Abstract
Post-operative endophthalmitis (POE) following cataract surgery is an uncommon, vision-threatening complication that has been reported to occur at rates of between approximately 0.03% and 0.2%. Prompt diagnosis and treatment of endophthalmitis is critical for minimizing vision loss, but most recent efforts have focused on the prophylactic administration of antibiotics to prevent the development of endophthalmitis. Surgeons from around the world have different topical and intracameral antibiotic usage patterns to prevent endophthalmitis, and to date no general consensus regarding best practice has emerged. Several studies have reported on the routine use of intracameral cefuroxime, moxifloxacin, and vancomycin, including a single randomized clinical trial by the European Society of Cataract and Refractive Surgery (ESCRS) in 2007. These studies have notable shortcomings, but many authors suggest that intracameral cefuroxime together with topical antibiotics probably decreases the risk of endophthalmitis. However, the deleterious effects of routine prophylactic antibiotics, which include toxicity, cost, and increasing antimicrobial resistance, among others, are noteworthy. In contrast, aseptic technique with pre-operative instillation of povidone-iodine remains the only technique supported by level I evidence to reduce the incidence of endophthalmitis. Although the routine use of intracameral antibiotics continues to increase throughout the world, data from multicenter, randomized, prospective trials is needed to provide better guidance regarding the prophylactic use of antibiotics.
Similar content being viewed by others
Introduction
Cataract extraction with intraocular lens implantation is the most frequently performed surgery throughout the world, with more than 10 million cases completed each year. Most patients experience uncomplicated post-operative courses and their visual acuities usually improve. With advances in surgical instrumentation, techniques, and training, the incidences of significant post-operative problems are, fortunately, very low.
One of the most feared complications of cataract surgery, however, remains endophthalmitis. Post-operative endophthalmitis can be defined as “severe inflammation involving both the anterior and posterior segments of the eye after intraocular surgery” [1]. It usually follows inoculation of the eye by bacteria, with fungi and parasites being less commonly involved, and has been reported to occur at rates of between 0.03% and 0.2% [2]. Endophthalmitis can have devastating effects on vision, with final acuities ranging from normal to complete loss in the affected eye. Unfortunately, the prognosis is frequently poor, and it depends on several factors, including the causative organism and time to diagnosis.
Incidence rates of post-operative endophthalmitis (POE) have fluctuated in conjunction with changes in surgical techniques, but they have generally been stable over the past two decades. Some authors have opined that endophthalmitis should be a “never event” [3], but we still know too little about the associated risk factors to state that we can completely eradicate POE [4, 5]. Nonetheless, physicians continuously attempt to decrease the incidence of endophthalmitis by applying innovative aseptic and surgical techniques. Most surgeons believe that endophthalmitis rates can continue to be improved, even beyond a baseline endophthalmitis rate of 0.07%, which is significantly lower than any nation’s reported average to date [6].
Here we describe current attempts to reduce the incidence of post-cataract extraction endophthalmitis and provide our own recommendations that are based upon a review of the literature and our own institution’s aseptic techniques. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Evolution of cataract surgery
Cataract extraction dates back to the 17th century B.C. at which time the “couching” technique was used to posteriorly sublux the cataractous lens into the vitreous cavity with a blunt instrument [7]. Despite the widespread adoption of modern surgical techniques, couching continues to be used in some parts of the world that have limited provision of healthcare. Not surprisingly, blindness rates after couching may be as high as 70% because of numerous complications, including high rates of infection [8,9,10]. Reported endophthalmitis rates following couching have ranged from 12.5% to 22% [10,11,12], but accurate rates are difficult to verify given the relative rarity of couching.
Extracapsular cataract extraction through a corneal incision was first performed in 1787 by Jacques Daviel after attempts to dislocate the lens during a couching procedure were unsuccessful. He presented this method to the Royal Academy of Surgery, after which his technique gained popularity and became the new standard in place of couching [13]. Because antisepsis was not practiced at that time and sutures were not available until 1867, the corneal incision remained open and represented a significant risk of wound dehiscence and infection [14]. Patients recovered in a dark room for approximately 1 week during which the eyes were bathed with mixtures of water and wine and bandaged with a cotton dressing [15].
Phacoemulsification was introduced in 1967 by Charles Kelman, after he took cues from his dentist’s ultrasound probes. During subsequent years, the surgical incisions became increasingly smaller, varying from 3 mm to as small as 1 mm, and together with improved instrumentation, the small incisions resulted in markedly reduced inflammation after extraction of the lens [16]. Hospital stays were shortened, and eventually the surgery became an outpatient procedure. Initially, the introduction of phacoemulsification and sutureless clear corneal incisions led to an increase in endophthalmitis rates, from 0.074% to 0.087% up to 0.0189–0.265%, which was thought to be due to increased microbial access to the anterior chamber after completion of the surgery [17]. The clear corneal incision, however, remains the favored approach for cataract extraction (compared to the scleral tunnel incision) since it has led to faster visual recovery, shorter surgical times, and less manipulation of the globe. In previous surveys, clear corneal incisions were preferred by 75% of American Society of Cataract and Refractive Surgery (ASCRS) members [18, 19].
Femtosecond laser-assisted cataract surgery (FLACS) was introduced in 2012 after the laser had originally been developed for refractive surgery (laser in situ keratomileusis [LASIK] in 2001). The laser automates the performance of incisions and softens the lens nucleus, all of which may improve surgical precision, accuracy, and reproducibility. One study reported significantly better optical quality and internal aberrations compared to phacoemulsification, but without significant differences in refractive errors or best corrected distance visual activity [20]. Whether the FLACS incisions result in lower rates of endophthalmitis is still under investigation [21].
Pre-Operative Care
The antiseptic properties of iodine were first noted in 1811, although its high toxicity profile and low solubility originally limited its ophthalmic application. Argyrol, a compound of mild silver-containing proteins, was the dominant ophthalmic antiseptic from its commercial introduction in 1901 until it was demonstrated to have minimal bactericidal effect in a 1983 study, after which its use was gradually abandoned [22]. The following year, a study validated the effectiveness of the povidone-iodine solution, which had originally been introduced in the 1950s as a pre-operative preparation. This study found that povidone-iodine decreased the number of bacterial colonies on the surface of the eye by 91% and the number of species by 50% [23]. The benefits of povidone-iodine solutions include rapid bactericidal action, low toxicity, higher solubility compared to iodine alone, and lack of bacterial resistance [24]. The efficacy of 5–10% povidone-iodine applied to the cornea, conjunctiva, and eyelids for at least 3 min prior to surgery is supported by level I evidence, and this procedure is now considered standard of care [5, 25]. The pre-operative preparation of the eye also includes the placement of a sterile eyelid speculum and draping of the patient with isolation of the eyelids and eyelashes. Trimming of the eyelashes pre-operatively has no demonstrable effect on preventing endophthalmitis [26].
The pre-operative administration of topical antibiotics is relatively common—90% of responders to the 2014 ASCRS survey reported routinely using antibiotics peri-operatively [27]. There is no universally agreed upon regimen, and the most common medication according to the ASCRS survey was a topical fourth-generation fluoroquinolone, such as moxifloxacin or gatifloxacin. Worldwide, fourth-generation fluoroquinolones are the most commonly used topical antibiotics [28] while the less commonly used antibiotics include the early-generation fluoroquinolones, trimethoprim-polymyxin B, gentamicin, and tobramycin. Although aminoglycosides are inexpensive and effective against Staphylococcus spp., they do not penetrate well into the anterior chamber and thus compare poorly to other choices [6]. Evidence that routine use of topical antibiotics may select for resistant bacteria calls into question the wisdom of routine antibiotic use [25, 29]. Up to 90% of cataract surgery patients, particularly those inexperienced with the use of eye drops, demonstrate poor instillation technique, including failure to wash hands, contamination of bottle tips, frequent missing of the eye, difficulty in extending their necks, and use of an incorrect number of drops [30]. Various instillation aids have been developed, and these may ameliorate at least a few of the difficulties [31]. Another purported reason for nonadherence is “drop phobia,” the reluctance to instill drops onto the eye [32]. A 2017 systematic review found “moderate-certainty evidence” that using antibiotic eye drops in addition to antibiotic injections probably lowers the incidence of endophthalmitis compared with using either injections or eye drops alone [33].
Intra-operative Care
Injecting intracameral antibiotics at the completion of cataract surgery has become an increasingly popular topic of discussion since the European Society of Cataract and Refractory Surgeons (ESCRS) conducted a landmark randomized clinical trial that evaluated the routine use of topical and intracameral antibiotics for cataract surgery in 2005. Their study included 13,698 patients from 24 European centers. Prophylactic intracameral injections of cefuroxime was found to reduce the incidence of POE by nearly fivefold (0.33% vs. 0.07%). Critics of this study have cited an unusually high rate of endophthalmitis in the control group at 0.33% (the high end of the incidence range often reported in prior studies is 0.2%), the use of multiple surgical techniques, the narrow spectrum of cefuroxime activity (which is not ideal for members of genus Staphylococcus), the reconstitution of the antibiotic from powder, and that the study was stopped prematurely [34].
Following publication of the ESCRS trial, many other studies from 2014 onwards, predominantly retrospective in design, also supported the use of intracameral antibiotics. One of the problems common to most of these retrospective studies is that they do not account for improvements in asepsis and operative techniques during the same study periods, which may account for the decline in rates of endophthalmitis. A less obvious limitation of database studies includes inaccuracies in diagnosis and procedure coding, particularly with the use of different International Classification of Disease, Tenth Edition (ICD-10) codes, such as the H44.0 codes for “purulent endophthalmitis” and H44.1 codes for “other endophthalmitis.” A relatively minor inaccuracy in coding may inadvertently exclude many cases from the population being studied [35, 36]. In Australia, patients with POE were treated as outpatients without a diagnosis entered into the database being studied [37]. It is therefore important to remember that big data is good at detecting associations, but it cannot tell us which associations are meaningful. Big data can work well as an adjunct to scientific inquiry, but it rarely succeeds as a wholesale replacement [38].
Around the world, the general trend has been toward increasing routine use of intracameral antibiotics. According to the 2014 ASCRS survey, approximately 47% of U.S. cataract surgeons currently use or planned to adopt the routine use of intracameral prophylaxis, which is up from 30% in 2007. Of those responding to the survey, 69% answered that they would use an intracameral antibiotic if it were commercially available, reasonably priced, and prepackaged [28]. In Japan, where one million cataract surgeries are performed each year, there was an increase in intracameral prophylaxis from < 2% to approximately 12% by 2013. The use of the intracameral route in Canada has been reported to be 42.1%, and in Australia intracameral use exceeds 80%. Intracameral prophylaxis is recommended by various national societies, including those in Italy, Turkey, Spain, Portugal, Hungary, and Finland. It is considered unethical to withhold treatment with the intracameral antibiotic cefuroxime in Sweden unless the patient has a known cephalosporin allergy [39].
The most common organisms associated with POE are Gram-positive bacteria, and the single most common offender is Staphylococcus epidermidis, a Gram-positive, coagulase-negative bacterium that is usually susceptible to the three most commonly used intracameral antibiotics. A smaller, but still significant, percentage of POE cases are due to other Gram-positive bacteria, such as Staphylococcus aureus and Streptococcus spp., Gram-negative bacteria, such as Pseudomonas aeruginosa, and, less commonly, fungi.
The most commonly used intracameral antibiotics are cefuroxime, moxifloxacin, and vancomycin. The medical risks associated with routine intracameral antibiotic prophylaxis include anaphylactic reactions, overdoses, introduction of contaminants, acquired bacterial resistance, and other adverse events specific to each antibiotic.
Cefuroxime is a second-generation cephalosporin that was first introduced for systemic use in 1987. It halts the synthesis of the peptidoglycan layer of the bacterial cell wall, thereby disrupting cell-wall integrity. Its action is time dependent, which means it possesses bactericidal activity as long as the drug concentration is greater than the minimum inhibitory concentration. Cefuroxime is the only one of these three commonly used intracameral antibiotics that has been studied in a prospective, randomized, controlled trial (RCT), and it has been discussed in the greatest number of observational studies. Retrospective studies from Canada, France, South Africa, and Sweden, among other countries, have found significant decreases in the rate of POE with the use of intracameral cefuroxime. In Spain, reductions in endophthalmitis were as high as tenfold with intracameral cefazolin, another cephalosporin [40,41,42,43,44,45,46] A tertiary center in Hong Kong reduced the incidence of endophthalmitis to 0% with the use of intracameral cefuroxime that had been compounded by the hospital pharmacy [47].
During the ESCRS trial, cefuroxime was reconstituted from powder, but a commercial preparation (Aprokam®, Thea Pharmaceuticals, Newcastle Under Lyme, UK) is now available in Europe. However, there is no Food and Drug Administration (FDA)-approved product available for use in the USA, and the substantial barriers to approval make it unlikely that a product will be approved soon [76]. The off-label use of intracameral cefuroxime requires that a nurse of other professional reconstitute the drug from a vial in the operating room or a reliable compounding pharmacy must be employed to decrease variability in dosage and prevent microbial contamination. Both strategies have been employed, particularly in parts of the world where cefuroxime that has been specifically prepared and approved for intracameral use is not available. Various methods of cefuroxime preparation have been described, many of which require multiple steps, including a two-step method to obtain a final concentration of 1 mg/0.1 mL [48]. Compounding the drug introduces a risk of infection, particularly if the same vial of antibiotic or solvent is used for multiple patients.
Excessive intracameral cefuroxime may cause macular edema, anterior and posterior segment inflammation, retinal vascular leakage and/or infarction, uveitis, and a decrease in long-term retinal function [49,50,51] Adverse reactions to the standard intracameral dose of 1.0 mg/0.1 mL are relatively rare and include serous macular detachment, increased central foveal thickness, anterior chamber inflammation, and vitritis [50]. Intracameral cefuroxime is also associated with the toxic anterior segment syndrome (TASS), a vision-threatening, noninfectious inflammation that begins within 24 h following surgery. TASS is characterized by corneal endothelial dysfunction and the absence of vitreous cells, and TASS cases often occur in clusters. TASS must be differentiated from infectious endophthalmitis because TASS responds favorably to topical corticosteroid administration and does not require antibiotics [52].
Enterococci are resistant to cefuroxime, and the routine use of intracameral cefuroxime in Sweden was associated with an increased proportion of Enterococci endophthalmitis cases [44]. Fungal endophthalmitis has also been seen following the use of intracameral cefuroxime, as a 2009 report described seven consecutive patients who developed Fusarium endophthalmitis due to a compounding error [53]. The final visual outcomes for these patients were between light perception and 20/100 despite treatment with local and systemic antifungal medications. Two patients with penicillin or cephalosporin allergies suffered anaphylactic reactions following intracameral cefuroxime [54, 55], but despite these cases, cefuroxime can usually be administered safely to patients with penicillin or cephalosporin allergies, although discussing this risk with patients may prove to be difficult [50].
Moxifloxacin, a fourth-generation fluoroquinolone that was first approved in 2003 for topical ophthalmic use in the treatment of bacterial conjunctivitis, is commonly used as intracameral prophylaxis. Moxifloxacin inhibits DNA gyrase and topoisomerase IV, both of which are necessary for bacterial cell replication because they separate bacterial DNA. Of the three commonly used antibiotics mentioned above, moxifloxacin has the broadest spectrum of coverage, with activity against both Gram-positive and Gram-negative bacteria, including Pseudomonas aeruginosa. It is biphasic, with an initial dose-dependent activity profile; after injection it remains bactericidal for a much longer time than cefuroxime, even at low injection concentrations [56]. Other advantages of moxifloxacin for ophthalmic use include its pH, tonicity, and lack of preservative [32]. In most countries it must be compounded prior to use. In India, where over one million cataract surgeries are performed each year, moxifloxacin PF hydrochloride (Promox®; Aurolab, Madurai, India) for intracameral use has been manufactured since 2013, and it currently accounts for more than 90% of intracameral antibiotic use in India [58]. The Aravind Eye Care System, which comprises ten surgical facilities and considers intracameral moxifloxacin to be standard-of-care after routine surgery, demonstrated a fourfold reduction in the rate of endophthalmitis following cataract surgery [57]. Unfortunately, moxifloxacin may be becoming less effective as a prophylaxis for endophthalmitis because repeated contact with ocular and nasopharyngeal flora has promoted the growth of resistant bacteria [59]. Coagulase-negative Staphylococcus spp. have become increasingly resistant to all fluoroquinolones, including moxifloxacin, with susceptibility rates that have decreased from 77.0% to 43.0% since 2004 [60]. Moxifloxacin is the most expensive of the three current antibiotics of choice, and routine use would significantly increase the total cost of cataract surgery in the USA. The use of intracameral moxifloxacin is not supported by level I evidence.
Vancomycin inhibits cell-wall synthesis in a time-dependent manner similar to cefuroxime. It is effective against nearly all Streptococci and Staphylococci species, including methicillin-resistant Staphylococcus aureus (MRSA), which may cause up to 2% of POE. It has no activity against the majority of Gram-negative organisms, which have been reported to cause up to 10% of POE [61]. Vancomycin was approved by the FDA in 1958 for intravenous administration, and although there is no commercially approved intraocular formulation, it is a commonly used intravitreal antibiotic for the treatment of endophthalmitis. When used prophylactically, 1 mg/0.1 mL is injected at the completion of cataract surgery. A large (14,805 cataract cases) retrospective cohort study from Australia demonstrated a ninefold reduction in endophthalmitis (0.43% vs. 0.049%; P < 0.0001) during the years 2000–2014 following the introduction of vancomycin prophylaxis [62]. Vancomycin has become the antibiotic of choice for 12.1% of Australian ophthalmologists who routinely use intracameral antibiotics [63]. A meta-analysis that included 17 studies found a lower average weighted incidence of POE with vancomycin compared to cefuroxime and moxifloxacin (0.0106%, 0.0332%, and 0.0153%, respectively) [61].
The routine use of vancomycin is of considerable concern because it has been associated with hemorrhagic occlusive retinal vasculitis (HORV), which is a delayed-onset/type III hypersensitivity reaction. HORV was first reported in 2014, and the first case from Australia, where vancomycin seems to be most popular, was reported in 2016. In light of vancomycin’s known systemic effects, it has been suggested that HORV represents a leukocytoclastic retinal vasculitis. However, recent histopathologic examination of an enucleated eye suggests that HORV may be a primary choroidopathy, with secondary effects on the overlying retina [64, 65]. All cases of HORV present within 2 weeks of surgery, usually with painless vision loss and minimal vitreous inflammation. A 2016 joint task force of the American Society of Retina Specialists and the ASCRS reported that patients seek treatment for HORV at an average of 8 days after cataract surgery. Visual acuity results from HORV are poor, with 61% of eyes (22/36) having 20/200 or worse and 22% (8/36) losing all perception of light [66]. Prophylactic use of vancomycin potentially compromises its efficacy as a treatment for POE because it may promote the development of resistant organisms. A 2016 literature review noted poor visual outcomes in 27 cases of endophthalmitis due to organisms with either reduced susceptibility or resistance to vancomycin [67]. Additionally, vancomycin is not active against Gram-negative organisms, which are responsible for a small percentage of POE cases.
The economic risks of routine intracameral prophylaxis ought to be noted, since a prohibitively high cost is the primary reason given by Americans for not accessing health care [68]. Routine use of intracameral antibiotics may significantly increase healthcare costs. Approximately three million cataract surgeries are performed each year in the USA. The acquisition and patient costs of the three commonly used antibiotics are as follows: cefuroxime ($5.08 and $80.16); vancomycin ($82.08 and $234.16); and moxifloxacin ($41.18 and $152.36). Some operating rooms obtain multiple doses of antibiotics from a single vial, a practice that is contrary to the recommendations in chapter 797 of the United States Pharmacopoeia (United States Pharmacopeial Convention, Rockville, MD, USA) and should be avoided if possible. Pharmacokinetic studies show that half of the injected cefuroxime is eliminated from the anterior chamber approximately 4–5 h after surgery, yet organisms may enter a non-sutured anterior chamber from the eyelids and the environment at any time during the first few postoperative days. This phenomenon calls into further question the efficacy and financial practicality of routine intracameral antibiotic use [69].
Post-operative Care
Many patients are treated with topical antibiotics post-operatively despite the fact that no drops have been approved by the FDA for routine use with cataract surgery. A 2017 review article noted that most ophthalmologists throughout the world prescribe topical antibiotics post-operatively, although the results from Russia and Mexico included in this review article were based on unpublished data [70]. There is no uniformly preferred regimen, so the choice of antibiotics depends on the surgeon’s preference, with the most common choices being similar to those prescribed pre-operatively, including fluoroquinolones, aminoglycosides, and chloramphenicol. Additionally, trimethoprim-polymyxin B and tobramycin provide excellent coverage against Staphylococcus spp., with 87.5% and 93.6% of colonies being sensitive to each of the respective antibiotics. Trimethoprim-polymyxin B has the added benefit of covering Streptococcus pneumoniae and Pseudomonas [71]. The best time to start antibiotics in the post-operative patient has not been determined, and timing thus varies according to surgeon preference. In the ESCRS study, topical antibiotics were started the day following surgery rather than immediately post-operatively. A retrospective study from the Moran Eye Center demonstrated an increased risk of endophthalmitis when antibiotics were started the day after surgery rather than on the day of surgery (odds ratio 13.7; P = 0.05) [72].
Subconjunctival injections of antibiotics and steroids are commonly administered after many intraocular procedures, but their use following cataract surgery is decreasing. For cataract surgeries, however, the major beneficiaries of subconjunctival injections are patients who, for any variety of reasons, may be unable to comply with a post-operative eye drop regimen. Choices of antibiotics include cefuroxime and gentamicin, in addition to corticosteroids, such as methylprednisolone. Despite concerns regarding penicillin hypersensitivity, a study by Mittra and McElvanney of 36 patients with penicillin allergy who had previous reactions ranging from rashes to loss of consciousness found cross-reaction with subconjunctival cefuroxime injections to be low [73]. These authors also concluded that cefuroxime is better than many other drugs because of its broad spectrum bactericidal activity and low toxicity [73]. Subconjunctival injections of methylprednisolone may be as safe and effective as drops, with the added benefit of nullifying compliance issues [74].
Mayo Clinic Data
The ESCRS trial is frequently cited for providing the best evidence in support of the prophylactic intracameral use of antibiotics. This multicenter, prospective, multi-armed trial studied 13,698 patients at 24 ophthalmology centers throughout Europe. Patients were randomized to one of four groups: no prophylactic antibiotics; topical antibiotics only; intracameral cefuroxime only; both topical antibiotics and intracameral cefuroxime. Cefuroxime was compounded for intracameral use because a single-use commercial product was not yet available. The primary endpoint was the development of endophthalmitis. The incidences of endophthalmitis among the four groups were 13/3438 (0.38%), 10/3424 (0.29%), 3/3408 (0.09%), and 2/3428 (0.06%), respectively. As detailed in Table 1, the incidence of endophthalmitis was significantly better in patients who received intracameral cefuroxime (5/6836; 0.07%) than in those who did not receive cefuroxime (23/6862; 0.33%), but the incidence of endophthalmitis in patients who received levofloxacin eye drops (12/6852; 0.18%) was not significantly different from those who did not receive drops (16/6846; 0.23%). The following risk factors for the development of endophthalmitis were also noted: clear corneal incision (5.88× higher) versus scleral tunnel incision; silicone intraocular lens (3.3× higher) versus acrylic lens; and surgical complications (4.95× higher) versus none.
Several problems with the design and results of the ESCRS trial deserve discussion. The cefuroxime required compounding at each site because the commercially available product, now used throughout Europe, was not available at the time of the trial. The levofloxacin eye drops were started the day after surgery. The trial was stopped prematurely because of an apparent treatment effect in favor of intracameral cefuroxime.
One of the major problems with the ESCRS trial was the very high rate of endophthalmitis (0.33%) in the cohorts not receiving intracameral cefuroxime. This surprisingly high rate more easily allowed intracameral cefuroxime to significantly improve the endophthalmitis rate over cohorts not receiving cefuroxime. We believe that good aseptic technique by the operating room staff (equipment sterilization, operating theater construction, room setup, gowns, gloves and other factors) combined with good surgical technique should produce endophthalmitis rates that not only exceed those of the non-intracameral antibiotic cohorts in the ESCRS trial, but should also rival the rates achieved with the injection of cefuroxime.
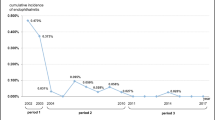
To test the above hypothesis, we determined the post-cataract extraction endophthalmitis rates from the three major ophthalmology sites within the Mayo Clinic Foundation—Arizona, Minnesota, and Florida. The sites function independently, with little exchange of staff between operating rooms and Ophthalmology departments, but aseptic and surgical procedures and techniques are frequently discussed by all sites and, when possible, converged.
Senior cataract surgeons at each of the three sites were asked to provide a retrospective total of cataract surgeries and endophthalmitis cases for the 5-year period 2012–2016. During this period, topical fluoroquinolone antibiotic drops were used routinely before and after surgery, but intracameral antibiotics were not used. As detailed in Table 2, the numbers of endophthalmitis cases, cataract surgeries, and endophthalmitis rates were as follows: Arizona—1/3535, 0.028%; Florida—1/4495, 0.022%; Minnesota—3/16250, 0.0185%. The aggregate rate was 0.02%. This compares favorably with the ESCRS endophthalmitis rate in eyes that received intracameral cefuroxime—0.073%. A Chi-square analysis determined that the Mayo Clinic endophthalmitis rate without the use of intracameral antibiotics was significantly better than the ESCRS rate with intracameral cefuroxime (P = 0.03).
Discussion
Post-operative endophthalmitis is not a “never event,” but with careful attention to detail, endophthalmitis rates from most ophthalmologic surgical facilities can probably be improved. Strict antisepsis practices should be the primary approach to endophthalmitis prevention since they are supported by centuries of surgical practice and will likely have the greatest and longest lasting impact. Surgeons wishing to improve their endophthalmitis rates should carefully assess all aspects of their operating room preparation and sterile technique. The use of povidone-iodine is the only antibiotic/antisepsis practice supported by level I evidence, but despite this, use of povidone-iodine is only 94% in India, and some aspects of preparation may not be fully optimized [58]. The authors believe that unless endophthalmitis rates within an institution are less than 1/1000 (0.1%), surgeons should critically evaluate their asepsis practices. Intracameral antibiotics can be incorporated into their practices, but unless asepsis is carefully and systematically optimized, endophthalmitis rates will always be higher than is necessary.
Among U.S. cataract surgeons, 47% either use or plan to use routine intracameral antibiotics, and it has been estimated that between 30% and 50% of all antibiotic use in ambulatory medicine is unnecessary or inappropriate [75, 76]. Inappropriate use of antibiotics adds significantly to the cost of medical care, exposes patients to unnecessary risks of drug-related adverse events, and increases the prevalence of antibiotic-resistant organisms. Before adopting the routine use of intracameral antibiotics, ophthalmologists need to consider the large burden of unnecessary treatment that is associated with intracameral prophylaxis.
Gower et al. found high-certainty evidence that intracameral cefuroxime with or without topical levofloxacin lowers the risk of endophthalmitis, and moderate evidence that the two methods together are better than either alone [33]. However, the heterogeneity of the study designs and modes of antibiotic delivery among reported studies made it impossible for them to conduct a formal meta-analysis [33]. A recent meta-analysis of 33 studies identified confounding variables and protocol deviations as the principle causes of moderate to high bias, and lack of homogeneity between studies was cited as the greatest challenge to comparing studies [61].
There is no FDA-approved product available for intracameral use in the USA at this time and preparing the antibiotics requires a reliable compounding pharmacy or a skilled nurse in the operating theater. While cefuroxime may be effective, it is not without risks. Javitt argues that the economic return on making an approved product readily available to U.S. physicians is likely to be minimal [77].
In light of the available data, routine use of intracameral antibiotics should be carefully considered since the ESCRS study remains the only RCT published to date. Results from recent “big data” reports and large retrospective studies are compelling, but these studies have limitations in study design and potential inaccuracies in diagnosis and procedure coding. Nonetheless, the strong trend throughout much of the world favors increasing the routine use of intracameral antibiotics. Surgeons electing to routinely use intracameral antibiotics should optimize their aseptic practices, adequately train staff in the preparation and use of antibiotics, and vigilantly monitor patients for antibiotic-related complications. Finally, in order to provide surgeons with reliable, actionable data, a carefully designed, multicenter RCT evaluating the efficacy of intraocular antibiotics needs to be performed.
References
Pandya HK, Lawton HW, Clark WL, Trattler WB, Kaiser PK. Postoperative endophthalmitis. www.emedicine.com/oph/topic394.htm. Accessed 30 Apr 2018.
Vaziri K, Schwartz SG, Kishor K, Flynn HW Jr. Endophthalmitis: state of the art. Clin Ophthalmol. 2015;9:95–108.
Frost BA, Kainer MA. Safe preparation and administration of intravitreal bevacizumab injections. N Engl J Med. 2011;365:2238.
Schachat AP, Rosenfeld PJ, Liesegang TJ, Stewaart MW. Endophthalmitis is not a “never event”. Ophthalmology. 2012;119:1507–8.
Ciulla TA, Starr MB, Masket S. Bacterial endophthalmitis prophylaxis for cataract surgery: an evidence-based update. Ophthalmology. 2002;109(1):13–24.
Herrinton LJ, Shorstein NH, Paschal JF, et al. Comparative effectiveness of antibiotic prophylaxis in cataract surgery. Ophthalmology. 2016;123(2):287–94.
Costea C, Sava A, Dimitriu G, et al. A brief account of the long history of cataract surgery. Rom J Funct Clin. 2016;15(1):7.
McGrath D. ‘Couching’ for cataracts remains a persistent problem in Yemen. In: EuroTimes. European Society of Cataract and Refractive Surgeons, Dublin, September 2005.
Isawumi MA, Kolawole OU, Hassan MB. Couching techniques for cataract treatment in Osogbo, South west Nigeria. Ghana Med J. 2013;47(2):64–9.
Schemann JF, Bakayoko S, Coulibaly S. Traditional couching is not an effective alternative procedure for cataract surgery in Mali. Ophthalmic Epidemiol. 2000;7(4):271–83.
Goyal M, Hogeweg M. Couching and cataract extraction. A clinical based study in northern. Nigeria. Community Eye Health J. 1997;10:6–8.
Siddig MA, Ali NAM. Complications of couching and visual outcome after IOL implantation—a study of 60 patients in Sudan. Sudan J Opthamol. 2018;1(1):33–6.
La. PFd. Memoirs of the Royal Academy of Surgery. Royal Academy of Surgery, London. 1753.
Ellett EC. Use of the suture in extraction of cataract. Arch Ophthalmol. 1937;17(3):523–9.
Obuchowska I, Mariak Z. Jacques Daviel—the inventor of the extracapsular cataract extraction surgery. Klin Oczna. 2005;107(7–9):567–71.
Bellan L. The evolution of cataract surgery: the most common eye procedure in older adults. Geriatr Aging MedScape. 2008;11:328–32.
Levison AL, Mendes TS, Bhisitkul R. Postprocedural endophthalmitis: a review. Exp Rev Ophthalmol. 2013;8(1):45–62.
Al Mahmood AM, Al-Swailem SA, Behrens A. Clear corneal incision in cataract surgery. Middle East Afr J Ophthalmol. 2014;21:25–31.
Leaming DV. Practice styles and preferences of ASCRS members—2003 survey. J Cataract Refract Surg. 2004;30(4):892–900.
Alio JL, Abdou AA, Puente AA, Zato MA, Nagy Z. Femtosecond laser cataract surgery: updates on technologies and outcomes. J Refract Surg. 2014;30(6):420–7.
Donaldson KE, Braga-Mele R, Cabot F, et al. Femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2013;39(11):1753–63.
Isenberg S, Apt L, Yoshimoro R. Chemical preparation of the eye in ophthalmic surgery: effectiveness of mild silver protein solution. Arch Ophthalmol. 1983;101:764–5.
Apt L, Isenberg S, Yoshimori R, Paez JH. Chemical preparation of the eye in ophthalmic surgery. III. Effect of povidone-iodine on the conjunctiva. Arch Ophthalmol. 1984;102(5):728–9.
Art G. Combination povidone-iodine and alcohol formulations more effective, more convenient versus formulations containing either iodine or alcohol alone: a review of the literature. J Infus Nurs. 2005;28(5):314–20.
Haripriya A. Antibiotic prophylaxis in cataract surgery—an evidence-based approach. Indian J Ophthalmol. 2017;65(12):1390–5.
Schmitz S, Dick HB, Krummenauer F, Pfeiffer N. Endophthalmitis in cataract surgery: results of a German survey. Ophthalmology. 1999;106(10):1869–77.
Grzybowski A, Schwartz SG, Matsuura K, et al. Endophthalmitis prophylaxis in cataract surgery: overview of current practice patterns around the world. Curr Pharm Des. 2017;23(4):565–73.
Chang DF, Braga-Mele R, Henderson BA, Mamalis N, Vasavada A. Antibiotic prophylaxis of postoperative endophthalmitis after cataract surgery: results of the 2014 ASCRS member survey. J Cataract Refract Surg. 2015;41(6):1300–5.
Grzybowski A, Kuklo P, Pieczynski J, Beiko G. A review of preoperative manoeuvres for prophylaxis of endophthalmitis in intraocular surgery: topical application of antibiotics, disinfectants, or both? Curr Opin Ophthalmol. 2016;27(1):9–23.
An JA, Kasner O, Samek DA, Levesque V. Evaluation of eyedrop administration by inexperienced patients after cataract surgery. J Cataract Refract Surg. 2014;40(11):1857–61.
Davies I, Williams AM, Muir KW. Aids for eye drop administration. Surv Ophthalmol. 2017;62(3):332–45.
Lindstrom RL, Galloway MS, Grzybowski A, Liegner JT. Dropless cataract surgery: an overview. Curr Pharm Des. 2017;23(4):558–64.
Gower EW, Lindsley K, Tulenko SE, Nanji AA, Leyngold I, McDonnell PJ. Perioperative antibiotics for prevention of acute endophthalmitis after cataract surgery. Cochrane Database Syst Rev. 2017;2:Cd006364.
Liesegang TJ. Intracameral antibiotics: questions for the United States based on prospective studies. J Cataract Refract Surg. 2008;34(3):505–9.
Coleman AL. How big data informs us about cataract surgery: the LXXII Edward Jackson memorial lecture. Am J Ophthalmol. 2015;160(6):1091–3.
Daien V, Villain M, Creuzot-Garcher C. Comparison of recent studies of postoperative endophthalmitis from the same national database: in reply. JAMA Ophthalmol. 2017;135:174.
Francis IC, Roufas A, Figueira EC, Pandya VB, Bhardwaj G, Chui J. Endophthalmitis following cataract surgery: the sucking corneal wound. J Cataract Refract Surg. 2009;35:1643–5.
Marcus G, Davis E. Eight (no, Nine!) Problems with big data. New York: New York Times 2014;A23.
Barry P, Javitt JC. Intracameral antibiotics reduce the risk of endophthalmitis after cataract surgery: does the preponderance of the evidence mandate a global change in practice? (Ophthalmology 2016;123:226–231). Ophthalmology. 2017;124(1):e7–8.
Arshinoff SA, Bastianelli PA. Incidence of postoperative endophthalmitis after immediate sequential bilateral cataract surgery. J Cataract Refract Surg. 2011;37(12):2105–14.
Barreau G, Mounier M, Marin B, Adenis JP, Robert PY. Intracameral cefuroxime injection at the end of cataract surgery to reduce the incidence of endophthalmitis: french study. J Cataract Refract Surg. 2012;38(8):1370–5.
van der Merwe J, Mustak H, Cook C. Endophthalmitis prophylaxis with intracameral cefuroxime in South Africa. J Cataract Refract Surg. 2012;38(11):2054.
Wejde G, Montan P, Lundstrom M, Stenevi U, Thorburn W. Endophthalmitis following cataract surgery in Sweden: national prospective survey 1999–2001. Acta Ophthalmol Scand. 2005;83(1):7–10.
Creuzot-Garcher C, Benzenine E, Mariet AS, et al. incidence of acute postoperative endophthalmitis after cataract surgery: a Nationwide Study in France from 2005 to 2014. Ophthalmology. 2016;123(7):1414–20.
Garat M, Moser CL, Alonso-Tarres C, Martin-Baranera M, Alberdi A. Intracameral cefazolin to prevent endophthalmitis in cataract surgery: 3-year retrospective study. J Cataract Refract Surg. 2005;31:2230–4.
Romero P, Mendez I, Salvat M, Fernandez J, Almena M. Intracameral cefazolin as prophylaxis against endophthalmitis in cataract surgery. J Cataract Refract Surg. 2006;32(3):438–41.
Ng AL, Tang WW, Li PS, Li KK. Intracameral cefuroxime in the prevention of postoperative endophthalmitis: an experience from Hong Kong. Graefes Arch Clin Exp Ophthalmol. 2016;254(10):1987–92.
Nguyen ET, Shorstein NH. Preparation of intracameral antibiotics for injection. J Cataract Refract Surg. 2013;39(11):1778–9.
Delyfer MN, Rougier MB, Leoni S, et al. Ocular toxicity after intracameral injection of very high doses of cefuroxime during cataract surgery. J Cataract Refract Surg. 2011;37(2):271–2.
Al-Abduljabbar KA, Stone DU. Risks of cefuroxime prophylaxis for postcataract endophthalmitis. Middle East Afr J Ophthalmol. 2017;24(1):24–9.
Gimenez-de-la-Linde M, Gimenez-Alcantara B, Baranano-Alcaide R, Cordoves-Dorta L, Abreu-Reyes JA. Macular oedema after uncomplicated cataract surgery. Possible relationship with the volume of intracameral cefuroxime. Arch Soc Esp Oftalmol. 2017;92(1):49–50.
Mamalis N, Edelhauser HF, Dawson DG, Chew J, LeBoyer RM, Werner L. Toxic anterior segment syndrome. J Cataract Refract Surg. 2006;32(2):324–33.
Cakir M, Imamoglu S, Cekic O, et al. An outbreak of early-onset endophthalmitis caused by Fusarium species following cataract surgery. Curr Eye Res. 2009;34(11):988–95.
Villada JR, Vicente U, Javaloy J, Alio JL. Severe anaphylactic reaction after intracameral antibiotic administration during cataract surgery. J Cataract Refract Surg. 2005;31(3):620–1.
Moisseiev E, Levinger E. Anaphylactic reaction following intracameral cefuroxime injection during cataract surgery. J Cataract Refract Surg. 2013;39(9):1432–4.
Arshinoff SA, Modabber M. Dose and administration of intracameral moxifloxacin for prophylaxis of postoperative endophthalmitis. J Cataract Refract Surg. 2016;42(12):1730–41.
Haripriya A, Chang DF, Namburar S, Smita A, Ravindran RD. Efficacy of intracameral moxifloxacin endophthalmitis prophylaxis at Aravind Eye Hospital. Ophthalmology. 2016;123(2):302–8.
Kelkar AS, Chang DF, Kelkar JA, Mehta HM, Lahane T, Parekh R. Antibiotic prophylaxis practice patterns for cataract surgery in India—results from an online survey. Indian J Ophthalmol. 2017;65(12):1470–4.
Kim SJ, Toma HS. Ophthalmic antibiotics and antimicrobial resistance a randomized, controlled study of patients undergoing intravitreal injections. Ophthalmology. 2011;118(7):1358–63.
Stringham JD, Relhan N, Miller D, Flynn HW Jr. Trends in fluoroquinolone nonsusceptibility among coagulase-negative Staphylococcus isolates causing endophthalmitis, 1995–2016. JAMA Ophthalmol. 2017;135(7):814–5.
Bowen RC, Zhou AX, Bondalapati S, et al. Comparative analysis of the safety and efficacy of intracameral cefuroxime, moxifloxacin and vancomycin at the end of cataract surgery: a meta-analysis. Br J Ophthalmol. 2018. doi:https://doi.org/10.1136/bjophthalmol-2017-311051.
Au CP, White AJ, Healey PR. Efficacy and cost-effectiveness of intracameral vancomycin in reducing postoperative endophthalmitis incidence in Australia. Clin Exp Ophthalmol. 2016;44(9):803–11.
Hsing YE, Park J. Haemorrhagic occlusive retinal vasculitis associated with intracameral vancomycin during cataract surgery. Clin Exp Ophthalmol. 2016;44(7):635–7.
Todorich B, Faia LJ, Thanos A, et al. Vancomycin-associated hemorrhagic occlusive retinal vasculitis: a clinical-pathophysiological analysis. Am J Ophthalmol. 2018;188:131–40.
Nicholson LB, Kim BT, Jardon J, et al. Severe bilateral ischemic retinal vasculitis following cataract surgery. Ophthalmic Surg Lasers Imaging Retina. 2014;45(4):338–42.
Witkin AJ, Chang DF, Jumper JM, et al. Vancomycin-associated hemorrhagic occlusive retinal vasculitis: clinical characteristics of 36 eyes. Ophthalmology. 2017;124(5):583–95.
Relhan N, Albini TA, Pathengay A, Kuriyan AE, Miller D, Flynn HW. Endophthalmitis caused by Gram-positive organisms with reduced vancomycin susceptibility: literature review and options for treatment. Br J Ophthalmol. 2016;100(4):446–52.
Department for Professional Employees, AFL-CIO. The U.S. health care system: an international perspective. Washington: Department for Professional Employees; 2016. http://dpeaflcio.org/programs-publications/issue-fact-sheets/the-u-s-health-care-system-an-international-perspective/
Lee MB, Bobba S, Francis IC. Comparison of recent studies of postoperative endophthalmitis from the same national database. JAMA Ophthalmol 2017;135(2):173–4.
Endophthalmitis Study Group, European Society of Cataract & Refractive Surgeons. Prophylaxis of postoperative endophthalmitis following cataract surgery. results of the ESCRS multicenter study and identification of risk factors. J Cataract Refract Surg. 2007;33(6):978–88.
Crowell EL, Koduri VA, Groat RS, Lee DA. Cost comparison of commonly used postoperative topical ophthalmic antibiotics. J Cataract Refract Surg. 2017;43(10):1322–7.
Wallin T, Parker J, Jin Y, Kefalopoulos G, Olson RJ. Cohort study of 27 cases of endophthalmitis at a single institution. J Cataract Refract Surg. 2005;31(4):735–41.
Mitra A, McElvanney A. Prophylactic subconjunctival cefuroxime during cataract surgery in patients with a penicillin allergy. Ann Ophthalmol (Skokie); 2006;38(4):293–5.
Merkoudis N, Wikberg Matsson A, Granstam E. Comparison of peroperative subconjunctival injection of methylprednisolone and standard postoperative steroid drops after uneventful cataract surgery. Acta Ophthalmol. 2014;92(7):623–8.
Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010–2011. JAMA. 2016;315(17):1864–73.
Spellberg B, Srinivasan A, Chambers HF. New societal approaches to empowering antibiotic stewardship. JAMA. 2016;315(12):1229–30.
Javitt JC. Intracameral antibiotics reduce the risk of endophthalmitis after cataract surgery: does the preponderance of the evidence mandate a global change in practice? Ophthalmology. 2016;123(2):226–31.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
Nicholas K. George has nothing to disclose. Michael W. Stewart, Alkahest: Consultant, Allergan: Institutional research support, Bayer: Consultant, Regeneron: Institutional research support
Compliance With Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced digital features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.6683093.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
George, N.K., Stewart, M.W. The Routine Use of Intracameral Antibiotics to Prevent Endophthalmitis After Cataract Surgery: How Good is the Evidence?. Ophthalmol Ther 7, 233–245 (2018). https://doi.org/10.1007/s40123-018-0138-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-018-0138-6