Abstract
Introduction
Parental stress following critical illness in their child has the potential to impact functional outcomes and quality of life for the child and whole family. Parent emotional functioning may also be an important clinical target to optimize child outcomes. This study assessed the effectiveness of training programs for parents aimed at reducing adverse psychological outcomes in parents of children with acute brain injury (ABI).
Methods
We conducted searches of Embase, PubMed, Web of Science, and Cochrane Library to November 13, 2020. Randomized controlled trials (RCTs) that compared parent training programs with usual care, or an active comparator, and assessed psychological outcomes (depression, anxiety, stress) in parents of children with ABI were included. Two reviewers independently extracted data on study characteristics, participants, interventions, outcome measures, and results before and after intervention. Risk of bias was assessed using the Cochrane risk-of-bias tool.
Results
Four RCTs involving 318 parents of children with ABI were eligible for review. Compared with usual care or active comparator, parent training was associated with significant reduction in parent stress (four RCTs; standardized mean difference [SMD], − 0.32 on a numerical rating scale [95% CI, − 0.60, − 0.05]; I-squared = 7.5%, p = 0.356); significant reduction in parent depression (three RCTs; SMD, − 0.43 [95% CI, − 0.72, − 0.14]; I-squared = 0.0%, p = 0.393); and significant reduction in parent anxiety (two RCTs; SMD, − 0.63 [95% CI, − 1.05, − 0.21]; I-squared = 0.0%, p = 0.629). Overall risk of bias was high for randomization process (one RCT), missing outcome data (three RCTs), measurement of the outcome (three RCTs), and selection of reported result (two RCTs). Heterogeneity between studies by country of study origin was not significant.
Conclusions
Compared with usual care or an active comparator, parent training was associated with short-term reduction in stress, depression, and anxiety in parents of children with ABI. Future clinical trials of parent interventions are needed as there may be some short-term beneficial effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Mental health functioning of parents or family caregivers of children with acute brain injury (ABI) mediates behavioral and functional outcomes of the child and may be an important clinical target to optimize child outcomes. |
This is a systematic review and meta-analysis of randomized controlled trials (RCTs) comparing parent training programs with usual care, or active comparator, and assessing psychological outcomes (depression, anxiety, stress) in parents of children with ABI. |
In this study including four RCTs involving 318 parents of children with ABI, parent training compared with usual care or active comparator was associated with significant short-term reductions in stress, depression, and anxiety among parents of children with ABI. |
Future clinical trials of parent training programs are needed as there may be some short-term beneficial effects. |
Introduction
Acquired brain injury (ABI) in children subsumes a variety of etiologies, such as traumatic brain injury (TBI), stroke, anoxic brain injury, hydrocephalus, and central nervous system infection/inflammation. In a prospective international point prevalence study of acute neurologic diseases in 107 pediatric intensive care units (PICUs) across 23 countries and six continents, TBI was associated with the highest rate of unfavorable outcome, and stroke was associated with the second highest rate of death [1]. Parents of children with TBI experience a high burden of psychological symptoms after their child’s diagnosis [2,3,4]. Beyond the characteristics of the child and the acute neurological insult, parent stress in response to their child’s critical illness also may impact functional and behavioral outcomes and quality of life for both the child and family [5,6,7,8,9,10,11,12]. ABI is therefore a catastrophic event that can have long-term sequelae not only on the trajectory of recovery in children but also on the life and function of the child and family.
An overarching goal of care for children with ABI is to preserve their developmental status, optimize their trajectory of recovery, and maximize functional restoration of the child and family back into their communities. For the parents of such children, however, ABI may become a chronic condition that leads to ongoing emotional stress for the whole family with significant psychological and social impact [2,3,4, 13,14,15]. Elevated levels of parent stress and impaired parent psychological functioning, in turn, have been associated with adverse child outcomes [5,6,7, 16, 17]. Reducing emotional dysfunction in parents of children with ABI may be an important clinical target to optimize child and family outcomes [18].
A 2013 systematic review of parent interventions for children with TBI identified six trials investigating the impact of parent and child therapy on child and parent behavioral and emotional outcomes [19]. In this systematic review, a statistically significant intervention effect for at least one outcome measure was found in each trial, but effectiveness of parent training alone could not be determined. In addition, included studies had mixed designs (randomized controlled trials, RCTs, and observational studies), and parent outcomes were secondary endpoints. The current gap in knowledge, therefore, is that effectiveness of parent training programs alone on parent emotional functioning remains unclear. The main objective of this study was to evaluate the effectiveness of RCTs of parent training programs to reduce adverse psychological outcomes (depression, anxiety, and/or stress) in parents of children with ABI compared to active control parent programs. We hypothesized that compared with usual care or active comparator, parent training is associated with a significant reduction in measures of parent depression, anxiety, and/or stress.
Methods
We followed the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines [20]. The protocol for this review was registered on PROSPERO (ID-
CRD42020220750). This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Search Strategy
A systematic literature search was conducted in Embase, PubMed, Web of Science, and Cochrane library. There were no date restrictions. The date of the last search was November 13, 2020. The search strategy for each database can be found in Supplementary Material Table 1.
Study Selection
Two reviewers independently screened the titles and abstracts of the citations produced from the database searches for inclusion according to the eligibility criteria using Covidence (Veritas Health Innovation, Melbourne, Australia). Duplicates were removed in Covidence. The same two reviewers screened each included full-text manuscript to determine final eligibility. Two other reviewers resolved any disagreements that arose during the study inclusion process. Peer-reviewed original research was included.
Eligibility Criteria
Studies were included for full review if they met the following criteria: randomized controlled trials, systematic reviews and meta-analyses; the subjects are parents of children with ABI; the studies contained an intervention that was a parent training program (e.g., cognitive behavior therapy [CBT], parent skills coaching, positive parenting strategies, face to face therapy); the control group can be no parent training or an alternative active parent non-training program; the included outcome variables were measures of parent emotional functioning and included depression, anxiety, and stress. Studies were excluded if they met the following criteria: abstracts, letters to the editor, and conference proceedings; cost-effectiveness studies; cross-sectional studies; case–control studies and nested case control studies; prospective and retrospective cohort studies and case-cohort studies. To isolate effects of parent training on parent functioning, studies were also excluded if they included children with the parents in the intervention, even if there was a parent training component. The reference lists of included studies were also manually checked for relevant studies. We did not include date restrictions.
Data Collection
Data was extracted by three independent reviewers. Microsoft Excel was used to organize and record numerical data of outcome variables. Data items included first author, year, country, trial design, number and characteristics of participants, type and characteristics of intervention and control treatment, outcome measures, and results. We attempted to reduce heterogeneity of ABI by limiting our search strategy to traumatic brain injury and stroke etiologies (see Supplementary Material Table 1) since these are globally among the most frequent types of ABI that are associated with the highest rates of death and unfavorable outcomes in children [1]. Two intervention groups (I-InTERACT and I-InTERACT-Express) in one RCT [21] were combined for statistical analyses since both interventions used the same two-stage framework with web content and videoconferencing for live coaching, and they only differed by the omission of supplemental sessions in I-InTERACT-Express. Outcomes data from primary analyses (reported as intention-to-treat in three RCTs [21,22,23]) were extracted in all RCTs. Discrepancies between the reviewers were rechecked and discussed until consensus was reached.
Risk of Bias (Quality Assessment)
Risk of bias in individual studies was assessed independently by two reviewers using the Cochrane risk-of-bias tool (RoB 2 version). This tool assesses risk of bias in the following five domains: randomization process, deviation from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported results. Any discrepancies were rechecked by the other two reviewers, and were discussed until consensus was achieved. We were unable to assess for publication bias by visually inspecting funnel plots because of the small number of eligible trials [24].
Data Synthesis
Meta-analyses were conducted if at least two RCTs had sufficient clinical and statistical homogeneity for at least one outcome of interest. Outcomes data was extracted from the immediate post-intervention period for two RCTs [22, 23], at 6 months follow-up for one RCT [21], and at 18–36 weeks follow-up in one RCT [25]. A summary of the outcome measures of interest in each study, and the characteristics of each instrument are shown in Table 1. Since outcomes were measured by different scales (e.g., different instruments for depression, anxiety, and stress), standardized mean differences (SMDs) and their 95% confidence intervals were used. For all outcome measures, negative SMD indicated a beneficial effect of the intervention when compared to the control group. Random-effects meta-analyses were performed using the metan package in Stata (Version 16.1). Forest plot was used to visualize the point estimates of study effects and their confidence intervals. Z-test was performed to test whether a summary effect was zero or not. P values less than 0.05 were considered statistically significant. Fixed-effects meta-analyses were performed as sensitivity analysis.
Assessment of Heterogeneity Across Studies
The Q-statistic was derived, and its chi-squared test was conducted for testing between-study heterogeneity in effect sizes. A P value less than 0.10 indicated significant heterogeneity. Heterogeneity in effect sizes between studies was explored using I-squared (I2) statistics. I2 values less than 25%, greater than 25%, greater than 50%, and greater than 75% indicate low, moderate, substantial, and considerable heterogeneity, respectively [26]. Meta-regression was used to test whether there was any between-study variation in outcomes due to country stratified by USA vs. not USA.
Results
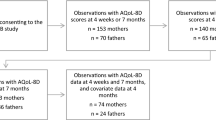
The database search originally yielded 509 potential references. After de-duplication, a total of 488 articles were screened, and 28 of these articles were eligible for full text review. Of these 28 papers, four RCTs [21,22,23, 25] that included a total of 318 parents of children with ABI met inclusion/exclusion criteria, and were eligible for both qualitative and quantitative analyses (Fig. 1).
Study Characteristics
Table 2 presents the characteristics of the included studies. Two RCTs were conducted in the USA [21, 25], one RCT in Mexico [22], and one RCT in Australia [23]. Three RCTs were registered in a clinical trials database (Universal Trial Number U1111-1193689 [22], Clinicaltrials.gov NCT 01214694 [21], and Australian New Zealand Clinical Trials Registry ACTRN12610001051033 [23]). The study recruitment periods were reported for three RCTs (2010 to 2015 [21], March 2016 to May 2017 [22], and October 2010 to May 2012 [23]), and were not reported in one RCT [25]. Study participants were recruited from four large children’s hospitals and one general hospital (all level 1 trauma centers) in four major US cities [21]; a trauma registry of an urban US children’s hospital [25]; via posters/flyers at local hospitals, universities, and one of the venues of Iskalti Centre of Psychological and Educational Support in Mexico [22]; and through two pediatric rehabilitation services in Australia [23]. The number of subjects who declined study participation was reported in three RCTs, and was 43% (37/87 subjects contacted) [25], 55% (140/257 subjects contacted) [21], and 72% (151/210 contacted) [23]; refusal rate was not reported in one RCT [22]. Reasons subjects refused to participate in the studies were too busy, not interested in the program, taking part in other treatments, had childcare problems, could not attend meeting times/locations, group sessions too far away, no longer experiencing concerns related to the Injury, and no reason given.
The type of ABI in children included tumor, cyst, infection, TBI, TBI and cyst, vascular lesion, and atrophy of unknown cause [22]; moderate to severe TBI defined as Glasgow Coma Scale (GCS) score of 8 or less (severe TBI), and GCS score of 9–12 or 13–15 with evidence of trauma-related abnormalities on imaging (moderate TBI) [21, 25]; and TBI (mild, moderate, severe), cardiovascular accident, hypoxia, brain tumor, and encephalitis/meningitis [23]. The time to intervention since ABI in all four RCTs was 3.13 ± 2.62 months [23], 3.5 ± 2.2 years [22], 1.02 ± 1.52 years [21], and 13.48 ± 6.86 months [25]. No significant between-group baseline differences in type of ABI and time to intervention were found after randomization in all four RCTs.
Intervention Characteristics
All four RCTs differed in regard to the type and duration of parent intervention. A group-based cognitive behavior therapy (CBT) approach to reduce dysfunctional parenting practices (six sessions per week, 2.5 h per session) was provided in one RCT [22]. On-line family therapy that included 14 separate self-guided sessions with didactic content (e.g., problem-solving skills), videos of parents modeling skills, and practice exercises for families followed by synchronous videoconference meetings with a therapist to review family exercises and implement the problem-solving process was administered in one RCT [25]. A web-based parenting intervention that provided web content and live coaching of parenting skills and positive parenting strategies (seven sessions or 10–14 sessions) was provided in one RCT [21]. Group-based family behavioral therapy (nine sessions—16 h of group sessions, 1.5 h individual telephone support over 10 weeks) combined with CBT (two sessions) for treating psychological distress in parents was provided in one RCT [23]. Interventions were administered by psychologists with masters or doctoral degrees in clinical psychology, or postgraduate clinical psychology students in all four RCTs.
Characteristics of Outcome Measures
Parent outcomes assessed were depression in three RCTs [21, 23, 25], stress in four RCTs [21,22,23, 25], and anxiety in two RCTs [23, 25]. Parent outcomes were primary study endpoints in two RCTs [21, 25], and secondary endpoints in two RCTs [22, 23]. The number of participants with outcomes analyzed were 73% (22/30 subjects randomized) [23], 90% (70/78 subjects) [21], 71% (25/35 subjects) [22], and 77% (20/26 subjects) [25]. For the three RCTs with a specified follow-up time period, treatment effects on parent stress were not maintained in two RCTs at 3 months [22] and 6 months [21], but were maintained in one RCT at 6 months [23]. Treatment effects on parent depression were maintained at 6 months in two RCTs [21, 23]. Treatment effects on parent anxiety were maintained in one RCT at 6 months [23].
Risk of Bias
The risk of bias for each study is shown in Fig. 2. Study participants and investigators were blinded to treatment allocation and outcomes in one RCT [22], and neither was blinded to treatment allocation or outcomes in three RCTs [21, 23, 25]. Attrition rates at the time of outcomes analysis in this study were 23% [25], 27% [23], 29% [22], and 10% [21]. Pre-specified statistical plans were not reported or published prior to randomization in all four RCTs [21,22,23, 25]. Using these criteria, the overall risk of bias was high in all four RCTs [21,22,23, 25].
Meta-Analysis
Four RCTs were included in the meta-analysis. Figure 3 shows the results of meta-analyses using random effects for the effects of parent interventions on parent stress, depression, and anxiety. Compared with usual care or an active comparator, parent training was associated with a significant reduction in parent stress [four RCTs; standardized mean difference [SMD], − 0.32 on a numerical rating scale (95% CI, − 0.6, − 0.05), z = 2.31, p = 0.021; heterogeneity chi-squared = 3.24 (d.f. = 3); p = 0.356; I2 = 7.5%]; significant reduction in parent depression [three RCTs; SMD, − 0.43 (95% CI, − 0.72, − 0.14), z = 2.88, p = 0.004; heterogeneity chi-squared = 1.87 (d.f. = 2); p = 0.393; I2 = 0.0%]; and a significant reduction in parent anxiety [two RCTs; SMD, − 0.63 (95% CI, − 1.05, − 0.21), z = 2.96, p = 0.003; heterogeneity chi-squared = 0.23 (d.f. = 1); p = 0.629; I2 = 0.0%]. In the meta-analysis, P values for testing between-study heterogeneity were all greater than 0.1, indicating that the studies were not heterogeneous in effect sizes. Additionally, the derived I-squared statistics were all less than 10%, indicating that heterogeneity in effect sizes of the studies was very low. Sensitivity analyses using fixed effects showed that compared with usual care or an active comparator, there was no change in the effect size estimates or confidence intervals and a significant reduction was again noted for parent stress, depression, and anxiety (Supplementary Material Fig. 1). Subgroup analysis between all four RCTs by country of study origin (USA vs. not USA) was not significant in meta-regression (beta coefficient = 0.28, (95% CI, − 0.94, 1.5), p = 0.426).
Discussion
In this systematic review and meta-analysis, we found that parent focused interventions (e.g., traditional group-based CBT, behavioral therapy, and on-line problem-solving interventions with live coaching or synchronous therapy) are associated with significant short-term reduction in stress, depression, and anxiety in parents of children with ABI when compared to usual care or an active comparator. The results, however, are based on four small RCTs with high risk of bias, missing data from high participant refusal and attrition rates, and variability in study demographics, interventions, control groups, and outcome measures. Accordingly, we failed to find evidence of long-term benefit (or harm) associated with these parent interventions, but there may be some short-term beneficial effects.
Given the bidirectional relationship between parent and child functioning following ABI [10], interventions targeting parent emotional functioning may be as important as those targeting child functioning after ABI. The effectiveness of parent focused therapy on emotional functioning in parents could not be determined in the prior systematic review by Brown and colleagues in 2013 [19]. In our meta-analysis, the pooled estimates show a beneficial effect of parent-directed therapies on parent stress, depression, and anxiety in the short-term. These studies may provide a useful framework for future research of parent interventions that aim to reduce psychological symptoms in parents, thereby reducing or preventing emotional and behavioral difficulties in their children with ABI [27], and improving the family environment for pediatric survivors with ABI.
The results from individual studies, however, were limited by wide confidence intervals, and high rates of study refusal ranging from 43% to 72% [21, 23, 25]. Parent stress is moderated by socioeconomic status and social support [9]. Accordingly, the families who refused participation in these studies may have different resources and demands, which are important to understand in order to develop effective rehabilitation programs that aim to improve the family environment and overall well-being of parents and children with ABI. The overall risk of bias was high in all included RCTs in the domains of randomization process [25], missing outcome data [22, 23, 25], measurement of the outcome [21, 23, 25], and selection of reported result [22, 23]. The average time to intervention across all four RCTs was 13.5 to 17 weeks. Some critical gaps remaining that could be investigated in future research are improving recognition of mental health disorders in parents through the use of screening tools, and better understanding social determinants of health, accessibility to parent interventions, impact of more timely parent interventions on child and family outcomes, and retention of long-term effects of parent interventions on parent psychological and family functioning.
This meta-analysis has several strengths. We included only RCTs with comparator groups. This study is novel as the first meta-analysis to quantify the association between parent interventions and parent outcomes. Given the bidirectional relationship between parent and child functioning following ABI [10], the results suggest that parent training is feasible and may reduce depression, stress, and anxiety in some parents. Accordingly, this study provides a foundational framework for future research in rehabilitation strategies for parents and children in the recovery phase following ABI.
Study Limitations
Our systematic review and meta-analysis has certain limitations. The number of eligible RCTs was limited. Parent outcomes were not the primary study endpoint in two RCTs [22, 23]. This could induce an underpowered investigation of these parent outcomes, and consequently introduce variations on our meta-analysis results. In addition, the parent outcome measures in all four selected studies rely on self-report, and a large proportion of eligible subjects contacted declined participation in the majority of RCTs, which could result in selection bias. This could also lead to differential misclassification bias. The four trials varied in patient baseline emotional status of parents, parent demographics such as race and region, the severity of ABI, baseline functional status of the children, interventions (program type, duration, frequency of sessions), comparison group, outcome measure, and time to follow-up assessment. All of these aspects in the four RCTs were considered factors that induce an overall high risk of bias in the meta-analysis. Other limitations arise from the small number of RCTs we identified for the meta-analysis. This circumstance prohibits us from conducting meta-regression and subgroup analysis and assessing for publication bias. Given the small number of RCTs, the reliability of the analysis performed using random-effects models can also be challenged. Because of this concern, we reported the analysis results from both random-effects and fixed-effects models for sensitivity analysis in this study.
Conclusions
This meta-analysis found that parent training may be associated with short-term reduction in stress, depression, and anxiety in parents of children with ABI compared to an active comparator or usual care. Future randomized prospective clinical trials with readily accessible, timely, and longer-term follow-up of parent interventions are needed to develop and plan rehabilitation strategies that incorporate parent emotional well-being into rehabilitation strategies involving children recovering from ABI.
References
Fink EL, Kochanek PM, Tasker RC, et al. International survey of critically ill children with acute neurologic insults: the prevalence of acute critical neurological disease in children: a global epidemiological assessment study. Pediatr Crit Care Med. 2017;18(4):330–42. https://doi.org/10.1097/PCC.0000000000001093.
Verhaeghe S, Defloor T, Grypdonck M. Stress and coping among families of patients with traumatic brain injury: a review of the literature. J Clin Nurs. 2005;14(8):1004–12. https://doi.org/10.1111/j.1365-2702.2005.01126.x.
Wade SL, Taylor HG, Drotar D, Stancin T, Yeates KO, Minich NM. A prospective study of long-term caregiver and family adaptation following brain injury in children. J Head Trauma Rehabil. 2002;17(2):96–111. https://doi.org/10.1097/00001199-200204000-00003.
Stancin T, Wade SL, Walz NC, Yeates KO, Taylor HG. Traumatic brain injuries in early childhood: initial impact on the family. J Dev Behav Pediatr. 2008;29(4):253–61. https://doi.org/10.1097/DBP.0b013e31816b6b0f.
Anderson VA, Catroppa C, Dudgeon P, Morse SA, Haritou F, Rosenfeld JV. Understanding predictors of functional recovery and outcome 30 months following early childhood head injury. Neuropsychology. 2006;20(1):42–57. https://doi.org/10.1037/0894-4105.20.1.42.
Li L, Liu J. The effect of pediatric traumatic brain injury on behavioral outcomes: a systematic review. Dev Med Child Neurol. 2013;55(1):37–45. https://doi.org/10.1111/j.1469-8749.2012.04414.x.
Yeates KO, Swift E, Taylor HG, et al. Short- and long-term social outcomes following pediatric traumatic brain injury. J Int Neuropsychol Soc. 2004;10(3):412–26. https://doi.org/10.1017/S1355617704103093.
Raj SP, Wade SL, Cassedy A, et al. Parent psychological functioning and communication predict externalizing behavior problems after pediatric traumatic brain injury. J Pediatr Psychol. 2014;39(1):84–95. https://doi.org/10.1093/jpepsy/jst075.
Schwartz L, Taylor HG, Drotar D, Yeates KO, Wade SL, Stancin T. Long-term behavior problems following pediatric traumatic brain injury: prevalence, predictors, and correlates. J Pediatr Psychol. 2003;28(4):251–63. https://doi.org/10.1093/jpepsy/jsg013.
Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Burant C. Bidirectional child-family influences on outcomes of traumatic brain injury in children. J Int Neuropsychol Soc. 2001;7(6):755–67. https://doi.org/10.1017/s1355617701766118.
Gerrard-Morris A, Taylor HG, Yeates KO, et al. Cognitive development after traumatic brain injury in young children. J Int Neuropsychol Soc. 2010;16(1):157–68. https://doi.org/10.1017/S1355617709991135.
Wade SL, Cassedy A, Walz NC, Taylor HG, Stancin T, Yeates KO. The relationship of parental warm responsiveness and negativity to emerging behavior problems following traumatic brain injury in young children. Dev Psychol. 2011;47(1):119–33. https://doi.org/10.1037/a0021028.
Anderson VA, Catroppa C, Haritou F, Morse S, Rosenfeld JV. Identifying factors contributing to child and family outcome 30 months after traumatic brain injury in children. J Neurol Neurosurg Psychiatry. 2005;76(3):401–8. https://doi.org/10.1136/jnnp.2003.019174.
Wade SL, Gerry Taylor H, Yeates KO, et al. Long-term parental and family adaptation following pediatric brain injury. J Pediatr Psychol. 2006;31(10):1072–83. https://doi.org/10.1093/jpepsy/jsj077.
Williams CN, Eriksson C, Piantino J, et al. Long-term sequelae of pediatric neurocritical care: the parent perspective. J Pediatr Intensive Care. 2018;7(4):173–81. https://doi.org/10.1055/s-0038-1637005.
Prinzie P, Stams GJ, Dekovic M, Reijntjes AH, Belsky J. The relations between parents’ Big Five personality factors and parenting: a meta-analytic review. J Pers Soc Psychol. 2009;97(2):351–62. https://doi.org/10.1037/a0015823.
Bernier A, Carlson SM, Whipple N. From external regulation to self-regulation: early parenting precursors of young children’s executive functioning. Child Dev. 2010;81(1):326–39. https://doi.org/10.1111/j.1467-8624.2009.01397.x.
Jarvis JM, Choong K, Khetani MA. Associations of participation-focused strategies and rehabilitation service use with caregiver stress after pediatric critical illness. Arch Phys Med Rehabil. 2019;100(4):703–10. https://doi.org/10.1016/j.apmr.2018.11.017.
Brown FL, Whittingham K, Boyd R, Sofronoff K. A systematic review of parenting interventions for traumatic brain injury: child and parent outcomes. J Head Trauma Rehabil. 2013;28(5):349–60. https://doi.org/10.1097/HTR.0b013e318245fed5.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009. https://doi.org/10.1371/journal.pmed.1000097.
Raj SP, Shultz EL, Zang H, et al. Effects of web-based parent training on caregiver functioning following pediatric traumatic brain injury: a randomized control trial. J Head Trauma Rehabil. 2018;33(6):E19–29. https://doi.org/10.1097/HTR.0000000000000388.
Chavez Arana C, Catroppa C, Yanez-Tellez G, et al. A parenting program to reduce disruptive behavior in hispanic children with acquired brain injury: a randomized controlled trial conducted in Mexico. Dev Neurorehabil. 2020;23(4):218–30. https://doi.org/10.1080/17518423.2019.1645224.
Brown FL, Whittingham K, Boyd RN, McKinlay L, Sofronoff K. Does Stepping stones triple P plus acceptance and commitment therapy improve parent, couple, and family adjustment following paediatric acquired brain injury? A randomised controlled trial. Behav Res Ther. 2015;73:58–66. https://doi.org/10.1016/j.brat.2015.07.001.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. https://doi.org/10.1136/bmj.315.7109.629.
Wade SL, Carey J, Wolfe CR. An online family intervention to reduce parental distress following pediatric brain injury. J Consult Clin Psychol. 2006;74(3):445–54. https://doi.org/10.1037/0022-006X.74.3.445.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557.
Sanders MR. Triple P-Positive Parenting Program: towards an empirically validated multilevel parenting and family support strategy for the prevention of behavior and emotional problems in children. Clin Child Fam Psychol Rev. 1999;2(2):71–90. https://doi.org/10.1023/a:1021843613840.
Acknowledgements
Funding
There was no funding source or sponsorship for this project. The Senior Department of Pediatrics, the Seventh Medical Center of PLA General Hospital reimbursed the Rapid Service Fee of this article.
Author Contributions
Dr. LaRovere designed and conceptualized the study, and drafted the initial manuscript for intellectual content. Drs. LaRovere, Tang, Li, and Wadhwani had major roles in data acquisition. All authors analyzed and interpreted the data, and revised the manuscript for intellectual content.
Disclosures
Dr. Robert C. Tasker has received royalties or licenses from Oxford Handbook of Paediatrics 3e (2021) and Up-to-Date. Dr. Tasker has received payment or honoraria as the Editor-in-Chief of Pediatric Critical Care Medicine and Associate Editor of Archives of Disease in Childhood. Dr. Robert C. Tasker is the Trial Steering Committee Chair for two contemporary randomized controlled trials (Oxy-PICU and PRESSURE). Each of the remaining authors (Drs. Kerri LaRovere, Yuzhe Tang, Kun Li, Nikita Wadhwani, Bo Zhang and Guang Yang) has nothing to disclose. This material has not been presented publicly.
Compliance with Ethics Guidelines
Ethics committee approval was not required for this systematic review of the published literature. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding authors on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
LaRovere, K.L., Tang, Y., Li, K. et al. Effectiveness of Training Programs for Reducing Adverse Psychological Outcomes in Parents of Children with Acquired Brain Injury: A Systematic Review and Meta-Analysis. Neurol Ther 11, 1691–1704 (2022). https://doi.org/10.1007/s40120-022-00399-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-022-00399-9