Abstract
We report localized opacification of a sclera-fixated Akreos® hydrophilic acrylic intraocular lens after successful repair of rhegmatogenous retinal detachment with silicone oil tamponade in a nondiabetic patient. No intraoperative lens opacification during air–fluid exchange or lens dislocation was encountered. Granular opacities within the optic were noted at 5 months after surgery, and did not relent to scrubbing with a vitrector during oil removal. Akreos lens opacification under silicone oil is not well documented in the literature. Surgeons must be aware of this potential complication, which is known to occur with various types of hydrophilic acrylic lenses after exposure to air or gas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Four-point scleral fixation of a hydrophilic acrylic IOL, Akreos® AO60 (Bausch & Lomb, Bridgewater, NJ, USA) using Gore-Tex (polytetrafluoroethylene) sutures has recently gained popularity in eyes without zonular support [1]. However, reports of late opacification of various hydrophilic acrylic lenses, including Akreos IOLs, are concerning. Opacification has been reported to occur due to UV blocker aging [2], calcium deposition [3,4,5], silicon (Si) and silicone (SiO) deposition from IOL packaging [6], after implantation in diabetics [5, 7], due to intracameral injection of tissue plasminogen activator (tPA) [8], and after instillation of air [9], SF6, or C3F8 gas in vitreoretinal surgery [10] or Descemet stripping keratoplasties [4, 9].
Opacification of an Akreos IOL under silicone oil is a less well-known phenomenon, with only three cases published in the literature so far, two in diabetics. Here we report our experience with the use of silicone oil in a 70-year-old nondiabetic patient presenting with rhegmatogenous retinal detachment after scleral fixation of an Akreos AO60 lens.
Case Report
A 70-year-old male was referred to the Miami Veterans Affairs Hospital due to recurrent episodes of anterior chamber inflammation, hyphema, and vitreous hemorrhage in his left eye associated with endocapsular one-piece PCIOL dislocation. Twenty-eight years before presentation, his left eye underwent a scleral buckle-vitrectomy-gas procedure complicated by infectious scleritis, necessitating scleral buckle removal and later cataract extraction with one-piece acrylic PCIOL placement. Previously he also received radial keratotomy in both eyes.
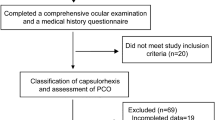
On presentation, best-corrected visual acuity was 20/20 in the right and 20/70 in the left eye. Left eye examination revealed radial keratotomy scars, trace anterior chamber cells, atrophic iris, an inferiorly dislocated PCIOL-capsular bag complex (Fig. 1), vitreous hemorrhage, and an attached retina with peripheral laser-induced chorioretinal scarring.
We performed an uncomplicated 23-gauge pars plana vitrectomy, explanted the dislocated bag-PCIOL complex through a scleral tunnel, and fixated the Akreos lens with CV-8 Gore-Tex sutures, as previously described [1, 11]. No retinal breaks were noted on scleral indentation.
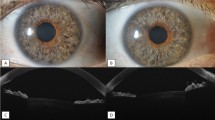
Eleven days later the patient presented with a total retinal detachment with grade B proliferative vitreoretinopathy due to multiple retinal breaks. Intraocular pressure (IOP) was 10, and white blood cells (WBC) in the anterior chamber (AC) were graded 1+. No hyphema or vitreous hemorrhage was present. A pars plana vitrectomy with a 5000 centistoke silicone oil tamponade was performed. One month later, the retina was attached with a well-centered Akreos lens and a moderate-size silicone oil droplet in the AC. The IOP was 12 and rare pigment and WBCs without a hyphema were present in the AC. The lens appeared clear. At 4.5 months after retinal detachment repair, whitish granular opacification was noted in the lens optic (Fig. 2). The silicone oil droplet in the AC was stable in size, IOP was 13, rare pigment was present in the AC, and the retina was well attached. Immediate silicone oil removal was scheduled. During the procedure, we were unable to scrape the opacities with the vitrector by scrubbing the anterior or the posterior IOL surface. One week after oil removal, the uncorrected VA was 20/150, trace WBCs were seen in the AC, the retina was attached, and the lens opacities appeared stable (Fig. 3). These opacities have not enlarged since silicone oil removal and have been stable for at least 3 months postoperatively.
Our patient was informed of the delicate nature of his ocular condition and gave his consent to publish this report. The case report complies with the guidelines for human studies and was conducted ethically in accordance with the World Medical Association Declaration of Helsinki.
Discussion
The surgical technique of Akreos AO60 hydrophilic lens scleral fixation with off-label Gore-Tex (polytetrafluoroethylene) sutures has recently become popular in the vitreoretinal community for eyes without sufficient zonular support [1]. Centration and surgical outcomes have been favorable [11]. Unfortunately, hydrophilic acrylic lenses are prone to opacification. Various hydrophilic acrylic IOLs have been reported to develop calcium deposition on the surface and subsurface in diabetics, in association with intracameral injection of tissue plasminogen activator (tPA), and after exposure to intracameral or intravitreal air, SF6, or C3F8 gas [4, 8, 10, 12, 13].
A recent report of two cases documented Akreos lens opacification at 6 weeks and 3 months postoperatively after intravitreal 20% SF6 gas instillation during lensectomy and Akreos lens scleral fixation in nondiabetic patients with ectopia lentis [10]. In the second patient, the opacification increased between month 3 and month 5 and was associated with symptomatic photophobia. This is the first report of sclera-fixated Akreos AO60 IOL opacification in the presence of a gas tamponade without a capsule present. Dhital et al. reported a case of Rayner (Hove, UK) C-flex 570C hydrophilic lens opacification after vitrectomy with SF6 gas injection for the repair of a traumatic retinal detachment [13]. Several authors have documented calcium and phosphate deposition within hydrophilic acrylic lenses, including “in-the-bag” Akreos AO IOLs, after straightforward phacoemulsification or vitrectomy without any tamponade in diabetic patients [5, 7, 14].
However, the interaction of hydrophilic IOLs with silicone oil is not well documented. Only three reports (two with an Akreos AO lens) were found in the literature at the time we performed a literature search while planning surgical repair for our patient. In 2010 Lee et al. reported a case of calcium deposits on the surface of an explanted C-flex 570C hydrophilic lens, which developed 6 months after silicone oil removal in a 24-year-old myopic female who had oil in the eye for 3 months after retinal detachment repair [12]. In 2010, Park et al. reported two cases of Akreos AO MI60 opacification in diabetic patients who had silicone oil placed for tractional retinal detachment repair [5]. Explanted lenses were shown to contain calcium and phosphate deposits within the anterior surface.
Since our patient was a nondiabetic and there were no other reports of Akreos opacification under silicone oil, we chose to utilize silicone oil rather than gas during the surgery. Unfortunately, at 5 months postoperatively we noted an obvious patch of granular whitish opacities within the lens optic (Fig. 2). These opacities did not enlarge after silicone oil removal and remained stable in appearance for at least 3 months postoperatively.
Two months after we treated our patient, Rubin and Baker published their case of a nondiabetic 80-year-old male who had a clinical course very similar to that of our 70-year-old nondiabetic patient [15]. Both patients underwent Akreos lens suturing to treat a single-piece IOL subluxation, and both developed a retinal detachment within 2 weeks of implantation (9 days in Rubin’s case report). Thus, metabolic changes in the anterior chamber and blood–aqueous barrier breakdown after a recent intraocular surgery may have led to the development of opacification.
Conclusions
Surgeons need to be aware of the possibility of Akreos IOL opacification with silicone oil tamponade. As more cases of Akreos opacification are published, our understanding of patient factors and clinical scenarios leading to the development of deposits will improve. It remains to be determined whether silicone oil limits the risk of developing lens opacification in the short and long term compared to the incidence or severity of this complication with intraocular gas.
References
Khan MA, Gupta OP, Smith RG, Ayres BD, Raber IM, Bailey RS, et al. Scleral fixation of intraocular lenses using Gore-Tex suture: clinical outcomes and safety profile. Br J Ophthalmol. 2016;100(5):638–43.
Frohn A, Dick HB, Augustin AJ, Grus FH. Late opacification of the foldable hydrophilic acrylic lens SC60B-OUV. Ophthalmology. 2001;108(11):1999–2004.
Habib NE, Freegard TJ, Gock G, Newman PL, Moate RM. Late surface opacification of Hydroview intraocular lenses. Eye (Lond). 2002;16(1):69–74.
Werner L, Wilbanks G, Nieuwendaal CP, Dhital A, Waite A, Schmidinger G, et al. Localized opacification of hydrophilic acrylic intraocular lenses after procedures using intracameral injection of air or gas. J Cataract Refract Surg. 2015;41(1):199–207.
Park DI, Ha SW, Park SB, Lew H. Hydrophilic acrylic intraocular lens optic opacification in a diabetic patient. Jpn J Ophthalmol. 2011;55(6):595–9.
Werner L, Hunter B, Stevens S, Chew JL, Mamalis N. Role of silicon contamination on calcification of hydrophilic acrylic intraocular lenses. Am J Ophthalmol. 2006;141(1):35–43.
Cao D, Zhang H, Yang C, Zhang L. Akreos Adapt AO Intraocular lens opacification after vitrectomy in a diabetic patient: a case report and review of the literature. BMC Ophthalmol. 2016;16:82.
Fung SS, Sykakis E, Islam NM, Zambarakji HJ, Khoramnia R, Auffarth GU, et al. Intraocular lens opacification following intracameral injection of recombinant tissue plasminogen activator to treat inflammatory membranes after cataract surgery. J Ophthalmol. 2015;2015:975075.
Norouzpour A, Zarei-Ghanavati S. Hydrophilic acrylic intraocular lens opacification after descemet stripping automated endothelial keratoplasty. J Ophthalmic Vis Res. 2016;11(2):225–7.
Kalevar A, Dollin M, Gupta RR. Opacification of scleral-sutured Akreos Ao60 intraocular lens after vitrectomy with gas tamponade: case series. Retin Cases Brief Rep. 2017. https://doi.org/10.1097/ICB.0000000000000634.
Khan MA, Samara WA, Gerstenblith AT, Chiang A, Mehta S, Garg SJ, et al. Combined pars plana vitrectomy and scleral fixation of an intraocular lens using gore-tex suture: one-year outcomes. Retina. 2018;38(7):1377–84.
Lee SJ, Choi JH, Sun HJ, Choi KS, Jung GY. Surface calcification of hydrophilic acrylic intraocular lens related to inflammatory membrane formation after combined vitrectomy and cataract surgery. J Cataract Refract Surg. 2010;36(4):676–81.
Dhital A, Spalton DJ, Goyal S, Werner L. Calcification in hydrophilic intraocular lenses associated with injection of intraocular gas (53(6):1154-60). Am J Ophthalmol. 2012;153(6):1154–1160 e1151.
Pandey SK, Werner L, Apple DJ, Kaskaloglu M. Hydrophilic acrylic intraocular lens optic and haptics opacification in a diabetic patient: bilateral case report and clinicopathologic correlation. Ophthalmology. 2002;109(11):2042–51.
Rubin U, Baker CF. Akreos lens opacification under silicone oil. Can J Ophthalmol. 2018;53(5):e188–90.
Acknowledgements
Funding
No funding or sponsorship was received for this study or the publication of this article. The article processing charges were funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship contributions
Drs. Gregori and Echegaray both collected the clinical information, drafted the manuscript, approved the final version of the manuscript, reviewed the references, and both take responsibility for the submission. Dr. Flynn participated in the interpretation of data, critically revised the manuscript, reviewed the references, approved the final version of the paper, and takes responsibility for the submission.
Disclosures
Ninel Z. Gregori, Jose J. Echegaray, and Harry W. Flynn Jr have nothing to disclose.
Compliance with ethics guidelines
This case report complies with the guidelines for human studies and was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The patient was informed and has given his written informed consent to publish his case (including publication of lens images). No photographs by which the patient may be identified are included in this submission.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.7880870.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Gregori, N.Z., Echegaray, J.J. & Flynn, H.W. Opacification of Akreos Hydrophilic Acrylic Lens After Retinal Detachment Repair with Silicone Oil Tamponade: A Case Report. Ophthalmol Ther 8, 341–345 (2019). https://doi.org/10.1007/s40123-019-0183-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-019-0183-9