Abstract
Introduction
Telemedicine during this pandemic acts as a lifeline for many non-COVID patients especially with chronic neurological diseases. The aim of present study was to evaluate cost effectiveness and level of satisfaction amongst patients from teleneurology outpatient department (OPD).
Methods
An online cross-sectional survey, having questions both in Hindi and English was conducted via telemedicine facility at Institute of Medical Sciences, Banaras Hindu University, Varanasi, India. Demographic variables, illness details, travel distance and time taken, travel expenditure, level of satisfaction and preferred choice among tele OPD versus in-person OPD once pandemic ends were recorded.
Results
Total 1388 patients filled the online COVID-19 teleneurology survey google form. Mean age was 39.21 ± 16.72 years. Majority (N = 824, 59%) were males. Six hundred (43%) patients’ educational qualification were ≤ 10th standard. Majority of patients (N = 840, 60.5%) belonged to the rural background. Headache (N = 424, 30.5%) followed by backache (N = 220, 16%), stroke (N = 176, 13%) and seizure (N = 148, 11%) were the common illnesses. Travel time of > 5 hours was saved in 496 (36%) patients and travel expenditure of > Rs100 in 796 (57%) patients. About 96% (N = 1332) felt satisfied with the treatment advice via teleconsultation.
Discussion
Teleneurology facility is not only feasible but also affordable and acceptable in various neurological conditions. The chief reasons being no waiting time, saving of travelling time and travel expenditure with good satisfaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Telemedicine is a mean of health care delivery by the utilisation of telecommunication technologies. Earliest available record of telemedicine was from 1950s to 1960 when they transmitted ECG over telephone lines [1]. During COVID-19 pandemic and National Lockdown, closure of outpatient services, cancellation and postponement of various planned procedures, unavailability of health care providers due to fear of risk of viral transmission as well as diversion towards COVID-19 management led to disruption of health services in both developed and developing countries [2, 3].
Though during this crisis period getting consultation was impossible for chronic neurological patients, teleconsultation proved a boon for them. Both new and old patients from faraway areas got the consultation by contacting on the advertised contact number for different specialties at various health care facilities of the country. The benefits of telemedicine services are not restricted to any particular race, age, and geographical location. However, factors such as lack of internet access, digital illiteracy, technological distrust, and reimbursement issues may lead to underutilisation of this service [4]. During present COVID-19 pandemic, the Teleconsultation, an underutilized method of health care delivery, proved indispensable and patients understood its invaluable role in patient–doctor interaction [5, 6]. The present study, a questionnaire-based survey, was conducted to evaluate the cost effectiveness and level of satisfaction amongst neurological patients from teleneurology outpatient department (OPD).
Materials and methods
Study design, settings and participants
An online cross-sectional survey was conducted via tele-medicine facility at Institute of Medical Sciences (I.M.S.), Banaras Hindu University (B.H.U.), Varanasi, India from June 2020 to October 2020. All patients from neighboring districts and states suffering from neurological diseases were included in the study. Ethical clearance was obtained from the Institute Ethical Committee (2020/EC/1996). No prior sample size calculation was done for the study.
Study procedure
The telemedicine services were started in the Department of Neurology, I.M.S., B.H.U., Varanasi, Uttar Pradesh, India. The telemedicine guidelines by the Ministry of Health and Family Welfare were the reference document for the conduct of the teleconsultation services [7]. Dedicated smartphones with high-speed internet facility were provided by the Institute authorities for conducting the teleconsultation. Demographic parameters, diagnosis, treatment details, investigations, any new or aggravation of the previous symptoms were enquired telephonically from the patient/family members and noted in a prespecified format. The details of the teleneurology consultation methodology is summarised in the authors’ previous published paper [8]. The patients/family members were offered a questionnaire on their phone (by WhatsApp or email) which they had to fill post teleconsultation. This was an electronic survey and was conducted after taking informed consent. Participants had to answer a yes–no question to confirm their willingness to participate. After their assents, the participants were directed to complete the self-report questionnaire. Confidentiality of the records were maintained.
Questionnaire
The cover page of the questionnaire includes a consent form, a declaration of confidentiality, and anonymity. The questionnaire consists of two parts: demographic details and study survey. Demographic variables include age, sex, education level, occupation, native state and contact number. The survey section consisted of questions both in Hindi and English regarding diagnosis, source of information of initiation of telemedicine services, saving of travel time, distance covered and travel expenses, level of satisfaction, any suggestions for improvement, preferred options, reason for preferring Telemedicine and preference between tele OPD and in person OPD post pandemic (Table 1). The questionnaire provided in google form for online survey was based on difficulties faced by neurological patients during COVID-19 pandemic and included the "keywords". However, it was not validated or tested in a pilot study. Translation of questionnaire was forward and it was checked again with backward translation.
Inclusion criteria
Patients with age more than 18 years who can understand the content of the survey and willing to participate were included. For patients below 18 years, consent of parents was essential. Only patients with a previous in-person follow-up visit were included to assess their tele-consult experience in the context of their usual in-person visit.
Exclusion criteria
Those who declined the consent for the participation or new patients were excluded from the study.
Statistical analysis
Statistical analysis was performed with SPSS software version 25.0 and Excel (office 365) were primarily used for analysis of data. Quantitative variables were described as mean and standard deviation (SD), whereas categorical data were presented as numbers (percentage). Chi Square test was performed between satisfaction status and gender, occupation as well as background. Variables with a P value < 0.05 were considered significant.
Results
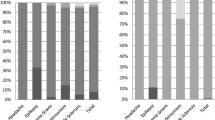
The data of initial 150 days of the survey were taken. Total 1396 patients attempted the online teleneurology survey google form. However, eight refused to give the consent. Hence, 1388 patients were included in the study (Fig. 1). Mean age of the patients was 39.21 ± 16.72 years. Majority of patients (N = 824, 59%) were males. Friends (N = 432, 31%), newspaper (N = 392, 28%), other health care professional (N = 208, 15%) were the chief sources of information regarding teleservices. Six hundred (43%) patients’ educational qualification were ≤ 10th standard. Majority of patients (N = 840, 60.5%) belonged to the rural background. Most of the patients (N = 1168, 84%) were residents of the native state (Table 2). Headache (N = 424, 30.5%) followed by backache (N = 220, 16%), stroke (N = 176, 13%) and seizure (N = 148, 11%) were the common illnesses, for which opinions were taken. Regarding suggestion for the ongoing Telemedicine consultation facility, 1024 (74%) patients did not suggest any modification. Of remaining 26%, 172 (12%) recommended video call facility, 32 (2%) proper telemedicine infrastructure and 160 (12%) an emergency contact number for communication in relation to critical patients (Table 2). Nearly half of the patients had to travel > 50 km to attend neurology OPD services (Fig. 2). The time efficacy and cost effectiveness of the telemedicine services was also revealed by the significant saving of travel time and expenditure (Figs. 3, 4).
Most of the patients (N = 1332, 96%) felt satisfied with the treatment advice via teleconsultation (Fig. 5). Nealy half of the patients opted for telemedicine services even after the end of pandemic. Major reasons were equal efficacy (N = 272, 20%) and less waiting time (N = 264, 19%) (Table 2).
There was no significant difference between satisfaction status and gender (P = 0.163), occupation (P = 0.171) and background status (P = 0.218).
Discussion
The present study evaluated the cost effectiveness and satisfaction level amongst neurological patients, who received consultation from teleneurology OPD. Contrary to the belief that low literacy rate and rural background were limitation for utilization of telemedicine services [9], we have most of our patients from rural background having formal education ≤ 10th standard in 43% patients. Teleneurology consultation service was the preferred choice for consultation in 48% patients, once the pandemic ends. The observed data point towards the teleconsultation as an invaluable tool to provide the health services with comparable satisfaction in a cost-effective manner.
Despite of the presence of a well-equipped infrastructure for telecommunication, teleconsultation was given to the patients via the use of a smartphone. Text message, WhatsApp chats and videos were used considering the mismatch between availability of infrastructure at the level of health care providers and patients. Different telecommunication tools, such as email, videoconferencing, text messages and WhatsApp messenger has been used in teleconsultation regarding different health problems, risk factor assessment and medication adherence[10]. We also observed teleneurology consultation as effective as in-person OPD in the management of neurological disorders in a Virtual Telephone and WhatsApp Video-Enabled neurology clinic during COVID-19 Lockdown. The satisfaction rate among patients using teleservices was 90% [8].
In present study, 340 (24%) patients were > 50 years. Owing to higher risk of severe disease and mortality in older age group, elderly patients preferred to use it to avoid the risk of exposure to SARS-COV-2.
Around 16% patients were from outside native state. This signifies the importance of telemedicine in managing neurological patients from remote areas and its benefit in terms of cost and time in this pandemic as in other diseases [11, 12].
In our study, telemedicine users were mainly from rural areas (60.5%). This finding is higher in contrast to a study by Jaffe et al. [13] Compulsion due to poor accessibility of health services, fear of COVID exposure and impaired transport facilities in Lockdown period might be the reason for larger percentage of rural areas residents.
Headache (30.5%) followed by backache, stroke, and seizure were the most common ailments for which the consultation was sought telephonically. The role of teleconsultation in the management across the different spectrum of neurological disorders is well established ranging from acute illness, such as stroke, head injury to chronic disorders, such as amyotrophic lateral sclerosis and movement disorders [14,15,16,17,18,19,20].
In our study, saving of travel time, travel expenditure, official leave and equal efficacy were the suggested reason for preference of teleneurology services once the pandemic ends. In a study by Vosburg et al., saving of travel time > 30 min, easy visit connection, use of video platform over telephone platform and identification as female were significantly associated with higher level of satisfaction [21]. However, Telemedicine health care providers also felt that in person visit is needed for extensive clinical evaluation in specific cases.
Use of smartphones has been increased in recent years and people from remote places are more or less well acquainted with the various software applications, such as WhatsApp, mails etc. The higher percentage of patients from rural background who consulted us showed that these technological advancements are not new to them.
A study from Jordan reported that patients with chronic neurological diseases communicated with their consultants via telephone. Text messages and WhatsApp was used as means of communication similar to the present study [22].
Similar to our study, Raheja et al. also found that majority (97%) of neurosurgical patients felt that teleconsultation was beneficial in lockdown period by reducing exposure to COVID-19. 60% patients were willing for continuation of teleconsultation. Challenges felt by them in teleconsultations were poor network (7%), suboptimal communication/discussion (5.6%), lack of physical examination (6%), and misinterpretation of prescription by pharmacists/patients (6%) [23]. The ICU consultants of smaller hospitals at remote places were also benefitted by teleconsultation. In a study, 61 neuro-consultations were provided for 56 patients admitted in remote ICU during COVID-19 pandemic, hence emphasizing the need for eNeuroIntensive care [24].
The recommendation by government of India during COVID-19 pandemic to maintain social distancing with closure of routine OPD services led to enormous challenges for clinician and their patients. People had sense of unfamiliarity to the telecommunication along with economic and health crisis due to National Lockdown in COVID-19 pandemic. On the other hand, clinician needed to manage both critical and non-critical patients with limited beds, closed OPDs and overburdened emergency services. In such scenario, Teleconsultation services proved a boon for both out and inpatient services.
However, the utility of this tool needs to be extended beyond this pandemic period in a developing country like ours. After this pandemic period, restoration of OPD and emergency services, similar to pre-COVID era, needs to be complemented by telemedicine for getting appointments, reviewing the investigations and follow-up course and lifesaving advice to critically ill patients from faraway places. Apart from these, it has immense potential to be used as surveillance and infection control tool as well.
Limitations
Data collection from a single tertiary care center limits its generalizability to other geographical area. Limited socioeconomic details were also one of the limitations. The general terminologies were used for common neurological disorders such as “headache” and “backache” rather than their subclassification as the questionnaire was filled by patients/their relatives. Results of this study cannot be generalised to other population of interest because of being a single center study involving a particular geographical region. Analytical approaches were not utilized and multivariate analysis was not conducted as there might be multiple confounders that might affect the cost benefit observation.
Conclusions
Teleneurology facility was not only feasible, but also affordable and acceptable in various neurological conditions. Literacy and socioeconomic background were not barriers for the teleconsultation and it was the preferred choice for nearly half of patients even after pandemic. It can be used as a very effective tool for providing health services in pandemic situations, such as COVID-19. In addition, it can also be used as a parallel means of health care delivery in addition to standard in person consultation. However, there is a requirement of further studies for the confirmation of the points made in this study.
References
History of Telemedicine—md Portal n.d. http://mdportal.com/education/history-of-telemedicine/. Accessed 12 June 2020
Shivendra Srivastava. OPD services halted in 7 UP districts amid Covid spike, elective surgeries postponed. https://www.indiatoday.in/cities/lucknow/story/uttar-pradesh-opd-services-halted-coronavirus-1790798-2021-04-14
World Health Organization. COVID-19 significantly impacts health services for noncommunicable diseases. https://www.who.int/news/item/01-06-2020-covid-19-significantly-impacts-health-services-for noncommunicable-Diseases
Ramsetty A, Adams C (2020) Impact of the digital divide in the age of COVID-19. J Am Med Inform Assoc 27:1147–1148
Moazzami B, Razavi-Khorasani N, Dooghaie Moghadam A, Farokhi E, Rezaei N (2020) COVID-19 and telemedicine: immediate action required for maintaining healthcare providers well-being. J Clin Virol 126:104345
Ohannessian R, Duong TA, Odone A (2020) Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill 6:e18810
Telemedicine Practice Guidelines. The Ministry of Health and Family Welfare, Govt of India. https://www.mohfw.gov.in/pdf/Telemedicine.pdf
Mishra VN, Pathak A, Chaurasia RN, Kumar A, Joshi D, Singh VK (2021) Observations in a virtual telephone and Whatsapp video-enabled neurology clinic during lockdown in Varanasi, India—a preliminary report. Neurol India 69:1234–1240
Dasgupta A, Deb S (2008) Telemedicine: a new horizon in public health in India. Indian J Community Med 33(1):3–8. https://doi.org/10.4103/0970-0218.39234
Ganapathy S, de Korne DF, Chong NK, Car J (2020) The role of text messaging and telehealth messaging apps. Pediatr Clin N Am 67(4):613–621
Buvik A, Bergmo TS, Bugge E, Smaabrekke A, Wilsgaard T, Olsen JA (2019) Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res 21(2):e11330
Lee JY, Lee SWH (2018) Telemedicine cost-effectiveness for diabetes management: a systematic review. Diabetes Technol Ther 20:492–500
Jaffe DH, Lee L, Huynh S, Haskell TP (2020) Health inequalities in the use of telehealth in the United States in the lens of COVID-19. Popul Health Manag 23:368–377
Hubert GJ, Santo G, Vanhooren G, Zvan B, Tur Campos S, Alasheev A et al (2019) Recommendations on telestroke in Europe. Eur Stroke J 4:101–109
Gabriel KMA, Jírů-Hillmann S, Kraft P, Selig U, Rücker V, Mühler J et al (2020) Two years’ experience of implementing a comprehensive telemedical stroke network comprising in mainly rural region: the Trans regional Network for Stroke Intervention with Telemedicine (TRANSIT-Stroke). BMC Neurol 20:104
Paganoni S, Simmons Z (2018) Telemedicine to innovate amyotrophic lateral sclerosis multidisciplinary care: the time has come. Muscle Nerve 59:3–5
Srinivasan R, Ben-Pazi H, Dekker M, Cubo E, Bloem B, Moukheiber E, Gonzalez-Santos J, Guttman M (2020) Telemedicine for hyperkinetic movement disorders. Tremor Other Hyperkinet Mov (N Y). https://doi.org/10.7916/tohm.v0.698
Wilson AM, Jamal NI, Cheng EM, Inkelas M, Saliba D, Hanssen A et al (2020) Teleneurology clinics for polyneuropathy: a pilot study. J Neurol 267:479–490
Torrisi M, Maresca G, De Cola MC, Cannavò A, Sciarrone F, Silvestri G et al (2019) Using telerehabilitation to improve cognitive function in post-stroke survivors: is this the time for the continuity of care? Int J Rehabil Res 42:344–351
Sidek MSM, Siregar JA, Ghani ARI, Idris Z (2018) Teleneurosurgery: outcome of mild head injury patients managed in non-neurosurgical centre in the state of Johor. Malays J Med Sci 25:95–104
Vosburg RW, Robinson KA (2022) Telemedicine in primary care during the COVID-19 pandemic: provider and patient satisfaction examined. Telemed J E Health 28(2):167–175
Yassin A. Invited commentary: Neurology service during COVID‑19 lockdown in Jordan: Challenges and solutions. Neurology Blogs. https://blogs.neurology.org/global/invitedcommentaryneurology‑service‑during‑covid‑19‑lock‑down-in‑jordan‑challenges‑and‑solutions/
Raheja A, Manjunath N, Garg K, Tandon V, Gupta V, Mishra S et al (2021) Turning a new chapter in neurosurgery outpatient services: telemedicine A “savior” in this pandemic. Neurol India 69(2):344–351
Haranath SP, Ganapathy K, Kesavarapu SR, Kuragayala SD (2021) eNeuroIntensive care in India: the need of the hour. Neurol India 69(2):245–251
Acknowledgements
We acknowledge all our patients for giving their consent and participating in the study.
Funding
None.
Author information
Authors and Affiliations
Contributions
AK concept and design of study, Writing the manuscript. NL writing and editing the manuscript. AP analyzing data and reviewing the manuscript, editing the manuscript. DJ data collection and reviewing the manuscript. VNM data collection and reviewing the manuscript. RNC data collection and reviewing the manuscript. VKS analyzing data, writing, editing and reviewing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Both Dr. Anand Kumar and Neha Lall will have the first authorship. Rest there is no conflicts of interest between the authors to declare.
Ethical statement
The study was approved by institute ethical committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kumar, A., Lall, N., Pathak, A. et al. A questionnaire-based survey of acceptability and satisfaction of virtual neurology clinic during COVID-19 lockdown: a preliminary study. Acta Neurol Belg 122, 1297–1304 (2022). https://doi.org/10.1007/s13760-022-02004-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-022-02004-0