant, according to Lin’s research [63]. A possible explanation for this is that the solubility of dexamethasone in the vitreous may be affected by vitreous turbidity and thickening of the internal limiting membrane caused by aging, resulting in a lower efficacy in patients ≥ 55 years. Although some young patients with CRVO respond well to steroids, side effects, such as ocular hypertension and cataracts, must be considered [64]. Therefore, steroids should not completely replace anti-VEGF therapy in young patients. It has been shown that in patients with macular edema secondary to RVO, alternating intravitreal steroid and anti-VEGF injections has a better effect than anti-VEGF therapy alone [65]. There are no studies on intravitreal anti-VEGF therapy combined with steroid injections in young patients with CRVO. As combination therapy may reduce the frequency of injections, incidence of complications, and economic pressure on patients, as well as maximize visual acuity, further studies are warranted.
Retinal laser coagulation can be performed in cases where there are extensive non-perfused areas on the retina and retinal or iris neovascularization. Rothman et al. reported that young patients required fewer sessions of panretinal photocoagulation than elderly patients [1]. However, Ye et al. showed that there was no difference in the number of laser photocoagulation sessions between young and elderly patients with RVO [66], and Eah et al. also believed that the frequency of laser photocoagulation is not significantly affected by age [18]. Vitrectomy can be performed in cases where vitreous hemorrhage does not clear or tractional retinal detachment or proliferating epiretinal membrane occurs. In the study of Eah et al., all 49 young patients did not undergo vitrectomy, whereas 22 of 146 elderly patients underwent vitrectomy [18]. From Eah et al.’s results, it can be inferred that young patients are less likely to develop serious complications, such as vitreous hemorrhage and retinal detachment, than elderly patients.
Although thrombosis is an important cause of CRVO, the benefits of antiplatelet or anticoagulant therapy to improve visual outcomes remain controversial [67, 68]. On the other hand, these treatments may exacerbate retinal hemorrhaging. Therefore, larger randomized controlled studies are required to determine the role and efficacy of antiplatelets and anticoagulants in CRVO. Since the risk factors for CRVO in young patients are diverse, targeted therapy for different etiologies and individualized long-term monitoring are critical.
Differences in Prognosis
At present, most authors believe that young patients with CRVO have a better visual prognosis after treatment [2, 6, 10, 18, 50, 66]. In contrast, some studies have suggested poorer visual outcomes in young patients due to the lack of anti-VEGF therapy [69]. However, a study by Dewan et al. showed that the BCVA and CRT after anti-VEGF therapy between elderly and young patients at the final follow-up were not significantly different [70]. Eah et al. reported that compared with elderly patients, young patients had a better BCVA (logMAR 0.37 ± 0.57 vs. 0.93 ± 1.02), thinner CRT at the last follow-up (272.8 ± 111.5 vs. 420.5 ± 523.0 μm, P = 0.007), and SRF (0% vs.15.1%, P = 0.004) and CME (8.2% vs. 34.9%, P < 0.001) accounted for a lower proportion [18]. However, Rothman’s study did not show any difference in the mean SRF and CRT at the final follow-up between young and elderly patients, despite better BCVA in young patients [2]. Ye et al.’s study of OCTA-related parameters before and after receiving anti-VEGF therapy in young and elderly patients showed that compared with elderly patients, anti-VEGF therapy in young patients resulted in a better visual prognosis, a more significant improvement in the macular vascular density, and a decrease in the foveal avascular area in each layer of the retinal capillary plexus [66]. Therefore, retinal perfusion in young patients can improve after treatment, which is conducive to improving the visual prognosis. Koh et al. reported that the baseline BCVA, degree of baseline retinopathy (degree of retinal hemorrhage and venous tortuosity), degree of optic disc swelling, and presence or absence of diabetes were associated with the visual prognosis in young patients with CRVO, with BCVA being the best predictor of visual prognosis [1]. In the future, electroretinography can also be used to further analyze the relationship between retinal and optic nerve function and explore the prognosis of CRVO in young patients. Although the prognosis of CRVO in young patients is generally favorable, studies have reported that patients with combined central retinal artery and vein occlusion may be younger than the patients who had only CRVO or CRAO [71, 72]. In a previous study, mean age of the patients with combined central retinal artery and vein occlusion was 48.8 ± 14.1 years [72]. In these patients, artery occlusion could be secondary to CRVO, which increases the intraluminal pressure of the retinal capillary bed, and the pressure is transmitted to the retinal artery to decrease or even stop the blood flow. Optic disc swelling related to CRVO may further compress the retinal arteries, narrowing and possibly occluding them. Young patients with CRVO have relatively high venous pressure and are more likely to develop optic disc swelling, as mentioned above, which may be the mechanisms for combined central retinal artery and vein occlusion developing in young patients.
In summary, the etiology, pathogenesis, treatment, and prognosis between young and elderly patients with CRVO are different. Hence, the diagnosis and treatment of CRVO should depend on the patients’ characteristics and risk factors. Ideally, the etiology and severity of disease should be identified as early as possible for prompt initiation of targeted treatment, which can lead to a better visual prognosis. However, this review had a few limitations, mainly due to the presence of non-prospective studies and small sample sizes in some studies. Hence, future studies are warranted to further explore the mechanisms of CRVO in young patients.
References
Koh YY, Lai CC, Wu WC, Hwang YS, Chen KJ, Wang NK, Chen TL, Huang JC, Liu L, Yeung L. Baseline clinical features predict visual outcome in young patients with central retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2020;258(7):1367–77.
Rothman AL, Thomas AS, Khan K, Fekrat S. Central retinal vein occlusion in young individuals: a comparison of risk factors and clinical outcomes. Retina. 2019;39(10):1917–24.
Sinawat S, Bunyavee C, Ratanapakorn T, Sinawat S, Laovirojjanakul W, Yospaiboon Y. Systemic abnormalities associated with retinal vein occlusion in young patients. Clin Ophthalmol. 2017;11:441–7.
Wittström E. Central retinal vein occlusion in younger Swedish adults: case reports and review of the literature. Open Ophthalmol J. 2017;11:89–102.
Nalcaci S, Degirmenci C, Akkin C, Mentes J. Etiological factors in young patients with retinal vein occlusion. Pak J Med Sci. 2019;35(5):1397–401.
Battaglia Parodi M, Iacono P, Sacconi R, Parravano M, Varano M, Bandello F. Dexamethasone implant for macular edema secondary to central retinal vein occlusion in patients younger than 50 years. Retina. 2015;35(7):1381–6.
Chen TY, Uppuluri A, Zarbin MA, Bhagat N. Risk factors for central retinal vein occlusion in young adults. Eur J Ophthalmol. 2021;31(5):2546–55.
Liu Q, Lahey JM, Karlen R, Stewart JM. Laboratory evaluation of hypercoagulable states in patients with central retinal vein occlusion who are less than 56 years of age. Retina. 2018;38(6):1175–9.
Rogers S, McIntosh RL, Cheung N, Lim L, Wang JJ, Mitchell P, Kowalski JW, Nguyen H, Wong TY. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia, and Australia. Ophthalmology. 2010;117(2):313-319.e311.
Lindsell LB, Lai MM, Fine HF. Current concepts in managing retinal vein occlusion in young patients. Ophthalmic Surg Lasers Imaging Retina. 2015;46(7):695–701.
Fong AC, Schatz H. Central retinal vein occlusion in young adults. Surv Ophthalmol. 1993;37(6):393–417.
Vieira MJ, Campos A, do Carmo A, Arruda H, Martins J, Sousa JP. Thrombophilic risk factors for retinal vein occlusion. Sci Rep. 2019;9(1):18972.
Priluck IA, Robertson DM, Hollenhorst RW. Long-term follow-up of occlusion of the central retinal vein in young adults. Am J Ophthalmol. 1980;90(2):190–202.
Noma H, Yasuda K, Shimura M. Cytokines and pathogenesis of central retinal vein occlusion. J Clin Med. 2020;9(11):3457.
Lyle TK, Wybar K. Retinal vasculitis. Br J Ophthalmol. 1961;45(12):778–88.
Lonn LI, Hoyt WF. Papillophlebitis: a cause of protracted yet benign optic disc edema. Eye Ear Nose Throat Mon. 1966;45(10):62 passim.
Green WR, Chan CC, Hutchins GM, Terry JM. Central retinal vein occlusion: a prospective histopathologic study of 29 eyes in 28 cases. Retina. 1981;1(1):27–55.
Eah KS, Kim YN, Park YJ, Lee JY, Kim JG, Yoon YH, Kim YJ. Central retinal vein occlusion in young patients: clinical characteristics and prognostic factors. Retina. 2021;41(3):630–7.
Uhr JH, Thau A, Chung C, Zhang XC. Rare presentation of bilateral central retinal vein occlusion and leukemic retinopathy in a young adult diagnosed with T-cell acute lymphoblastic leukemia. Cureus. 2020;12(1): e6666.
Golesic EA, Sheidow TG. An otherwise healthy young man presents with bilateral CRVO as the first sign of hyperviscosity syndrome in the setting of new multiple myeloma. Retin Cases Brief Rep. 2015;9(1):38–40.
Yang V, Turner LD, Imrie F. Central retinal vein occlusion secondary to severe iron-deficiency anaemia resulting from a plant-based diet and menorrhagia: a case presentation. BMC Ophthalmol. 2020;20(1):112.
Huggins AB, Garg SJ, Sando RS, Jr. Central retinal vein occlusion in hereditary spherocytosis. Retin Cases Brief Rep. 2015.
Zuche M, Ladewig MS. Combined retinal vascular occlusion after overexertion in sport at a young age: an unusual case as interdisciplinary challenge. Ophthalmologe. 2021;118(9):944–7.
Rouhani B, Mandava N, Olson JL. Central retinal vein occlusion after intense exercise in healthy patients. Retin Cases Brief Rep. 2010;4(2):105–8.
Moisseiev E, Sagiv O, Lazar M. Intense exercise causing central retinal vein occlusion in a young patient: case report and review of the literature. Case Rep Ophthalmol. 2014;5(1):116–20.
Ahluwalia J, Rao S, Varma S, Gupta A, Bose S, Masih J, Das R, Kumar N, Naseem S, Sharma P, et al. Thrombophilic risk factors are uncommon in young patients with retinal vein occlusion. Retina. 2015;35(4):715–9.
Bremond-Gignac D, Daruich A, Gallet M, Menoud PA, Nowomiejska K, Rejdak R, Behar-Cohen F, Benkhalifa M, Copin H. Central retinal vein occlusion in otherwise healthy children and adolescents: association with multigenetic variants of thrombophilia. Retina. 2020;40(7):1339–43.
Bucciarelli P, Passamonti SM, Gianniello F, Artoni A, Martinelli I. Thrombophilic and cardiovascular risk factors for retinal vein occlusion. Eur J Intern Med. 2017;44:44–8.
Ammar MJ, Wu CM, Starr MR, Regillo CD. Central retinal vein occlusion after laparoscopic sleeve gastrectomy in an 18-year-Old female. Am J Ophthalmol Case Rep. 2021;23: 101165.
Liu Z, Pan X, Jiang W, Bi H. Central retinal venous occlusion in a child with hyperhomocysteinemia: a case report. Medicine (Baltimore). 2019;98(23): e15813.
Lahey JM, Tunç M, Kearney J, Modlinski B, Koo H, Johnson RN, Tanaka S. Laboratory evaluation of hypercoagulable states in patients with central retinal vein occlusion who are less than 56 years of age. Ophthalmology. 2002;109(1):126–31.
Kang SS, Rosenson RS. Analytic approaches for the treatment of hyperhomocysteinemia and its impact on vascular disease. Cardiovasc Drugs Ther. 2018;32(2):233–40.
Parodi MB, Di Crecchio L. Hyperhomocysteinemia in central retinal vein occlusion in young adults. Semin Ophthalmol. 2003;18(3):154–9.
Hernández JL, Sanlés I, Pérez-Montes R, Martínez-Taboada VM, Olmos JM, Salmón Z, Sierra I, Escalante E, Napal JJ. Antiphospholipid syndrome and antiphospholipid antibody profile in patients with retinal vein occlusion. Thromb Res. 2020;190:63–8.
Schockman S, Glueck CJ, Hutchins RK, Patel J, Shah P, Wang P. Diagnostic ramifications of ocular vascular occlusion as a first thrombotic event associated with factor V Leiden and prothrombin gene heterozygosity. Clin Ophthalmol. 2015;9:591–600.
Masood I. The platelet glycoprotein Ia/IIa gene polymorphism C807T/C873A: a novel risk factor for retinal vein occlusion. Eye (Lond). 2004;18(10):1013.
Bertram B, Remky A, Arend O, Wolf S, Reim M. Protein C, protein S, and antithrombin III in acute ocular occlusive diseases. Ger J Ophthalmol. 1995;4(6):332–5.
Rehak M, Rehak J, Müller M, Faude S, Faude F, Siegemund A, Krcova V, Slavik L, Hasenclever D, Scholz M, et al. The prevalence of activated protein C (APC) resistance and factor V Leiden is significantly higher in patients with retinal vein occlusion without general risk factors. Case-control study and meta-analysis. Thromb Haemost. 2008;99(5):925–9.
Kuhli-Hattenbach C, Hellstern P, Nägler DK, Kohnen T, Hattenbach LO. Prothrombin polymorphism A19911G, factor V HR2 haplotype A4070G, and plasminogen activator-inhibitor-1 polymorphism 4G/5G and the risk of retinal vein occlusion. Ophthalmic Genet. 2017;38(5):413–7.
Yahalomi T, Pikkel J, Arnon R, Pessach Y. Central retinal vein occlusion in a young healthy COVID-19 patient: a case report. Am J Ophthalmol Case Rep. 2020;20: 100992.
Ashkenazy N, Patel NA, Sridhar J, Yannuzzi NA, Belin PJ, Kaplan R, Kothari N, Benitez Bajandas GA, Kohly RP, Roizenblatt R, et al. Hemi- and central retinal vein occlusion associated with coronavirus disease 2019 infection in young patients without known risk factors. Ophthalmol Retina 2022.
Weiss MY, Kuriyan AE. Acute monocular vision loss in a young adult. JAMA Ophthalmol. 2018;136(3):297–8.
Stowe GC 3rd, Zakov ZN, Albert DM. Central retinal vascular occlusion associated with oral contraceptives. Am J Ophthalmol. 1978;86(6):798–801.
Aggarwal RS, Mishra VV, Aggarwal SV. Oral contraceptive pills: a risk factor for retinal vascular occlusion in in-vitro fertilization patients. J Hum Reprod Sci. 2013;6(1):79–81.
Oglodek EA, Just MJ, Grzesinska AD, Araszkiewicz A, Szromek AR. The impact of antipsychotics as a risk factor for thromboembolism. Pharmacol Rep. 2018;70(3):533–9.
Taki K, Kida T, Fukumoto M, Sato T, Oku H, Ikeda T. Central retinal vein occlusion in 2 patients using antipsychotic drugs. Case Rep Ophthalmol. 2017;8(2):410–5.
Yin X, Li J, Zhang B, Lu P. Association of glaucoma with risk of retinal vein occlusion: a meta-analysis. Acta Ophthalmol. 2019;97(7):652–9.
Xu K, Wu L, Ma Z, Liu Y, Qian F. Primary angle closure and primary angle closure glaucoma in retinal vein occlusion. Acta Ophthalmol. 2019;97(3):e364–72.
Kavoussi SC, Kempton JE, Huang JJ. Central retinal vein occlusion resulting from anomalous retinal vascular anatomy in a 24-year-old man. Clin Ophthalmol. 2015;9:885–7.
Walters RF, Spalton DJ. Central retinal vein occlusion in people aged 40 years or less: a review of 17 patients. Br J Ophthalmol. 1990;74(1):30–5.
Hayreh SS, Klugman MR, Beri M, Kimura AE, Podhajsky P. Differentiation of ischemic from non-ischemic central retinal vein occlusion during the early acute phase. Graefes Arch Clin Exp Ophthalmol. 1990;228(3):201–17.
Wei Y, Jiang H, Shi Y, Qu D, Gregori G, Zheng F, Rundek T, Wang J. Age-related alterations in the retinal microvasculature, microcirculation, and microstructure. Investig Ophthalmol Vis Sci. 2017;58(9):3804–17.
Maruko I, Arakawa H, Koizumi H, Izumi R, Sunagawa H, Iida T. Age-dependent morphologic alterations in the outer retinal and choroidal thicknesses using swept source optical coherence tomography. PLoS ONE. 2016;11(7): e0159439.
Albon J, Karwatowski WS, Easty DL, Sims TJ, Duance VC. Age related changes in the non-collagenous components of the extracellular matrix of the human lamina cribrosa. Br J Ophthalmol. 2000;84(3):311–7.
Rahimy E, Sarraf D, Dollin ML, Pitcher JD, Ho AC. Paracentral acute middle maculopathy in nonischemic central retinal vein occlusion. Am J Ophthalmol. 2014;158(2):372-380.e371.
Scharf J, Freund KB, Sadda S, Sarraf D. Paracentral acute middle maculopathy and the organization of the retinal capillary plexuses. Prog Retin Eye Res. 2021;81: 100884.
Sarraf D, Rahimy E, Fawzi AA, Sohn E, Barbazetto I, Zacks DN, Mittra RA, Klancnik JM Jr, Mrejen S, Goldberg NR, et al. Paracentral acute middle maculopathy: a new variant of acute macular neuroretinopathy associated with retinal capillary ischemia. JAMA Ophthalmol. 2013;131(10):1275–87.
Browning DJ. Patchy ischemic retinal whitening in acute central retinal vein occlusion. Ophthalmology. 2002;109(11):2154–9.
Beaumont PE, Kang HK. Pattern of vascular nonperfusion in retinal venous occlusions occurring within the optic nerve with and without optic nerve head swelling. Arch Ophthalmol. 2000;118(10):1357–63.
Insausti-Garcia A, Reche-Sainz JA, Ruiz-Arranz C, Lopez Vazquez A, Ferro-Osuna M. Papillophlebitis in a COVID-19 patient: Inflammation and hypercoagulable state. Eur J Ophthalmol. 2022;32(1):NP168–72.
Oh KT, Oh DM, Hayreh SS. Optic disc vasculitis. Graefes Arch Clin Exp Ophthalmol. 2000;238(8):647–58.
Larsen M, Waldstein SM, Boscia F, Gerding H, Monés J, Tadayoni R, Priglinger S, Wenzel A, Barnes E, Pilz S, et al. Individualized ranibizumab regimen driven by stabilization criteria for central retinal vein occlusion: twelve-month results of the CRYSTAL study. Ophthalmology. 2016;123(5):1101–11.
Lin CJ, Chen HS, Su CW, Tien PT, Lin JM, Chen WL, Kuo CY, Lai CT, Tsai YY. The effect of age and initial central retinal thickness on earlier need of repeat ozurdex treatment for macular edema due to retinal vein occlusion: a retrospective case series. J Ocul Pharmacol Ther. 2017;33(10):763–72.
Rezkallah A, Mathis T, Abukhashabah A, Voirin N, Malclès A, Agard É, Lereuil T, Denis P, Dot C, Kodjikian L: Long-term incidence and risk factors of ocular hypertension following dexamethasone-implant injections. The SAFODEX-2 study. Retina. 2020.
Bae YH, Kim SM, Kim JY, Bae SH, Kim H, Ma DJ. Effect of alternate treatment with intravitreal corticosteroid and anti-VEGF for macular edema secondary to retinal vein occlusion. J Ophthalmol. 2021;2021:5948113.
Ye P, Zhu T, Zheng F, Zhou M, Fang X, Yao K. Microvascular comparison in younger and older patients with retinal vein occlusion analyzed by OCT angiography. BMC Ophthalmol. 2021;21(1):161.
Hayreh SS, Podhajsky PA, Zimmerman MB. Central and hemicentral retinal vein occlusion: role of anti-platelet aggregation agents and anticoagulants. Ophthalmology. 2011;118(8):1603–11.
Ageno W, Cattaneo R, Manfredi E, Chelazzi P, Venco L, Ghirarduzzi A, Cimino L, Filippucci E, Ricci AL, Romanelli D, et al. Parnaparin versus aspirin in the treatment of retinal vein occlusion. A randomized, double blind, controlled study. Thromb Res. 2010;125(2):137–41.
Gupta A, Agarwal A, Bansal RK, Agarwal A, Chugh KS. Ischaemic central retinal vein occlusion in the young. Eye (Lond). 1993;7(Pt 1):138–42.
Dewan KS, Hentati F, Greenlee TE, Conti TF, Chen AX, Hom GL, Singh RP. Age-related differences in presentation and outcomes of anti-VEGF treatment of retinal vein occlusion. Can J Ophthalmol. 2021;56(2):96–104.
Vallee JN, Paques M, Aymard A, Massin P, Santiago PY, Adeleine P, Gaudric A, Merland JJ. Combined central retinal arterial and venous obstruction: emergency ophthalmic arterial fibrinolysis. Radiology. 2002;223(2):351–9.
Wang H, Chang Y, Zhang F, Yang R, Yan S, Dong J, Zhang M, Peng S. Clinical features of combined central retinal artery and vein occlusion. J Ophthalmol. 2019;2019:7202731.
Acknowledgements
Funding
Liaoning Science and Technology Project (no. 2013225303, H.Z.) supported this work. However, the funder played no role in the study design, data assembly or analysis, publishing decision, or manuscript preparation. The journal’s Rapid Service Fees were funded by the authors.
Author Contributions
Han Zhang, Xiao-Tong Zhang and Yi-Fan Zhong designed the study and prepared the manuscript. Yan-Qi Xue, Si-Qi Li, Bing-Yu Wang, Gui-Qi Zhang and Iko Hidasa collected the data. All authors have reviewed the manuscript.
Disclosures
Xiao-Tong Zhang, Yi-Fan Zhong, Yan-Qi Xue, Si-Qi Li, Bing-Yu Wang, Gui-Qi Zhang, Iko Hidasa and Han Zhang all confirm that they have no competing interests to declare.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
All data generated or analyzed during this study are included in this published article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zhang, XT., Zhong, YF., Xue, YQ. et al. Clinical Features of Central Retinal Vein Occlusion in Young Patients. Ophthalmol Ther 11, 1409–1422 (2022). https://doi.org/10.1007/s40123-022-00534-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00534-7