Abstract
Purpose
The aim of this study was to evaluate the effectiveness of ceftolozane/tazobactam (C/T) for treating extensively drug-resistant Pseudomonas aeruginosa (XDR-PA) infections, and to analyze whether high C/T dosing (2 g ceftolozane and 1 g tazobactam every 8 h) and infection source control have an impact on outcome.
Methods
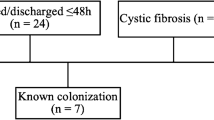
Retrospective study of all consecutive patients treated with C/T for XDR-PA infection at a tertiary referral hospital (November 2015–July 2017). Main clinical and microbiological variables were analyzed.
Results
Thirty-eight patients were included. Median age was 59.5 years and Charlson Comorbidity Index was 3.5. Fourteen (36.8%) patients had respiratory tract infection, six (15.8%) soft tissue, and six (15.8%) urinary tract infection. Twenty-three (60.5%) received high-dose C/T and in 24 (63.2%) C/T was combined with other antibiotics. At completion of treatment, 33 (86.8%) patients showed clinical response. At 90 days of follow-up, 26 (68.4%) achieved clinical cure, and 12 (31.6%) had clinical failure because of persistent infection in one patient, death attributable to the XDR-PA infection in four, and clinical recurrence in seven. All-cause mortality was 5 (13.2%). Lower C/T MIC and adequate infection source control were the only variables significantly associated with clinical cure.
Conclusions
C/T should be considered for treating XDR-PA infections, with infection source control being an important factor to avoid failure and resistance.

Similar content being viewed by others
References
Sader HS, Farrell DJ, Castanheira M, Flamm RK, Jones RN. Antimicrobial activity of ceftolozane/tazobactam tested against Pseudomonas aeruginosa and Enterobacteriaceae with various resistance patterns isolated in European hospitals (2011–2012). J Antimicrob Chemother. 2014;1:2713–22. https://doi.org/10.1093/jac/dku184.
Farrell DJ, Flamm RK, Sader HS, Jones RN. Antimicrobial activity of ceftolozane–tazobactam tested against Enterobacteriaceae and Pseudomonas aeruginosa with various resistance patterns isolated in US hospitals (2011–2012). Antimicrob Agents Chemother. 2013;1:6305–10. https://doi.org/10.1128/AAC.01802-13.
Liscio JL, Mahoney MV, Hirsch EB. Ceftolozane/tazobactam and ceftazidime/avibactam: two novel β-lactam/β-lactamase inhibitor combination agents for the treatment of resistant Gram-negative bacterial infections. Int J Antimicrob Agents. 2015;46:266–71. https://doi.org/10.1016/j.ijantimicag.2015.05.003.
Munita JM, Aitken SL, Miller WR, Perez F, Rosa R, Shimose LA, et al. Multicenter evaluation of ceftolozane/tazobactam for serious infections caused by carbapenem-resistant Pseudomonas aeruginosa. Clin Infect Dis. 2017;65:158–61. https://doi.org/10.1093/cid/cix014.
Peghin M, Maiani M, Castaldo N, Givone F, Righi E, Lechiancole A, et al. Ceftolozane/tazobactam for the treatment of MDR Pseudomonas aeruginosa left ventricular assist device infection as a bridge to heart transplant. Infection. 2017. https://doi.org/10.1007/s15010-017-1086-0.
Dinh A, Wyplosz B, Kernéis S, Lebeaux D, Bouchand F, Duran C, et al. Use of ceftolozane/tazobactam as salvage therapy for infections due to extensively drug-resistant Pseudomonas aeruginosa. Int J Antimicrob Agents. 2017;49:782–3. https://doi.org/10.1016/j.ijantimicag.2017.04.001.
Castón JJ, De la Torre Á, Ruiz-Camps I, Sorlí ML, Torres V, Torre-Cisneros J. Salvage therapy with ceftolozane–tazobactam for multidrug-resistant Pseudomonas aeruginosa infections. Antimicrob Agents Chemother. 2017;61:e02136-16. https://doi.org/10.1128/AAC.02136-16.
Sousa Dominguez A, Perez-Rodríguez MT, Nodar A, Martinez-Lamas L, Perez-Landeiro A, Crespo Casal M. Successful treatment of MDR Pseudomonas aeruginosa skin and soft-tissue infection with ceftolozane/tazobactam. J Antimicrob Chemother. 2017;72:1262–3. https://doi.org/10.1093/jac/dkw526.
Hernández-Tejedor A, Merino-Vega CD, Martín-Vivas A, Ruiz de Luna-González R, Delgado-Iribarren A, Gabán-Díez Á, et al. Successful treatment of multidrug-resistant Pseudomonas aeruginosa breakthrough bacteremia with ceftolozane/tazobactam. Infection. 2017;45:115–7. https://doi.org/10.1007/s15010-016-0944-5.
Haidar G, Philips NJ, Shields RK, Snyder D, Cheng S, Potoski BA, et al. Ceftolozane–tazobactam for the treatment of multidrug-resistant Pseudomonas aeruginosa infections: clinical effectiveness and evolution of resistance. Clin Infect Dis. 2017;65:110–20. https://doi.org/10.1093/cid/cix182.
Kuti JL, Ghazi IM, Quintiliani R, Shore E, Nicolau DP. Treatment of multidrug-resistant Pseudomonas aeruginosa with ceftolozane/tazobactam in a critically ill patient receiving continuous venovenous haemodiafiltration. Int J Antimicrob Agents. 2016;48:342–3. https://doi.org/10.1016/j.ijantimicag.2016.06.00512.
Vickery SB, McClain D, Wargo KA. Successful Use of Ceftolozane–tazobactam to treat a pulmonary exacerbation of cystic fibrosis caused by multidrug-resistant Pseudomonas aeruginosa. Pharmacother J Hum Pharmacol Drug Ther. 2016;36:e154–9. https://doi.org/10.1002/phar.1825.
Xiao AJ, Miller BW, Huntington JA, Nicolau DP. Ceftolozane/tazobactam pharmacokinetic/pharmacodynamic-derived dose justification for phase 3 studies in patients with nosocomial pneumonia. J Clin Pharmacol. 2016;56:56–66. https://doi.org/10.1002/jcph.5666.
Gelfand MS, Cleveland KO. Ceftolozane/tazobactam therapy of respiratory infections due to multidrug-resistant Pseudomonas aeruginosa. Clin Infect Dis. 2015;61:853–5.
Magiorakos A-P, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81. https://doi.org/10.1111/j.1469-0691.2011.03570.x.
Centers for Disease Control and Prevention. National Healthcare Safety Network surveillance definitions for specific types of infections [Internet]. 2016 [cited 2017 23]. Available at: http://www.cdc.gov/nhsn/PDFs/pscManual/17pscNosInfDef_current.pdf.
Marshall JC, Maier RV, Jimenez M, Dellinger EP. Source control in the management of severe sepsis and septic shock: an evidence-based review. Crit Care Med. 2004;32:S513–26.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing: Twenty-Fifth Informational Supplement MS100-S25. CLSI, Wayne, PA, USA, 2015. [Internet]. [cited 2017 29] http://shop.clsi.org/site/Sample_pdf/M100S25_sample.pdf.
National Committee for Clinical Laboratory Standards. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard M07-A10–Tenth Edition. NCCLS, Wayne, PA, USA, 2015. [Internet] [cited 2017 29] http://shop.clsi.org/site/Sample_pdf/M07A10_sample.pdf.
EUCAST: Clinical breakpoints [Internet] [cited 2017 29] http://www.eucast.org/clinical_breakpoints//.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic Dis. 1987;40:373–83.
Linden PK, Kusne S, Coley K, Fontes P, Kramer DJ, Paterson D. Use of parenteral colistin for the treatment of serious infection due to antimicrobial-resistant Pseudomonas aeruginosa. Clin Infect Dis. 2003;1:e154–60. https://doi.org/10.1086/37961.
Dalfino L, Puntillo F, Ondok MJM, Mosca A, Monno R, Coppolecchia S, et al. Colistin-associated acute kidney injury in severely ill patients: a step toward a better renal care? A prospective cohort study. Clin Infect Dis. 2015;15:1771–7. https://doi.org/10.1093/cid/civ717.
Nation RL, Garonzik SM, Li J, Thamlikitkul V, Giamarellos-Bourboulis EJ, Paterson DL, et al. Updated US and European dose recommendations for intravenous colistin: how do they perform? Clin Infect. Dis. 2016;62:552–8. https://doi.org/10.1093/cid/civ964.
US National Institutes of Health. ClinicalTrials.gov. Safety and efficacy study of ceftolozane/tazobactam to treat ventilated nosocomial pneumonia (MK-7625A-008)(ASPECT-NP). [Internet]. https://www.clinicaltrials.gov/ct2/show/ NCT02070757?term“ceftolozane?tazobactam&rank”3.
Martínez ML, Ferrer R, Torrents E, Guillamat-Prats R, Gomà G, Suárez D, et al. Impact of source control in patients with severe sepsis and septic shock. Crit Care Med. 2017;45:11–9. https://doi.org/10.1097/CCM.0000000000002011.
Fraile-Ribot PA, Cabot G, Mulet X, Periañez L, Martín-Pena ML, Juan C, et al. Mechanisms leading to in vivo ceftolozane/tazobactam resistance development during the treatment of infections caused by MDR Pseudomonas aeruginosa. J Antimicrob Chemother. 2017. https://doi.org/10.1093/jac/dkx424/4629302.
Berrazeg M, Jeannot K, Ntsogo Enguéné VY, Broutin I, Loeffert S, Fournier D, et al. Mutations in β-lactamase AmpC increase resistance of Pseudomonas aeruginosa isolates to antipseudomonal cephalosporins. Antimicrob Agents Chemother. 2015;59:6248–55. https://doi.org/10.1128/AAC.00825-15.
Cabot G, Bruchmann S, Mulet X, Zamorano L, Moya B, Juan C, et al. Pseudomonas aeruginosa ceftolozane–tazobactam resistance development requires multiple mutations leading to overexpression and structural modification of AmpC. Antimicrob Agents Chemother. 2014;1:3091–9. https://doi.org/10.1128/AAC.02462-13.
Acknowledgements
We thank Celine Cavallo for English language support.
Funding
Supported by Plan Nacional de I + D+I 2013-2016 and Instituto de Salud Carlos III, Subdirección General de Redes y Centros de Investigación Cooperativa, Ministerio de Economía, Industria y Competitividad, Spanish Network for Research in Infectious Diseases (REIPI RD16/0016/0003)—co-financed by European Development Regional Fund “A way to achieve Europe”, Operative program Intelligent Growth 2014-2020. MSD provided medical writing support but was not involved in the content of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
CP. has received honoraria for talks on behalf of Angelini, MSD, Novartis, Pfizer, Salvat, and Zambon. O.L. has received honoraria for talks on behalf of Astellas, MSD and Pfizer. R.F. has received honoraria for talks on behalf of MSD, Pfizer, Estor and Orion. B.A. has received grant support from Gilead Sciences, Pfizer, and the Instituto de Salud Carlos III. He has received honoraria for talks on behalf of Gilead Sciences, Merck Sharp & Dohme, Pfizer, Astellas Pharma, Novartis, and Angelini. The other authors have no declarations.
Rights and permissions
About this article
Cite this article
Escolà-Vergé, L., Pigrau, C., Los-Arcos, I. et al. Ceftolozane/tazobactam for the treatment of XDR Pseudomonas aeruginosa infections. Infection 46, 461–468 (2018). https://doi.org/10.1007/s15010-018-1133-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-018-1133-5