Abstract
Purpose of Review
This review was conducted to gain insight into the history, present and future of bariatric and/or metabolic surgery and endoscopic treatments of obesity. The challenges that have been overcome, the challenges we still face and our recommendations for the future are discussed.
Recent Findings
Over the last few decades, a number of treatment strategies have emerged for the treatment of obesity. Both endoscopic and surgical options are available and they lead to significant weight loss and comorbidity reduction. However, to remain a credible treatment alternative to the obesity pandemic, we need to perform these procedures in much larger numbers than we currently do. Even though significant gains have been made in reducing the morbidity and mortality of surgical interventions, there is further room for improvement, especially when it comes to long-term issues. Due to its impact on almost every single organ system in the human body, bariatric surgery has attracted the attention of academics from a variety of medical disciplines. This has led to a rapidly enlarging body of high-quality scientific literature, supporting its wider use and cost-effectiveness.
Conclusion
Despite the advances made in bariatric surgery, the criteria determining suitability of patients for bariatric surgery in most parts of the world are still based on a consensus agreed upon in the USA in 1991. There is a need to formulate some new consensus and guidelines that would allow for a significant expansion of the pool of patients that can be offered these procedures.


















Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Buchwald H. Metabolic surgery: a brief history and perspective. Surg Obes Relat Dis. 2010;6:221–2.
Saber AA, Elgamal MH, McLeod MK. Bariatric surgery: the past, present and future. Obes Surg. 2008;18:121–8.
Martin LF. The evolution of surgery for morbid obesity. (2004). Obes Surg, 2004; 14:15–47.
Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, Himpens J, et al. IFSO Worldwide Survey 2016: Primary, endoluminal, and revisional procedures. Obesity Sugery. 2018;28:3783–94.
Pinchiera JC, Prince RA, Mason EE. Effect of bariatric surgery on erythromycin absorption. Am J Hosp Pharm. 198(38):232.
Scott HW Jr. Metabolic surgery for hyperlipidemia and atherosclerosis. American Journal of Surg. 1972;123:3–12.
Mahawar K. Gastric bypass is not a “restrictive and malabsorptive” procedure. Obes Surg. 2016;26:2225–6.
Stefanidis A, Oldfield BJ. Neuroendocrine mechanisms underlying bariatric surgery: insights from human studies and animal models. J Neuroendocrinol. 2017;29(10).
Buchwald H, Rucker RD. The rise and fall of jejunoileal bypass. In: Nelson RL, Nyhus, editors. Surgery of the small intestine. Norwalk, CT: Appleton Century Crofts; 1987; 529–41.
Printen KJ, Mason EE. Gastric surgery for relief of morbid obesity. Arch Surg. 1973;106:428–31.
Long M, Collins JP. The technique and early results of high gastric reduction for obesity. Aust N Z J Surg. 1980;50:146–9.
Mason EE. Vertical banded gastroplasty for obesity. Arch Surg. 1982;11:701–6.
Mason EE, Cullen JJ. Management of complications in vertical banded gastroplasty. Curr Surg. 2003;60(1):33–7.
Salinas A, Santiago E, Yeguez J, et al. Silastic ring vertical gastric bypass: evolution of an open surgical technique, and review of 1,588 cases. Obes Surg 2005;15:1403–1407.
Tretbar LL, Taylor TL, Sifers EC. Weight reduction. Gastric plication for morbid obesity. J Kans Med Soc. 1976;77:488–90.
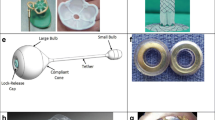
Kuzmak LI, Thelmo W, Abramson DL. Reversible adjustable gastric banding. Surgical technique. Eur J Surg. 1994;160:569–71.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2008. Obes Surg. 2009;19:1605–11.
Aarts EO, Dogan K, Koehestanie P, Aufenacker TJ, Janssen IMC, Berends FJ. Long term results after laparoscopic adjustable gastric banding: a mean fourteen year follow-up study. Surg Obes Relat Dis. 2014;24:1835–42.
Brown JJ, Boyle M, Mahawar K, Balupuri S, Small PK. Laparoscopic adjustable gastric band survival in a high-volume bariatric unit. Br J Surg. 2013;100:1614–8.
Marceau P, Biron S, Bourque RA, Potvin M, Hould FS, Simard S. Biliopancreatic diversion with a new type of gastrectomy. Obes Surg. 1993;3:29–35.
Langer FB, Bohdjalian A, Felberbauer FX, Fleischmann E, Reza Hoda M, Ludvik B, et al. Does gastric dilatation limit the success of sleeve gastrectomy as a sole operation for morbid obesity? Obes Surg. 2006;16:166–71.
Zhao H, Jiao L. Comparative analysis for the effect of Roux-en-Y gastric bypass vs sleeve gastrectomy in patients with morbid obesity: Evidence from 11 randomized clinical trials (meta-analysis). Int J Surg. 2019;72:216–23.
Gagner M. Hypoabsorption not malabsorption, hypoabsorptive surgery and not malabsorptive surgery. Obes Surg. 2016;26:2783–4.
Kral JG. Malabsorptive procedures in surgical treatment of morbid obesity. Gastroenterol Clin N Am. 1987;16:293–305.
Li W, Baraboi ED, Cluny NL, Roy MC, Samson P, Biertho L, et al. Malabsorption plays a major role in the effects of the biliopancreatic diversion with duodenal switch on energy metabolism in rats. Surg Obes Relat Dis. 2015;11:356–66.
Silecchia G, Boru C. Effectiveness of laparoscopic sleeve gastrectomy (first stage of biliopancreatic diversion with duodenal switch) on comorbidities in super-obese high-risk patients. Obes Surg. 2006;16:1138–44.
Scopinaro N, Gianetta E, Civalleri D, Bonalumi U, Bachi V Bilio-pancreatic bypass for obesity: II. Initial experience in man. Br J Surg 1979;66:618–620.
Scopinaro N, Gianetta E, Adami GF, Friedman D, Traverso E, Marinari GM, et al. Biliopancreatic diversion for obesity at eighteen years. Surgery. 1996;119:261–8.
Scopinaro N, Adami GF, Marinari GM, Gianetta E, Traverso E, Friedman D, et al. Biliopancreatic diversion. World J Surg. 1998;22:936–46.
Sánchez-Pernaute A, Herrera MA, Pérez-Aguirre ME, Talavera P, Cabrerizo L, Matía P, et al. Single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). One to three-year follow-up. Obes Surg. 2010;20:1720.
Martini F, Paolino L, Marzano E, D'Agostino J, Lazzati A, Schneck AS, et al. Single-anastomosis pylorus-preserving bariatric procedures: review of the literature. Obes Surg. 2016;26:2503–15.
Griffen WO Jr, Young VL, Stevenson CC. A prospective comparison of gastric and jejunoileal bypass procedures for morbid obesity. Ann Surg. 1977;186(4):500–9.
Wittgrove AC, Clark GW, Tremblay LJ. Laparoscopic gastric bypass, Roux-en-Y: preliminary report of five cases. Obes Surg. 1994;4:353–7.
Mahawar KK, Sharples AJ. Contribution of malabsorption to weight loss after Roux-en-Y gastric bypass: a systematic review. Obes Surg. 2017;8:2194–206.
• Mahawar KK, Parmar C, WRJ C, Jennings N, Schroeder N, Small PK. Impact of biliopancreatic limb length on severe protein-calorie malnutrition requiring revisional surgery after one anastomosis (mini) gastric bypass. J Minim Access Surg. 2018;14:37–43 This article clearly shows the downside of one of the hot topics of the moment; OAGB-MGB with a long biliopancreatic limb. Healthcare professionals should take care to prevent protein and micronutrient deficiencies with (too) long biliopancreatic limbs.
Boyle M, Mahawar K. One anastomosis gastric bypass performed with a 150-cm biliopancreatic limb delivers weight loss outcomes similar to those with a 200-cm biliopancreatic limb at 18–24 months. Obes Surg. 2019 [published online ahead of print].
De Luca M, Tie T, Ooi G, Higa K, Himpens J, Carbajo MA, et al. Mini gastric bypass-one anastomosis gastric bypass (MGB-OAGB)-IFSO position statement. Obes Surg. 2018;28:1188–206.
Foster MW, Gershuni VM, Tewksbury CM, Giri JS, Dumon KR, Rame JE, et al. Laparoscopic sleeve gastrectomy carries a lower perioperative mortality including sudden cardiac death over Roux-en-Y gastric bypass in patients with a prior cardiac history: an MBSAQIP analysis. Obes Surg. 2019 Dec;24 [Epub ahead of print].
Glass J, Chaudhry A, Zeeshan MS, Ramzan Z. New era: endoscopic treatment options in obesity–a paradigm shift. World J Gastroenterol. 2019;25:4567–79.
Ly HG, Dupont P, Van Laere K, Depoortere I, Tack J, Van Oudenhove L. Differential brain responses to gradual intragastric nutrient infusion and gastric balloon distension: a role for gut peptides? Neuroimage. 2017;144:101–12.
Bužga M, Evžen M, Pavel K, Tomáš K, Vladislava Z, Pavel Z, et al. Effects of the intragastric balloon MedSil on weight loss, fat tissue, lipid metabolism, and hormones involved in energy balance. Obes Surg. 2014;24:909–15.
Raftopoulos I, Giannakou A. The Elipse Balloon, a swallowable gastric balloon for weight loss not requiring sedation, anesthesia or endoscopy: a pilot study with 12-month outcomes. Surg Obes Relat Dis. 2017;13:1174–82.
Hedjoudje A, Abu Dayyeh BK, Cheskin LJ, Adam A, Neto MG, Badurdeen D, et al. Efficacy and safety of endoscopic sleeve gastroplasty: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2019;S1542-3565(19):30897–3.
Gys B, Plaeke P, Lamme B, Lafullarde T, Komen N, Beunis A, et al. Endoscopic gastric plication for morbid obesity: a systematic review and meta-analysis of published data over time. Obes Surg. 2019;29:3021–9.
Kumar N, Sullivan S, Thompson CC. The role of endoscopic therapy in obesity management: intragastric balloons and aspiration therapy. Diabetes Metab Syndr Obes. 2017;10:311–6.
Thompson CC, Abu Dayyeh BK, Kushner R, Sullivan S, Schorr AB, Amaro A, et al. Percutaneous gastrostomy device for the treatment of class II and class III obesity: results of a randomized controlled trial. Am J Gastroenterol. 2017;112:447–57.
• Betzel B, Cooiman MI, Aarts EO, Janssen IMC, Wahab PJ, Groenen MJM, et al. Clinical follow-up on weight loss, glycemic control, and safety aspects of 24 months of duodenal-jejunal bypass liner implantation. Surg Endosc. 2020;34:209–15 With many new techniques coming out to treat obesity, it is very important to look for the best risk-benefit ratios. Most often, the first results of new techniques are promising, very often there is hardly any follow-up published afterwards. This article is one of the few that shows disappointing medium term results of a device (Endobarrier) and reports on the downfalls and relapse of type two diabetes.
Betzel B, Homan J, Aarts EO, Janssen IMC, de Boer H, Wahab PJ, et al. Weight reduction and improvement in diabetes by the duodenal-jejunal bypass liner: a 198 patient cohort study. Surg Endosc. 2017;31:2881–91.
van Rijn S, Roebroek YGM, de Jonge C, Greve JWM, Bouvy ND. Effect of the EndoBarrier device: a 4-year follow-up of a multicenter randomized clinical trial. Obes Surg. 2019;29:1117–21.
Betzel B, Koehestanie P, Aarts EO, Dogan K, Homan J, Janssen IM, et al. Safety experience with the duodenal-jejunal bypass liner: an endoscopic treatment for diabetes and obesity. Gastrointest Endosc. 2015;82:845–52.
Poelemeijer YQM, Liem RL, Våge V, Mala T, Sundbom M, Ottosson J, et al. Perioperative outcomes of primary bariatric surgery in North-Western Europe: a pooled multinational registry analysis. Obes Surg. 2018;28:3916–22.
Mulier JP, Dillemans B. Anaesthetic factors affecting outcome after bariatric surgery, a retrospective levelled regression analysis. Obes Surg. 2019;29:1841–50.
Pouwels S, Buise MP, Twardowski P, Stepaniak PS, Proczko M. Obesity surgery and anesthesiology risks: a review of key concepts and related physiology. Obes Surg. 2019;29:2670–7.
Lemanu DP, Singh PP, Berridge K, et al. Randomized clinical trial of enhanced recovery versus standard care after laparoscopic sleeve gastrectomy. Br J Surg. 2013;100:482–9.
Dogan K, Kraaij L, Aarts EO, Hammink E, van Laarhoven CJ, Aufenacker TJ, et al. Fast-track bariatric surgery improves perioperative care and logistics compared to conventional care. Obes Surg. 2015 Jan;25:28–35.
Schijns W, Deenen MJ, Aarts EO, Homan J, Janssen IMC, Berends FJ, et al. The effect of obesity on anti-Xa concentrations in bariatric patients. Obes Surg. 2018;28:1997–2005.
Foster MW, Gershuni VM, Tewksbury CM, Giri JS, Dumon KR, Rame JE, et al. Laparoscopic sleeve gastrectomy carries a lower perioperative mortality including sudden cardiac death over Roux-en-Y gastric bypass in patients with a prior cardiac history: an MBSAQIP analysis. Obes Surg. 2019 Dec;24 [Epub ahead of print].
van Rijswijk AS, Moes DE, Geubbels N, Hutten BA, Acherman YIZ, van de Laar AW, et al. Can a laparoscopic Roux-en-Y gastric bypass be safely performed by surgical residents in a bariatric center-of-excellence? The learning curve of surgical residents in bariatric surgery. Surg Endosc. 2018;32:1012–20.
• Wehrtmann FS, de la Garza JR, Kowalewski KF, Schmidt MW, Müller K, Tapking C, et al. Learning curves of laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy in bariatric surgery: a systematic review and introduction of a standardization. Obes Surg. 2019; This article is of importance, while, although not the only one, it advocates something that will help comparing research in bariatric surgery in the future; standardization. The hardest thing nowadays is comparing between studies which makes it for example hard to actually compare outcomes of different surgeries performed. Although it will be hard to standardize everything, it would be a major step forward.
Ozsoy Z, Demir E. The evolution of bariatric surgery publications and global productivity: a bibliometric analysis. Obes Surg. 2018;28:1117–29.
Gastrointestinal surgery for severe obesity. Consens Statement. 1991: 9:1–20.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
Dr. Aarts has no conflicts of interest to disclose. Dr. Mahawar has been paid honoraria by Medtronic ®, Ethicon ®, Gore ®, Olympus ®, and various NHS Trusts in the United Kingdom for educational activities.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclaimer
Figures have all been drawn by Dr. E.O. Aarts and he holds current intellectual property.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on The Obesity Epidemic: Causes and Consequences
Rights and permissions
About this article
Cite this article
Aarts, E.O., Mahawar, K. From the Knife to the Endoscope—a History of Bariatric Surgery. Curr Obes Rep 9, 348–363 (2020). https://doi.org/10.1007/s13679-020-00382-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-020-00382-1