Abstract
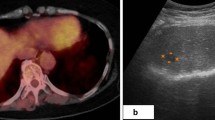
Reactive lymphoid hyperplasia (RLH) of the liver is extremely rare. Despite advancements in diagnostic imaging technology, it is still difficult to distinguish from hepatocellular carcinoma (HCC). Herein, we present a case of hepatic RLH mimicking HCC that was postoperatively diagnosed using several imaging modalities. A 78-year-old female was referred to our hospital with a positive hepatitis C virus antibody (HCV Ab) test. Ultrasonography revealed a 13 mm isoechoic lesion in segment 8 of the liver. Contrast-enhanced computed tomography (CE-CT) demonstrated arterial hyperintensity and washout during the later phase. On ethoxybenzyl magnetic resonance imaging (EOB-MRI), the lesion was hyperenhanced in the arterial phase and of low intensity in the hepatocyte phase. Although the tumor markers were all within normal limits, the pattern of contrast enhancement of the tumor on CT and MRI was consistent with that of HCC. We performed S8 segmentectomy of the liver. Histological examination of the resected specimen revealed dense lymphoid tissue of variable sizes and shapes with expanded germinal centers. Immunohistochemical examination was positive for CD3, CD10 (germinal center), and CD20, and negative for B-cell lymphoma 2 (bcl-2) (germinal center) and Epstein–Barr virus (EBV). A polymerase chain reaction (PCR) analysis of IgH-gene rearrangements revealed polyclonality. Based on these findings, hepatic RLH was diagnosed. The postoperative course was uneventful, and the patient was discharged on the 10th postoperative day. She had a good quality of life after surgery and no liver nodule recurrence was detected at the 4-month medical follow-up. Hepatic RLH is an extremely rare disease and preoperative diagnosis is difficult. This should be considered in the differential diagnosis of single small hepatic tumors. An echo-guided biopsy and careful observation of imaging may help diagnose hepatic RLH, and a PCR analysis of IgH-gene rearrangements would be necessary for the definitive diagnosis of hepatic RLH.






Similar content being viewed by others
Availability of data and materials
The authors declare that all the data in this article are available within the article.
Abbreviations
- RLH:
-
Reactive lymphoid hyperplasia
- HCC:
-
Hepatocellular carcinoma
- CE-CT:
-
Contrast-enhanced computed tomography
- EOB-MRI:
-
Ethoxybenzyl magnetic resonance imaging
- Bcl-2:
-
B-cell lymphoma 2
- EBV:
-
Epstein–Barr virus
- PCR:
-
Polymerase chain reaction
- DWI:
-
Diffusion-weighted imaging
- ICG-R15:
-
Indocyanine green retention rate at 15 min
- CEA:
-
Carcinoembryonic antigen
- CA19-9:
-
Carbohydrate antigen 19–9
- AFP:
-
Alpha-fetoprotein
- PIVKA-II:
-
Protein induced by vitamin K absence-II
- US:
-
Ultrasonography
- IgH:
-
Immunoglobulin heavy chain
- PNE:
-
Perinodular enhancement
- PET-CT:
-
Positron emission tomography–Computed tomography
- SUVmax:
-
Standardized uptake value max
References
Kobayashi A et al (2011) MR imaging of reactive lymphoid hyperplasia of the liver. J Gastrointest Surg 15(7):1282–1285
Zen Y, Fujii T, Nakanuma Y (2010) Hepatic pseudolymphoma: a clinicopathological study of five cases and review of the literature. Mod Pathol 23(2):244–250
Okada T et al (2009) Pseudolymphoma of the liver associated with primary biliary cirrhosis: a case report and review of literature. World J Gastroenterol 15(36):4587–4592
Ishida M et al (2010) Hepatic reactive lymphoid hyperplasia in a patient with primary biliary cirrhosis. World J Hepatol 2(10):387–391
Takahashi H et al (2006) Reactive lymphoid hyperplasia of the liver in a patient with colon cancer: report of two cases. BMC Gastroenterol 6:25
Ohtsu T et al (1994) Development of pseudolymphoma of liver following interferon-alpha therapy for chronic hepatitis B. Intern Med 33(1):18–22
Talamo TS et al (1980) Primary hepatic malignant lymphoma: its occurrence in a patient with chronic active hepatitis, cirrhosis, and hepatocellular carcinoma associated with hepatitis B viral infection. Cancer 46(2):336–339
Kim SR et al (1997) A case of pseudolymphoma of the liver with chronic hepatitis C. J Hepatol 26(1):209–214
Zampino R et al (2015) Hepatocellular carcinoma in chronic HBV-HCV co-infection is correlated to fibrosis and disease duration. Ann Hepatol 14(1):75–82
Zhang W, Zheng S (2019) Reactive lymphoid hyperplasia of the liver: A case report. Medicine (Baltimore) 98(30):e16491
Kanno H et al (2020) A case of reactive lymphoid hyperplasia of the liver in a patient with autoimmune hepatitis. Surg Case Rep 6(1):90
Dong CH et al (2019) Contrast-enhanced ultrasound features of hepatic reactive lymphoid hyperplasia: correlation with histopathologic findings. J Ultrasound Med 38(9):2379–2388
Bao C et al (2018) Prognostic value of fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography in primary hepatic mucosa-associated lymphoid tissue lymphoma: a case report and review of the literature. Medicine (Baltimore) 97(10):e9877
Lu RC et al (2019) Positron-emission tomography for hepatocellular carcinoma: Current status and future prospects. World J Gastroenterol 25(32):4682–4695
Machida T et al (2007) Reactive lymphoid hyperplasia of the liver: a case report and review of literature. World J Gastroenterol 13(40):5403–5407
Yoshida K et al (2013) Hepatic pseudolymphoma: imaging-pathologic correlation with special reference to hemodynamic analysis. Abdom Imaging 38(6):1277–1285
Zhou Y et al (2018) Hepatic pseudolymphoma: imaging features on dynamic contrast-enhanced MRI and diffusion-weighted imaging. Abdom Radiol (NY) 43(9):2288–2294
Lv A et al (2015) Reactive lymphoid hyperplasia of the liver mimicking hepatocellular carcinoma: incidental finding of two cases. Int J Clin Exp Pathol 8(5):5863–5869
Miyazaki Y et al (2018) Indocyanine green fluorescence-navigated laparoscopic metastasectomy for peritoneal metastasis of hepatocellular carcinoma: a case report. Surg Case Rep 4(1):130
Yoshikawa K et al (2011) Reactive lymphoid hyperplasia of the liver: literature review and 3 case reports. Hepatogastroenterology 58(109):1349–1353
Amer A et al (2012) Reactive lymphoid hyperplasia of the liver and pancreas. a report of two cases and a comprehensive review of the literature. Clin Res Hepatol Gastroenterol 36(4):e71-80
Bagg A et al (2002) Immunoglobulin heavy chain gene analysis in lymphomas: a multi-center study demonstrating the heterogeneity of performance of polymerase chain reaction assays. J Mol Diagn 4(2):81–89
Lu C et al (2017) The value of detecting immunoglobulin gene rearrangements in the diagnosis of B-cell lymphoma. Oncotarget 8(44):77009–77019
Ota H et al (2006) A case of hepatic pseudolymphoma observed without surgical intervention. Hepatol Res 35(4):296–301
Sousa PM, Afonso Goncalves GG, Ana C (2021) Ferreira, reactive Lymphoid Hyperplasia, a Mimicker of Hepatocelular Carcinoma. Acta Radiol Port. 33:39–41
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
All authors have no funding regarding this paper.
Author information
Authors and Affiliations
Contributions
JM reported the case and wrote the manuscript. KY, TM, ST were engaged in the patient’s care including the surgery. ET helped in drafting the manuscript. TM participated in revising the manuscript critically. All authors have read and approved the final manuscript for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Mita, J., Maeda, T., Tsujita, E. et al. A case of difficult-to-diagnose hepatic reactive lymphoid hyperplasia finally diagnosed by using PCR analysis of IgH-gene rearrangements: a case report. Int Canc Conf J 13, 33–39 (2024). https://doi.org/10.1007/s13691-023-00632-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13691-023-00632-8