Abstract
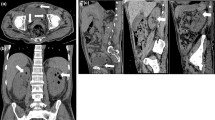
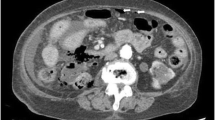
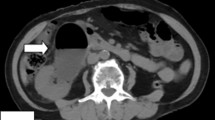
Emphysematous pyelonephritis (EPN) is a necrotizing bacterial infection characterized by gas retention and a poor prognosis. We present the case of a 75-year-old man who was diagnosed early with EPN and received multidisciplinary treatment. He had poorly controlled type 2 diabetes mellitus (DM) and chronic kidney disease (CKD), and was treated with oral hypoglycemic drugs, including a sodium–glucose co-transporter-2 inhibitor. He experienced the onset of back pain in the midsection of his back, tenderness in the costovertebral angle, and a high fever (> 39 °C), accompanied by tachycardia, hypotension, and tachypnea. The patient was diagnosed with pyelonephritis and septic shock. Immediate measures encompassing empirical antibiotic therapy, administration of noradrenaline, blood glucose regulation, and urethral catheterization were implemented. However, due to the persistent fever (> 38 °C) and lack of improvement in his condition, abdominal computed tomography (CT) was repeated on the fourth day. This revealed the presence of gas around the right kidney parenchyma, leading to a diagnosis of EPN that had evolved from acute pyelonephritis. Subsequently, percutaneous drainage of the right kidney parenchyma was performed. Subsequently, multidisciplinary treatment was continued, and his condition gradually improved. Clinicians should evaluate abdominal CT when acute pyelonephritis does not improve within a few days of antibiotic therapy. Disease progression from acute pyelonephritis to EPN should be considered in patients with DM and CKD.



Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Schainuck LI, Fouty R, Cutler RE. Emphysematous pyelonephritis. A new case and review of previous observations. Am J Med. 1968;44:134–9.
Olvera-Posada D, Armengod-Fischer G, Vázquez-Lavista LG, Maldonado-Ávila M, Rosas-Nava E, Manzanilla-García H, et al. Emphysematous pyelonephritis: multicenter clinical and therapeutic experience in Mexico. Urology. 2014;83:1280–4.
Rahoui M, Ouanes Y, Chaker K, Bibi M, Dali KM, Sellami A, et al. Predictive factors for failure of conservative management in patients with emphysematous pyelonephritis. Ann Med Surg (Lond). 2022;78: 103930.
Japanese Association for Infectious Disease/Japanese Society of Chemotherapy; JAID/JSC Guide/Guidelines to Clinical Management of Infectious Disease Preparing Committee; Urinary tract infection/male genital infection working group, Shingo Y, Kiyohito I, Hiroshi H, Tadahiro N, Isao M, Tadashi H, et al. JAID/JSC Guidelines for clinical management of infectious disease 2015 - urinary tract infection/male genital infection. J Infect Chemother. 2017;23(11):733–51.
Huang JJ, Tseng CC. Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med. 2000;160:797–805.
Ahlering TE, Boyd SD, Hamilton CL, Bragin SD, Chandrasoma PT, Lieskovsky G, et al. Emphysematous pyelonephritis: a 5-year experience with 13 patients. J Urol. 1985;134:1086–8.
Wan YL, Lee TY, Bullard MJ, Tsai CC. Acute gas-producing bacterial renal infection: correlation between imaging findings and clinical outcome. Radiology. 1996;198:433–8.
Soulen MC, Fishman EK, Goldman SM, Gatewood OM. Bacterial renal infection: role of CT. Radiology. 1989;171:703–7.
Expert Panel on Urologic Imaging, Nikolaidis P, Dogra VS, Goldfarb S, Gore JL, Harvin HJ, Heilbrun ME, et al. ACR appropriateness Criteria® acute pyelonephritis. J Am Coll Radiol. 2018;15:S232–9.
Bonkat G, Bartoletti R, Bruyère F, Cai T, Geerlings SE, Köves B, et al. European Association of Urology 2022 guidelines on urological infections. https://uroweb.org/guidelines/urological-infections/summary-of-changes/2022. Accessed 5 Mar 2023.
Owa S, Sasaki K, Yonemura S, Sakurai M. A case of emphysematous pyelonephritis after starting treatment for acute pyelonephritis. Hinyokika Kiyo. 2021;67:373–9.
Takei T, Hama Y, Ito T, Takemoto M. Emphysematous pyelonephritis detected incidentally by a second CT examination after the improvement of septic shock. Nihon Shuchu Chiryo Igakukai Zasshi. 2009;16:487–91.
Somani BK, Nabi G, Thorpe P, Hussey J, Cook J, N’Dow J. Is percutaneous drainage the new gold standard in the management of emphysematous pyelonephritis? Evidence from a systematic review. J Urol. 2008;179:1844–9.
Aboumarzouk OM, Hughes O, Narahari K, Coulthard R, Kynaston H, Chlosta P, et al. Emphysematous pyelonephritis: time for a management plan with an evidence-based approach. Arab J Urol. 2014;12:106–15.
Adapala RR, Shetty R, Venugopal P, Prabhu GGL, Yalla D, Unnikrishnan B. Renal salvage, an achievable goal in patients with emphysematous pyelonephritis: outcomes of an algorithmic renal preserving strategy. Urol Ann. 2020;12:156–62.
US Food and Drug Administration. FDA drug safety communication: FDA revises labels of SGLT2 inhibitors for diabetes to include warnings about too much acid in the blood and serious urinary tract infections; updated 2018. https://www.fda.gov/drugs/drug-safety-and-availability/fda-revises-labels-sglt2-inhibitors-diabetes-include-warnings-about-too-much-acid-blood-and-serious. Accessed 21 Oct 2022.
Fisher A, Fralick M, Filion KB, Dell’Aniello S, Douros A, Tremblay E, et al. Sodium-glucose co-transporter-2 inhibitors and the risk of urosepsis: a multi-site, prevalent new-user cohort study. Diabetes Obes Metab. 2020;22:1648–58.
Tanvi P, Morgan C, Jesse H, Alamdeep K, Aliza L. Evaluating the safety of sodium-glucose cotransporter-2 inhibitors in a nationwide veterans health administration observational cohort study. Am J Cardiol. 2023;201:281–3.
Dave CV, Schneeweiss S, Kim D, Fralick M, Tong A, Patorno E. Sodium-glucose cotransporter-2 inhibitors and the risk for severe urinary tract infections: a population-based cohort study. Ann Intern Med. 2019;171:248–56.
Mauro R, Gian PF, Angelo A. Safety of sodium-glucose cotransporter 2 inhibitors in elderly patients with type 2 diabetes: a meta-analysis of randomized controlled trials. Diabetes Obes Metab. 2023. https://doi.org/10.1111/dom.15193.Accessed26Jul.
Sarah E, Christine L, Lindsay T. Evaluation of the safety and tolerability of sodium-glucose co-transporter 2 inhibitors in the older population: a systematic review. Sr Care Pharm. 2023;38:276–87.
Kufel WD, Scrimenti A, Steele JM. A case of septic shock due to Serratia marcescens pyelonephritis and bacteremia in a patient receiving empagliflozin. J Pharm Pract. 2017;30:672–5.
Woloshuk A, Lee M, Assmus M, Agarwal D, Krambeck A, Large T. A case of ureteral fungal mass removal in a patient taking empagliflozin. CEN Case Rep. 2021;10:603–7.
Vinik AI, Maser RE, Mitchell BD, Freeman R. Diabetic autonomic neuropathy. Diabetes Care. 2003;26:1553–79.
Funding
None.
Author information
Authors and Affiliations
Contributions
All the authors met the ICMJE authorship criteria. All the authors contributed significantly to this work. MN, DY, and TK were treating physicians in the current case and prepared the images and data tables for the manuscript. MN, MH, and DY drafted the manuscript. TK, KH, and YK revised and supervised the manuscript. All authors approved the submission of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Declaration of Helsinki 1964 and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Nishikawara, M., Harada, M., Yamazaki, D. et al. A case of emphysematous pyelonephritis in an older man with poorly controlled type 2 diabetes mellitus. CEN Case Rep 13, 161–167 (2024). https://doi.org/10.1007/s13730-023-00821-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13730-023-00821-7
Keywords
Profiles
- Makoto Harada View author profile