Abstract
Introduction
While it is widely recognized that older adults, adults with chronic medical conditions (CMC), and adults with immunocompromising conditions (IC) are at increased risk of lower respiratory tract illness (LRTI), evidence of the magnitude of increased risk is limited. This study was thus undertaken to characterize rates of hospitalized and ambulatory LRTI among United States (US) adults by age and comorbidity profile.
Methods
A retrospective cohort design and US healthcare claims database (2016–2019) were employed. Study population included adults aged ≥ 18 years and was stratified by age and comorbidity profile (CMC−, CMC+ , IC). LRTI was ascertained overall and by pathogen pathogen (e.g., respiratory syncytial virus [RSV]), and was classified by care setting (hospital, emergency department [ED], physician office/hospital outpatient [PO/HO]).
Results
Relative rates (RR) of LRTI generally increased with older age across care settings (vs. 18–49 years), with the most marked increase for hospitalizations: for LRTI-hospitalized, RRs ranged from 3.3 for 50–64 years to 46.6 for ≥ 85 years; for LRTI-ED and LRTI-PO/HO, RRs ranged from 1.0 to 2.7 and from 1.3 to 1.5, respectively. Within age groups, LRTI rates were also consistently higher among CMC+ and IC adults (vs. CMC− adults). Age-specific RRs of LRTI patients hospitalized due to RSV were largely comparable to overall LRTI; age-specific RRs for other care settings, and RRs for CMC+ and IC adults (vs. CMC− adults), were generally higher for LRTI due to RSV.
Conclusions
Incidence of LRTI, including that due to RSV, especially for events requiring acute inpatient care, is markedly higher among older adults and adults of all ages with CMC or IC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Acute lower respiratory tract illnesses (LRTI) are one of the leading causes of morbidity and mortality among adults. |
While adult rates of LRTI are known to increase with age and the presence of medical conditions, a comprehensive evaluation of adult LRTI rates by care setting, age, and comorbidity profile is not currently available. |
This study was undertaken to better understand the magnitude of increased LRTI rates across adult subgroups and to inform public health strategies to prevent LRTI. |
What was learned from this study? |
Rates of LRTI among US adults, especially LRTI requiring hospitalization, are markedly higher among older adults and adults of all ages with underlying chronic or immunocompromising conditions. |
Study findings suggest that strategies to prevent LRTI should target not only older adults but also younger adults with medical conditions. |
Introduction
Acute lower respiratory tract illnesses (LRTI) include infections of the lung (pneumonia) and infections affecting the airways such as acute bronchitis and acute bronchiolitis [1]. LRTIs are a leading cause of morbidity and mortality in the United States (US), with risk increasing among adults as they age [1]. In a 2015 US population-based surveillance study, the annual incidence rate of hospitalized pneumonia among adults aged 50–64 years, 65–79 years, and ≥ 80 years was reported to be, respectively, 3.9, 9.4, and 24.5 times the incidence rate in adults aged 18–49 years [2]. A similar trend was reported in a 2020 study of older adults in Louisville, Kentucky (relative rate [RR] [vs. 65–69]: 70–74 = 1.6; 75–78 = 1.8, 80–84 = 2.1; 85–89 = 2.9; 90–94 = 4.6; ≥ 95 = 4.9) [3]. In addition, about 5% of US adults have an episode of acute bronchitis each year, making it among the ten most common outpatient illnesses in the US [4].
Rates of these conditions are known to increase not only with increasing age among adults but also with the presence of chronic medical conditions (CMC) and immunocompromising conditions (IC) [5,6,7,8]. In a 2019 study evaluating three distinct study periods using two healthcare claims databases spanning 2005–2015, incidence rates (per 100,000 person-years) of hospitalized pneumonia among immunocompetent adults aged 50–64 years, 65–74 years, and ≥ 75 years were reported to be, respectively, 2.3–2.5, 5.1–5.4, and 20–27 times (depending on the study period) the rate among adults aged 18–49 years [7]. Moreover, rates of hospitalized pneumonia were 3–6 times higher among adults with CMC and 4–20 times higher among adults with IC across age groups, compared with corresponding rates of hospitalized pneumonia among immunocompetent adults without a CMC.
While several studies have evaluated rates of LRTI—overall and/or by specific clinical manifestation—among specific populations of adults, few have evaluated LRTI rates among younger and older US adults stratified by age, and even fewer have evaluated LRTI rates by care setting [5,6,7, 9,10,11,12,13]. Moreover, no studies—to the best of our knowledge—have evaluated rates of LRTI by care setting among US adults of all ages stratified by age and comorbidity profile. Because of the limitations of existing research, a new study using a large healthcare claims database was undertaken to address these evidence gaps and to better understand the epidemiology of LRTI among US adults.
Methods
Study Design and Data Sources
A retrospective cohort design and data from the Merative MarketScan Commercial Claims and Encounters (CCAE) and Medicare Supplemental and Coordination of Benefits (MDCR) Databases (the “MarketScan Database”) were employed. For this study, data from the MarketScan Database spanned January 2016 through December 2019. Although the study database included healthcare claims through the end of calendar year 2020, the study period was truncated at the end of 2019 to avoid confounding of study findings by the COVID-19 pandemic.
The CCAE Database includes healthcare claims and enrollment information from US employer-sponsored plans covering > 15 million working persons aged < 65 years each year, including employees, spouses, and dependents. The MDCR Database includes healthcare claims and enrollment information for retirees enrolled in US employer-sponsored Medicare supplemental plans. Facility and professional-service claims include dates and places of service, diagnoses and procedures, and quantity of services (professional service claims). Outpatient pharmacy claims include the drug name, dispensing date, dose, quantity, and therapy days. All claims also include amounts paid to healthcare providers by health plans and patients.
The study database was de-identified prior to its release to study investigators, as set forth in the corresponding Data Use Agreement. Use of the study database for health services research was fully compliant with the Health Insurance Portability and Accountability Act Privacy Rule and federal guidance on Public Welfare and the Protection of Human Subjects (45 CFR 46 §46.101). Institutional Review Board approval was not required.
Study Population
The study population comprised all adults who were aged ≥ 18 years at any time from January 2017 through December 2019, and who had at least 1 year of continuous healthcare coverage between January 2016 and December 2019. For each qualifying person, the day after the end date of the initial 1-year continuous enrollment period was designated as the “index date”.
Study Outcomes
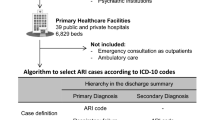
LRTI included episodes of influenza, pneumonia, bronchitis, bronchiolitis, unspecified acute lower respiratory infection, and other miscellaneous respiratory manifestations (Appendix 1) [14]. Episodes were ascertained on a monthly basis (i.e., in 30-day intervals) during the follow-up period, beginning on the index date and ending on the healthcare coverage end date or the end of the study period, whichever occurred first. All qualifying LRTI encounters occurring within 30 days of each other were considered part of the same episode; for patients with multiple episodes during their follow-up period, each one was considered separately in analyses. Episodes including a hospitalization for LRTI, irrespective of ambulatory LRTI encounters during the episode, were considered a hospitalized episode. Hospitalized LRTI was identified based on an acute-care inpatient admission with a corresponding diagnosis code in the principal or secondary positions. Ambulatory LRTI episodes were identified based on an outpatient encounter with a corresponding diagnosis code in any position and was further stratified by care setting (emergency department [ED] vs. physician office/hospital outpatient [PO/HO]).
Because testing for specific pathogens (e.g., respiratory syncytial virus [RSV]) is often not performed in clinical practice, and because pathogens detected via testing are not always recorded in healthcare claims, rates of LRTI due to specific pathogens are not reported in the current study [15, 16]. However, in light of the recent approval of RSV vaccines and recommendation for their use in clinical practice, LRTI due to RSV was identified based on the presence of corresponding diagnosis codes (Appendix 2) and RR of RSV-LRTI by age and comorbidity profile were estimated for purposes of comparison.
Population Characteristics
Baseline characteristics included age, sex, comorbidity profile, geographic region, and health plan type. Age was defined using a categorical stratification scheme (e.g., 18–49, 50–64, 65–74, 75–84, ≥ 85 years). Comorbidity profile was defined based on the presence or absence of high-risk medical conditions listed in the US Advisory Committee on Immunization Practices recommendations for influenza vaccination, as follows: CMC−, “immunocompetent without CMC”; CMC+ , “immunocompetent with a CMC”; and IC, “immunocompromised” [17]. An alternative, two-level stratification scheme for comorbidity profile (CMC− vs. CMC+ /IC) was also considered.
Presence of medical conditions among adults in the study population was ascertained at the beginning of each month of follow-up, based on healthcare claims information with service dates at any time prior to the month of follow-up. Medical conditions were thus defined as time-dependent variables and were ascertained using from 1 to 4 years of healthcare claims data, depending on the month/year during the follow-up period. Medical conditions were identified based on ≥ 2 outpatient diagnoses (≥ 7 days apart) or ≥ 1 inpatient diagnosis (Appendix 3). For patients with ≥ 2 outpatient diagnoses, the date of first evidence was employed.
Statistical Methods
Characteristics of adults in the study population, overall and within subgroups defined by age and comorbidity profile, were summarized using descriptive statistics (i.e., means/standard deviation [SD], %). Rates of LRTI were reported per 100,000 person-years, and were adjusted for differential follow-up using a population-based approach. Techniques of nonparametric bootstrapping were used to characterize 95% confidence intervals (CI) for rates and corresponding RRs (i.e., by age and comorbidity profile). Age- and comorbidity-specific RRs were estimated for LRTI due to any pathogen and LRTI due to RSV. Analyses were conducted considering all calendar months and, alternatively, considering only calendar months during a typical respiratory season, which was assumed to span November through April in each year of the study period [18].
Results
Population Characteristics
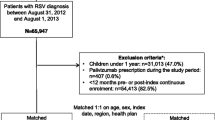
A total of 28.3 million adults were aged ≥ 18 years and had one or more days of healthcare coverage at any time from January 2017 through December 2019. Among these persons, 22.2 million had at least 1 year of continuous healthcare coverage between January 2016 and December 2019 and were thus included in the study population. Mean age of the study population was 43 (SD 16) years; 63% of persons were aged 18–49 years, 30% were aged 50–64 years, and 7% were aged ≥ 65 years (Table 1).
Most (80%) adults were classified as CMC−, 17% as CMC+, and 3% as IC. The percentage of adults classified as CMC+ increased with increasing age, from 10% among those aged 18–49 years to 61% among adults aged ≥ 85 years; corresponding values for adults classified as IC were 1.3% and 12%. Population characteristics based on the two-level stratification scheme are included in the Online Supplement (OS—Table 1).
Rates of LRTI
Incidence rates of hospitalized LRTI (per 100,000 person-years) increased with increasing age, from 148 for ages 18–49 years to 6,884 for ages ≥ 85 years; RRs (vs. ages 18–49 years) were 3.3 for ages 50–64 years, 9.6 for ages 65–74 years, 23.0 for ages 75–84 years, and 46.6 for ages ≥ 85 years (Table 2). Rates and RRs of hospitalized LRTI were also higher among CMC+ adults and IC adults (vs. CMC−) within each age group. For CMC+ adults, RRs ranged from 9.4 to 15.5; corresponding values for IC adults were 10.9 and 41.1. The percentage of all LRTI episodes that were classified as hospitalized increased from 2.1% for ages 18–49 years to 39.2% for ages ≥ 85 years, and was substantially higher for CMC+ and IC adults (vs. CMC−). For example, among adults aged 65–74 years, 15% and 22% of LRTI episodes among CMC+ adults and IC adults, respectively, required hospitalization, versus 2% among CMC− adults. For hospitalized LRTI, pneumonia was, by far, the most common diagnosis (≥ 80% of cases).
Rates of ED and PO/HO LRTI (per 100,000 person-years) also generally increased with increasing age: ED, from 567 for ages 18–49 years to 1,527 for ages ≥ 85 years; and PO/HO, from 6,458 for ages 18–49 years to 9162 for ages ≥ 85 years. For ED LRTI, RRs (vs. ages 18–49 years) ranged from 1.0 to 2.7 across age groups; for PO/HO LRTI, RRs (vs. ages 18–49 years) ranged from 1.3 to 1.5. For CMC+ adults (vs. CMC−) within each age group, RRs ranged from 2.5 to 2.9 for ED and from 1.7 to 2.3 for PO/HO; for IC adults (vs. CMC−), RRs ranged from 2.7 to 3.2 for ED and from 1.7 to 2.8 for PO/HO. Common diagnoses for ED LRTI included bronchitis (≥ 65%), pneumonia (≥ 25%), and influenza (≥ 10%), and for PO/HO LRTI, bronchitis (≥ 55%), influenza (≥ 20%), and pneumonia (≥ 10%) (note, multiple LRTI diagnoses may have been observed during a single episode).
Age-specific RRs of hospitalized LRTI were largely comparable between LRTI due to any pathogen (i.e., on an overall basis) versus LRTI due to RSV (Fig. 1). In the ambulatory setting, age-specific RRs of LRTI due to RSV were 1.3–2.5 times higher versus LRTI due to any pathogen. Age- and comorbidity-specific RRs of LRTI due to any pathogen versus RSV followed a similar pattern (i.e., they were nominally higher for RSV) (Fig. 2). LRTI rates and RRs, and RSV RRs, based on the two-level stratification scheme are included in the Online Supplement (OS—Table 2). Rates were comparable, albeit somewhat lower, when limiting the analysis to the respiratory season.
Discussion
In this retrospective observational study including 22.2 million commercially insured adults aged ≥ 18 years, we evaluated incidence rates of LRTI and RRs of LRTI (overall and due to RSV) by age and comorbidity profile. Study findings indicate that rates of LRTI generally increased with older age across care settings, especially LRTI requiring hospitalization, and that, within age groups, LRTI rates were consistently higher among adults with versus without CMC/IC. Study findings also indicate that age-specific RRs of hospitalized LRTI due to RSV were comparable with results for overall LRTI; age-specific RRs for other care settings, and RRs for adults with versus without CMC/IC across care settings, were generally higher for LRTI due to RSV. These findings are especially important for public health policy in light of the recent approval of RSV vaccines and recommendation for their use in US clinical practice [19].
Additionally, rates of ED LRTI and PO/HO LRTI were found to be comparable between all adults aged ≥ 65 years and adults aged < 65 years with CMC/IC. While rates of hospitalized LRTI were found to be slightly lower among younger adults with CMC/IC versus older adults, they were higher among younger adults with CMC/IC versus older adults without CMC. These findings suggest that strategies to prevent LRTI should target not only older adults but also younger adults with CMC/IC [20].
These findings build on those from previously published research. While direct comparisons of disease rates between studies are challenging due to differences in study designs, data sources, study populations, and study measures, comparisons of RRs are less problematic. For example, in the aforementioned retrospective evaluation by Pelton and colleagues, RRs of hospitalized pneumonia increased from 2.3–2.5 among adults aged 50–64 years to 20–27 among adults aged ≥ 75 years (vs. adults aged 18–49 years) [7]. The results from our study suggest that, for hospitalized LRTI, the gradient across ages may be somewhat steeper, with corresponding RRs increasing from 3.3 to 30 among adults aged ≥ 75 years (based on a weighted average of the two oldest age groups). A similar finding was observed for RRs by comorbidity profile. In the Pelton et al. study, rates of hospitalized pneumonia were 3–6 times higher among CMC+ adults and 4–20 times higher among IC adults (vs. adults without CMC), depending on age [7]. In our study, corresponding RRs increased ranged from 9–15 (CMC+) to 11–41 (IC).
While the MarketScan Database provides healthcare information for large numbers of patients, its use has several limitations in this study. Although the algorithm for identifying LRTI has been used in prior and ongoing studies, to the best of our knowledge, the algorithm has not been formally evaluated against a “gold standard”, and thus its accuracy (e.g., sensitivity, specificity, positive predictive value) is unknown [14]. While we used an operational algorithm to identify unique LRTI episodes per person based on a maximum 30-day window between encounters, some episodes occurring after an initial episode may not be unique (e.g., they may be a continuation of the previous episode) or may reflect a recurrent infection. We note that, when employing a 90-day (in lieu of a 30-day) window, rates of LRTI were comparable.
Most patients with LRTI are not tested for specific pathogens (such as RSV) in clinical practice, and pathogens detected via testing are not always recorded in healthcare claims. Accordingly, estimates of pathogen-specific LRTI rates based on healthcare claims data are downwardly biased; for this reason, rates of LRTI due to RSV were not reported [15]. Moreover, because RSV cases in this study may not be representative of all patients with RSV infection, and to the extent that RSV testing varies based on age and/or comorbidity profile, RRs of LRTI due to RSV may be mis-estimated.
Use of operational algorithms to characterize comorbidity profiles, which have been utilized in several previously published studies, undoubtedly resulted in misclassification of some adults who actually have the underlying conditions, as well as some adults who actually do not have the underlying conditions [5,6,7, 21, 22]. While the MarketScan Database includes information on a large number of patients across demographic profiles, providers, payors, and geographic regions, the source population is limited to US persons who are commercially insured and certain variables—such as socioeconomic status and race/ethnicity—are not available in the database. To the extent that commercially insured persons in the study database are systematically different in terms of, for example, race/ethnicity versus the US population, and to the extent that LRTI rates are higher among races/ethnicities who are under-represented in the study database, rates of LRTI reported here may be under-estimated relative to those among the overall US population. To ensure that sufficient claims information was available to characterize comorbidity profiles, the study population was limited to adults who had at least 1 year of healthcare coverage. To the extent that persons excluded from the study population (22% of 28.3 million) were systematically different than those included, the generalizability of results beyond the study population may be limited.
Conclusion
The findings from our study indicate that LRTI incidence, especially for events requiring acute inpatient care, is markedly higher among older adults and adults of all ages with CMC or IC. To address the burden of LRTI, prevention strategies, including vaccination when available, should focus on older adults and younger adults with comorbidities.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available due to data use agreements.
References
Feldman C, Shaddock E. Epidemiology of lower respiratory tract infections in adults. Expert Rev Respir Med. 2019;13(1):63–77.
Jain S, Self WH, Wunderink RG, et al. Community-acquired pneumonia requiring hospitalization among U.S. adults. New Engl J Med. 2015;373(5):415–27.
Arnold FW, Reyes Vega AM, Salunkhe V, et al. Older adults hospitalized for pneumonia in the United States: incidence, epidemiology, and outcomes. J Am Geriatr Soc. 2020;68(5):1007–14.
Singh A, Avula A, Zahn E. Acute bronchitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448067/.
Pelton SI, Shea KM, Weycker D, Farkouh RA, Strutton DR, Edelsberg J. Rethinking risk for pneumococcal disease in adults: the role of risk stacking. Open Forum Infect Dis. 2015;2(1):ofv020. https://doi.org/10.1093/ofid/ofv020.
Shea KM, Edelsberg J, Weycker D, Farkouh RA, Strutton DR, Pelton SI. Rates of pneumococcal disease in adults with chronic medical conditions. Open Forum Infect Dis. 2014;1(1):ofu024.
Pelton SI, Bornheimer R, Doroff R, Shea KM, Sato R, Weycker D. Decline in pneumococcal disease attenuated in older adults and those with comorbidities following universal childhood PCV13 immunization. Clin Infect Dis. 2019;68(11):1831–8.
Zimmerman RK, Lauderdale DS, Tan SM, Wagener DK. Prevalence of high-risk indications for influenza vaccine varies by age, race, and income. Vaccine. 2010;28(39):6470–7.
Hak E, Rovers M, Kuyvenhoven M, Schellevis F, Verheij T. Incidence of GP-diagnosed respiratory tract infections according to age, gender and high-risk co-morbidity: the Second Dutch National Survey of General Practice. Fam Pract. 2006;23(3):291–4.
Kumar R, Dar L, Amarchand R, et al. Incidence, risk factors, and viral etiology of community-acquired acute lower respiratory tract infection among older adults in rural north India. J Glob Health. 2021;11:04027–04027.
McDonald HI, Nitsch D, Millett ERC, Sinclair A, Thomas SL. New estimates of the burden of acute community-acquired infections among older people with diabetes mellitus: a retrospective cohort study using linked electronic health records. Diabet Med. 2014;31(5):606–14.
Millett ERC, Quint JK, Smeeth L, Daniel RM, Thomas SL. Incidence of community-acquired lower respiratory tract infections and pneumonia among older adults in the United Kingdom: a population-based study. PLoS One. 2013;8(9): e75131.
Trucchi C, Paganino C, Orsi A, et al. Hospital and economic burden of influenza-like illness and lower respiratory tract infection in adults ≥50 years-old. BMC Health Serv Res. 2019;19(1):585.
Lewnard JA, Bruxvoort KJ, Fischer H, et al. Effectiveness of 13-valent pneumococcal conjugate vaccine against medically-attended lower respiratory tract infection and pneumonia among older adults. Clin Infect Dis. 2022;75(5):832–41. https://doi.org/10.1093/cid/ciab1051.
McLaughlin JM, Khan F, Begier E, Swerdlow DL, Jodar L, Falsey AR. Rates of medically attended RSV among US adults: a systematic review and meta-analysis. Open Forum Infect Dis. 2022;9(7):300.
Rozenbaum MH, Judy J, Tran D, Yacisin K, Kurosky SK, Begier E. Low levels of RSV testing among adults hospitalized for lower respiratory tract infection in the United States. Infect Dis Ther. 2023;12(2):677–85.
Cho B-H, Weinbaum C, Tsai Y, Koppaka R. Influenza vaccine uptake and missed opportunities among the medicare-covered population with high-risk conditions during the 2018 to 2019 influenza season: a retrospective cohort study. Ann Intern Med. 2022;175(1):1–10. https://doi.org/10.7326/M21-1550.
Shi N, Palmer L, Chu B, et al. Association of RSV lower respiratory tract infection and subsequent healthcare use and costs: a Medicaid claims analysis in early-preterm, late-preterm, and full-term infants. J Med Econ. 2011;14(3):335–40.
Melgar M, Britton A, Roper LE, et al. Use of respiratory syncytial virus vaccines in older adults: recommendations of the advisory committee on immunization practices - United States, 2023. MMWR Morb Mortal Wkly Rep. 2023;72(29):793–801.
Grant LR, Slack MPE, Yan Q, et al. The epidemiologic and biologic basis for classifying older age as a high-risk, immunocompromising condition for pneumococcal vaccine policy. Expert Rev Vaccines. 2021;20(6):691–705.
Averin A, Shaff M, Weycker D, Lonshteyn A, Sato R, Pelton SI. Mortality and readmission in the year following hospitalization for pneumonia among US adults. Respir Med. 2021;185:106476. https://doi.org/10.1016/j.rmed.2021.106476.
Weycker D, Moynahan A, Silvia A, Sato R. Attributable cost of adult hospitalized pneumonia beyond the acute phase. PharmacoEcon Open. 2021;5(2):275–84. https://doi.org/10.1007/s41669-020-00240-9.
Acknowledgements
Medical Writing/Editorial Assistance: Editorial assistance was provided by Mary Cecil, who is employed by Policy Analysis Inc. (PAI). Funding was provided to PAI by Pfizer Inc.
Funding
Funding for this research (including preparation of study protocol, statistical analysis plan, and manuscript; conduct of analyses; publication fees) was provided to Policy Analysis Inc. (PAI) by Pfizer Inc.
Author information
Authors and Affiliations
Contributions
Authorship was designated based on guidelines promulgated by the International Committee of Medical Journal Editors (2004). All persons who met criteria for authorship were listed as authors on the title page. The contribution of each of these persons to this study is as follows: (1) conception and design (Ahuva Averin, Elizabeth Begier, Daniel Curcio, Bradford D. Gessner, Linnea Houde, Mark Rozenbaum, Kimberly Shea, Derek Weycker, Kari Yacisin), acquisition of data (Mark Rozenbaum, Derek Weycker), analysis or interpretation of data (all authors); and (2) preparation of manuscript (Ahuva Averin, Linnea Houde, Derek Weycker), critical review of manuscript (Elizabeth Begier, Daniel Curcio, Bradford D. Gessner, Kevin Ottino, Mark Rozenbaum, Reiko Sato, Kimberly Shea, Kari Yacisin). All authors have read and approved the final version of the manuscript. The study sponsor, Pfizer Inc., reviewed the study research plan and study manuscript; data management, processing, and analyses were conducted by PAI. All final analytic decisions and the decision to submit for publication were made solely by study investigators.
Corresponding author
Ethics declarations
Conflict of interest
Derek Weycker, Ahuva Averin, Linnea Houde, and Kevin Ottino are employees of PAI, which received funding from Pfizer for manuscript development. Kimberly Shea, Reiko Sato, Bradford D. Gessner, Kari Yacisin, Daniel Curcio, Elizabeth Begier, and Mark Rozenbaum are employed by, and hold shares of, Pfizer Inc.
Ethical Approval
The study database was de-identified prior to its release to study investigators, as set forth in the corresponding Data Use Agreement. Use of the study database for health services research was fully compliant with the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule and federal guidance on Public Welfare and the Protection of Human Subjects (45 CFR 46 §46.101). Institutional Review Board approval was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentation: This study was presented in part at IDWeek 2022, Washington, DC, USA, October 19–23, 2022 (Poster #2207). The corresponding abstract was published in Open Forum Infectious Diseases, Volume 9, Issue Supplement_2, December 2022.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Weycker, D., Averin, A., Houde, L. et al. Rates of Lower Respiratory Tract Illness in US Adults by Age and Comorbidity Profile. Infect Dis Ther 13, 207–220 (2024). https://doi.org/10.1007/s40121-023-00904-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-023-00904-z