Abstract
Purpose
We aimed to explore the clinical characteristics of Campylobacter bacteraemia and identify the trends, risk factors for mortality, and antimicrobial susceptibility patterns from clinical samples.
Methods
This retrospective cohort study included patients confirmed to have Campylobacter bacteraemia from seven hospitals between January 2010 and June 2021. Data on demographics and underlying history, clinical manifestation, and antimicrobial susceptibility patterns were collected and analyzed. Annual cases of Campylobacter enteritis were extracted from a public database.
Results
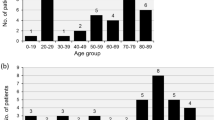
A total of 108 patients were included, and five species were isolated. Campylobacter jejuni accounted for 54 (50.0%) cases and 17 (16%) patients had no symptoms other than fever. In-hospital mortality occurred in 14 (13.0%) patients. C. jejuni bacteraemia was associated with lower mortality compared to non-C. jejuni bacteraemia. Underlying cancer and septic shock were the significant factors associated with in-hospital mortality. Quinolone resistance was high (59%), whereas only 4% of isolates exhibited macrolide resistance. There has been a significant increase in the number of Campylobacter enteritis cases, which was strongly correlated with the number of Campylobacter bacteraemia cases (Pearson’s coefficient: 0.953; p < 0.0001).
Conclusion
The notably increasing incidence of Campylobacter bacteraemia and antibiotic resistance patterns can challenge the treatment, necessitating collective efforts of national surveillance and networks by many departments.


Similar content being viewed by others
Data availability
The data analysed during the current study is available from the corresponding author on reasonable request.
References
WHO. Campylobacter, https://www.who.int/news-room/fact-sheets/detail/campylobacter. Accessed 20 Jul 2023.
CDC Foodborne Disease Active Surveillance Network (FoodNet), https://wwwn.cdc.gov/foodnetfast/ Accessed 20 Jul 2023.
Ray LCCJ, Griffin PM. Decreased incidence of infections caused by pathogens transmitted commonly through food during the COVID-19 pandemic—foodborne diseases active surveillance network, 10 US Sites, 2017–2020. MMWR Morb Mortal Wkly Rep. 2021;70:1332–6. https://doi.org/10.15585/mmwr.mm7038a4.
de Miguel BR, Trigo E, De La Calle-Prieto F, Arsuaga M, Díaz-Menéndez M. Social distancing to combat COVID-19 led to a marked decrease in food-borne infections and sexually transmitted diseases in Spain. J Travel Med. 2020;27:taaa134. https://doi.org/10.1093/jtm/taaa134.
Ahn SY, Park JY, Lim IS, Chae SA, Yun SW, Lee NM, et al. Changes in the occurrence of gastrointestinal infections after COVID-19 in Korea. J Korean Med Sci. 2021. https://doi.org/10.3346/jkms.2021.36.e180.
Nielsen H, Hansen KK, Gradel KO, Kristensen B, Ejlertsen T, Østergaard C, et al. Bacteraemia as a result of Campylobacter species: a population-based study of epidemiology and clinical risk factors. Clin Microbiol Infect. 2010;16:57–61. https://doi.org/10.1111/j.1469-0691.2009.02900.x.
Alfredson DA, Korolik V. Antibiotic resistance and resistance mechanisms in Campylobacter jejuni and Campylobacter coli. FEMS Microbiol Lett. 2007;277:123–32. https://doi.org/10.1111/j.1574-6968.2007.00935.x.
Kim YJ, Park KH, Park DA, Park J, Bang BW, Lee SS, et al. Guideline for the antibiotic use in acute gastroenteritis. Infect Chemother. 2019;51:217–43. https://doi.org/10.3947/ic.2019.51.2.217.
Post A, Martiny D, van Waterschoot N, Hallin M, Maniewski U, Bottieau E, et al. Antibiotic susceptibility profiles among Campylobacter isolates obtained from international travelers between 2007 and 2014. Eur J Clin Microbiol Infect Dis. 2017;36:2101–7.
HIRA, https://opendata.hira.or.kr/op/opc/olap4thDsInfoTab1.do Accessed 20 Jul 2023.
The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. Version 12.0, 2022.
Costa D, Iraola G. Pathogenomics of emerging Campylobacter Species. Clin Microbiol Rev. 2019;32:e00072-e118. https://doi.org/10.1128/CMR.00072-18.
Dearlove BL, Cody AJ, Pascoe B, Méric G, Wilson DJ, Sheppard SK. Rapid host switching in generalist Campylobacter strains erodes the signal for tracing human infections. ISME J. 2016;10:721–9. https://doi.org/10.1038/ismej.2015.149.
Liu F, Ma R, Wang Y, Zhang L. The clinical importance of campylobacter concisus and other human hosted Campylobacter species. Front Cell Infect Microbiol. 2018;8:243. https://doi.org/10.3389/fcimb.2018.00243.
Liao CH, Chuang CY, Huang YT, Lee PI, Hsueh PR. Bacteremia caused by antimicrobial resistant Campylobacter species at a medical center in Taiwan, 1998–2008. J Infect. 2012;65(5):392–9. https://doi.org/10.1016/j.jinf.2012.06.014.
Pacanowski J, Lalande V, Lacombe K, Boudraa C, Lesprit P, Legrand P, et al. Campylobacter bacteremia: clinical features and factors associated with fatal outcome. Clin Infect Dis. 2008;47:790–6. https://doi.org/10.1086/591530.
Tinévez C, Velardo F, Ranc AG, Dubois D, Pailhoriès H, Codde C, et al. Retrospective multicentric study on Campylobacter spp. Bacteremia in France: the Campylobacteremia study. Clin Infect Dis. 2022;75:702–9. https://doi.org/10.1093/cid/ciab983.
Francois Watkins LK, Laughlin ME, Joseph LA, Chen JC, Nichols M, Basler C, et al. Ongoing outbreak of extensively drug-resistant Campylobacter jejuni infections associated with US pet store puppies, 2016–2020. JAMA Netw Open. 2021;4:e2125203. https://doi.org/10.1001/jamanetworkopen.2021.25203.
Kuhn KG, Nygård KM, Guzman-Herrador B, Sunde LS, Rimhanen-Finne R, Trönnberg L, et al. Campylobacter infections expected to increase due to climate change in Northern Europe. Sci Rep. 2020;10:13874. https://doi.org/10.1038/s41598-020-70593-y.
Ravel A, Pintar K, Nesbitt A, Pollari F. Non food-related risk factors of campylobacteriosis in Canada: a matched case-control study. BMC Public Health. 2016;16:1016. https://doi.org/10.1186/s12889-016-3679-4.
Cho H, Lee SH, Lee JH, Lee SJ, Park SC. Epidemiologic and clinical features of Campylobacter enteritis before and during COVID-19 in Korea. J Korean Med Sci. 2023;38: e67. https://doi.org/10.3346/jkms.2023.38.e67.
Ternhag A, Asikainen T, Giesecke J, Ekdahl K. A meta-analysis on the effects of antibiotic treatment on duration of symptoms caused by infection with Campylobacter species. Clin Infect Dis. 2007;44:696–700. https://doi.org/10.1086/509924.
Yoon JG, Lee SN, Hyun HJ, Choi MJ, Jeon JH, Jung E, et al. Campylobacter jejuni Bacteremia in a liver cirrhosis patient and review of literature: a case study. Infect Chemother. 2017;49:230–5. https://doi.org/10.3947/ic.2017.49.3.230.
Park SH, Kim BJ, Kwon YH, Hwang IY, Sung GH, Park EH, et al. Antimicrobial susceptibility and genetic analysis of Campylobacter jejuni isolated from diarrhea patients in Busan. Ann Clin Microbiol. 2019;22(2):42–9. https://doi.org/10.5145/ACM.2019.22.2.42.
Gahamanyi N, Song DG, Yoon KY, Mboera LEG, Matee MI, Mutangana D, et al. Antimicrobial resistance profiles, virulence genes, and genetic diversity of thermophilic Campylobacter species isolated from a layer poultry farm in Korea. Front Microbiol. 2021;12: 622275. https://doi.org/10.3389/fmicb.2021.622275.
Oh JY, Kwon YK, Wei B, Jang HK, Lim SK, Kim CH, et al. Epidemiological relationships of Campylobacter jejuni strains isolated from humans and chickens in South Korea. J Microbiol. 2017;55:13–20. https://doi.org/10.1007/s12275-017-6308-8.
Khademi F, Sahebkar A. Prevalence of fluoroquinolone-resistant campylobacter species in Iran: a systematic review and meta-analysis. Int J Microbiol. 2020;2020:8868197. https://doi.org/10.1155/2020/8868197.
The European Union Summary Report on Antimicrobial Resistance in zoonotic and indicator bacteria from humans, animals and food in 2019–2020. EFSA J. 2022;20:e07209. https://doi.org/10.2903/j.efsa.2022.7209.
Park M, Kim J, Feinstein J, Lang KS, Ryu S, Jeon B. Development of fluoroquinolone resistance through antibiotic tolerance in Campylobacter jejuni. Microbiol Spectr. 2022;10: e0166722. https://doi.org/10.1128/spectrum.01667-22.
Goyal D, Watkins LKF, Montgomery MP, Jones SMB, Caidi H, Friedman CR. Antimicrobial susceptibility testing and successful treatment of hospitalised patients with extensively drug-resistant Campylobacter jejuni infections linked to a pet store puppy outbreak. J Glob Antimicrob Resist. 2021;26:84–90. https://doi.org/10.1016/j.jgar.2021.04.029.
Heimesaat MM, Backert S, Alter T, Bereswill S. Human Campylobacteriosis—a serious infectious threat in a one health perspective. Curr Top Microbiol Immunol. 2021;431:1–23. https://doi.org/10.1007/978-3-030-65481-8_1.
Acknowledgements
We are grateful to the health and agriculture sector workers and health authorities striving to improve public health.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
YJB conceptualized the research question, collected data, conducted the analysis, and drafted the initial manuscript. JES, EJK, HC, YS, YDJ, and EHL collected data and carried out the data analysis. JYA, SJJ, NSK, JYC, J-SY, and YGS provided feedback on the research design and analysis. JHK contributed to conceiving the ideas, supervising the study, and reviewing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The study protocol was approved by the Ethics Review Committee of Severance Hospital (approval no. 4-2021-1796). The requirement for informed consent was waived owing to the retrospective nature of the study.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Baek, Y.J., Song, J.E., Kim, E.J. et al. Trends, clinical characteristics, antimicrobial susceptibility patterns, and outcomes of Campylobacter bacteraemia: a multicentre retrospective study. Infection (2023). https://doi.org/10.1007/s15010-023-02118-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s15010-023-02118-4