Abstract
Sleep disturbance is common in patients with chronic obstructive pulmonary disease (COPD) and can be due to the underlying respiratory impairment itself or arise from comorbid obstructive sleep apnea, insomnia or restless legs syndrome. Sleep is associated with several changes in respiratory physiology, including the cessation of behavioral input to respiratory drive, reduction of hypoxic and hypercapnic ventilatory responses and decrease in activity of accessory muscles of respiration. Nocturnal oxygen desaturation can develop in persons with moderate-severe COPD.
Similar content being viewed by others
Introduction
The term chronic obstructive pulmonary disease (COPD) refers to progressive, not fully reversible, airflow limitation due to injury to the small airways and alveoli from noxious particles or gases. Chronic obstructive pulmonary disease encompasses several distinct disorders, including chronic bronchitis (clinically defined as chronic productive cough for 3 months in each of two successive years) and emphysema (anatomically defined as abnormal, permanent enlargement of the airspaces distal to the terminal bronchioles). Patients with COPD often present with dyspnea, chronic cough or chest tightness. Complaints of nighttime symptoms are common in patients with COPD. However, the prevalence of the latter is difficult to establish since there is no uniform definition for “nocturnal symptoms.” It has been reported that the prevalence of sleep-related and nighttime symptoms may exceed 75 % in this patient group [1].
Respiratory physiology during sleep
Significant changes in the respiratory system occur during sleep. These factors alter respiratory physiology and modify the clinical manifestations of a number of pulmonary disorders, including chronic obstructive pulmonary disease (COPD).
Firstly, both metabolic (pH, PaO2 and PaCO2) and behavioral control of respiration are operational during wakefulness. Sleep abolishes the behavioral input to respiratory drive, leaving the latter under sole metabolic control. Secondly, hypoxic and hypercapnic ventilatory responses, upper airway dilator muscle tone, and activity of accessory muscles of respiration diminish during non-rapid eye movement (NREM) sleep compared to wakefulness, and decreases further during rapid eye movement (REM) sleep. Respiration relies mainly on the diaphragmatic muscles during REM sleep, a situation that is most problematic in patients with bilateral diaphragm paralysis. Hyperinflation in patients with COPD may also give rise to inefficiencies of diaphragm function, which will likewise become more clinically significant during REM sleep. The supine position assumed during sleep can result in significant alterations in respiratory mechanics due to anatomical changes of the ribcage and diaphragm [2]. Lastly, comorbid obesity or neuromuscular weakness can give rise to additional inefficiencies in thoraco-abdominal mechanical performance and load responsiveness.
Chemosensitivity to oxygen (O2) and carbon dioxide (CO2) falls at the onset of sleep [3, 4]. These physiologic changes generally result in falls in PaO2 by 2 to 12 mmHg and oxygen saturation (SaO2) by 2 % as well as an increase in PaCO2 by 2 to 8 mmHg during sleep compared to wakefulness in healthy individuals; these changes are due mostly to decreases in tidal volume and minute ventilation. Individuals with underlying pulmonary disorders commonly demonstrate greater aberrations in these blood gas parameters. For instance, patients with borderline or mild daytime hypoxemia can experience more profound degrees of oxygen (O2) desaturation during sleep. Another important change in pulmonary physiology during sleep is the development of periodic breathing with episodes of hypopneas and hyperpneas during stage 1 NREM sleep and an irregular pattern of respiration with variable respiratory rates and tidal volumes during REM sleep. Additionally, periodic breathing may re-emerge during phasic REM sleep. In contrast, respiration is relatively stable with regular frequency and amplitude of breathing during stage N3 NREM sleep.
Finally, both sleep-state dependent and circadian rhythm related factors are important to the development of certain pulmonary disorders. Activity of upper airway dilator muscles, such as genioglossus, tensor palatini and sternohyoid, maintain patency of the upper airways and prevent their collapse during inspiration; activity of these muscles is reduced during sleep and this, in turn, can produce obstructive sleep apnea (OSA) in predisposed individuals [5]. Obstructive sleep apnea, if present, can contribute to sleep disturbance, nocturnal hypoxemia and worsening of symptoms in patients with COPD. Restless legs syndrome (RLS), another highly prevalent sleep disorder, is worse in patients with COPD compared to healthy patients and can further disturb sleep. Nocturnal exacerbation of asthma-related symptoms is an important example of how sleep and circadian day-night rhythms change respiratory function. Circadian influences on airflow with lowest levels in the early morning are more pronounced in patients with asthma [6]. Factors related to sleep itself, including changes in the autonomic nervous system, with increased parasympathetic tone and decreased sympathetic activity compared to waking levels; lung capacity and inflammatory mediators are also important pathophysiologic mechanisms responsible for nocturnal worsening of asthma and, possibly, COPD as well.
Nocturnal oxygen desaturation
Patients with moderate to severe COPD may develop nocturnal O2 desaturation. Sleep-related hypoxemia occurs more frequently, lasts longer, and is generally more severe during REM sleep compared to NREM sleep. Furthermore, nocturnal O2 desaturation is generally more commonly associated with emphysema than with chronic bronchitis. Factors that predict nocturnal hypoxemia in stable COPD without comorbid daytime respiratory failure or OSA include lower daytime SaO2, higher diurnal PaCO2, lung dynamic hyperinflation, lower inspiratory capacity and smaller upper airway caliber [7]. Oxygen level during wakefulness is the major predictor of both mean and lowest SaO2 during sleep in COPD. Nocturnal oximetry should be considered for patients with moderate-to-severe COPD. In this population, a significant number of persons without sleep apnea (up to 38 % in one study of 128 patients with a mean forced expiratory volume in 1 s (FEV1) of 37 % of predicted and daytime PaO2 between 56 - 69 mmHg) had nocturnal O2 desaturation. An additional 16 % of nocturnal desaturators had evidence of sleep apnea [8••].
Hypoventilation is the most important mechanism responsible for sleep-related hypoxemia. Other possible causes for nighttime O2 desaturation are ventilation-perfusion mismatching, diminished lung volumes and comorbid OSA.
Sleep disturbance and insomnia
Prevalence of poor sleep quality among COPD patients is high. In one study, 70 % of patients with COPD reported having poor sleep quality (Pittsburgh Sleep Quality Index [PSQI] > 5) [9]. Patients frequently complain of sleep-related symptoms including insomnia (difficulty falling asleep, repetitive or early awakening or non-restorative sleep), excessive sleepiness and nightmares. They also tend to use hypnotics more frequently than healthy controls [10]. One study noted that the relative risk (95 % confidence interval [CI]) of sleep disorders was 1.82 (1.03 to 3.22) in COPD patients compared with control subjects. The incidence of sleep disorders and depression were significantly related to lower body mass index (BMI), greater dyspnea, poorer health-related quality of life (HRQOL), lower PaO2 and higher PaCO2 [11]. In a cross-sectional study, 27 % of patients with stable COPD described having insomnia associated with impaired daytime functioning. Higher prevalence of insomnia was associated with current tobacco use and frequent sadness/anxiety, whereas use of O2 supplementation was related to lower prevalence of insomnia. More importantly, insomnia correlated with worse QOL and more frequent daytime sleepiness [12•].
The frequency and severity of insomnia is dependent on the severity of respiratory symptoms. Compared to asymptomatic COPD patients, those with new or persistent cough, dyspnea or wheezing are more likely to develop new insomnia and persistent sleep disturbance [13]. Insomnia prevalence was related to the number of symptoms (cough or wheezing); in one report, insomnia was present in 28 % of asymptomatic patients, in 39 % of patients when either cough or wheezing is present, and in 53 % of patients having both symptoms [14]. Similar to that of the general population, insomnia is more common in women and older adults with COPD [13].
Sleep disturbance is predictive of incident COPD exacerbations, respiratory-related emergency health care utilization and mortality even after controlling for socio-demographic factors, BMI, baseline FEV1 and COPD Severity Score [15]. However, other investigators disagree. In one report, the presence of depression, but not sleep disorders, independently increased the risk of exacerbations and hospitalization among COPD patients [11].
Sleep disturbance also predicts poor general health-related QOL and poor disease-specific QOL in COPD patients. In addition to its associations with dyspnea severity and post-bronchodilator FEV1, health-related QOL measured using the Saint George's Respiratory Questionnaire is significantly related to quality of sleep [9]. A multivariate regression analysis reported that sleep quality was an independent predictor of both the Health Utilities Index 3 (general HRQOL measure) and the St George's scores (disease-specific QOL measure), accounting for 3 % and 5 %, respectively, of the scores. In this study, 75 % of patients had PSQI scores > 5, and 25 % reported excessive daytime sleepiness (Epworth Sleepiness Scale [ESS] > 9) [16]. After controlling for other contributing variables, including patient characteristics and physical activity, the presence of sleep disturbance, along with not living with a spouse and self-efficacy, predicted depression and accounted for 45 % of the variance [17].
Etiology of sleep disturbance
Sleep disturbance in COPD patients can arise from several factors, many of which may be present in the same individual. These include (a) age-related changes, including reductions in homeostatic sleep pressure and arousal threshold, (b) disease-specific factors, such as presence of cough, dyspnea and hypoxemia, (c) frequency and severity of acute exacerbations, (d) pharmacotherapy, (e) comorbid medical disorders, including depression or cardiovascular diseases, and (f) presence of sleep disorders, such as insomnia, OSA and RLS [6, 18]. Investigators have noted that predictors of poor sleep quality in COPD patients included the presence of cough and dyspnea, COPD severity, daytime PaO2, and need for medications, O2 therapy and hospital care [15, 19]. Other risk factors for poor sleep quality in COPD patients are severity of airflow obstruction and thoracic hyperinflation. Both total sleep time and sleep efficiency have been shown to correlate positively with FEV1 and length of the diaphragm's zone of apposition, and negatively with residual volume [20].
Overlap syndrome
Obstructive sleep apnea consists of repetitive episodes of complete cessation (apnea) or reduction (hypopnea) of airflow due to complete (apnea) or partial (hypopnea) upper airway obstruction occurring during sleep. Common clinical features of OSA include episodic snoring, witnessed apnea, excessive daytime sleepiness and insomnia. If left untreated, OSA can give rise to multi-systemic consequences, such as hypertension, ischemic heart disease, heart failure, cardiac arrhythmias, pulmonary hypertension, stroke, metabolic syndrome, insulin resistance, nocturia, depression and neurocognitive dysfunction. The term “overlap syndrome” refers to the presence of both COPD and OSA. Patients with overlap syndrome tend to have lower PaO2, higher PaCO2, and more elevated pulmonary artery (PA) pressures than those with isolated COPD.
The prevalence of OSA in COPD patients is similar to that in the general population. In patients with COPD, decreased pulmonary function is not an independent risk factor for OSA. One study found no correlation between FEV1% predicted and risk for OSA, total apnea hypopnea index (AHI), oxygen desaturation index (ODI), % time with SaO2 < 90 %, and mean SaO2 [21]. Conversely, the prevalence of COPD is comparable in groups with and without OSA. Nevertheless, since both OSA and COPD are highly prevalent, it is not uncommon to encounter both disorders in the same individual [22].
Patients with overlap syndrome not treated with continuous positive airway pressure (CPAP) have been shown to have an increased risk of death and hospitalization due to COPD exacerbation compared to patients with COPD alone. The higher cardiovascular mortality associated with the overlap syndrome might be explained, at least in part, by more extensive right ventricular (RV) remodeling in patients with comorbid OSA and COPD. In one study, patients with overlap syndrome had higher RV mass indices (RVMI) and reduced RV remodeling indices (ratio of RVMI and RV end-diastolic volume) than those with isolated COPD. The extent of RV remodeling correlated with severity of O2 desaturation [23]. Another study showed that the comorbid presence of COPD augments the increase in arterial stiffness resulting from OSA. Compared to OSA alone, patients with overlap syndrome had significantly higher brachial-ankle pulse wave velocity and plasma B-natriuretic peptide (BNP) levels. The investigators postulated that this further increase in arterial stiffness might also contribute to the increased cardiovascular risk seen in the overlap syndrome [24]. Survival is increased and hospitalizations are decreased with CPAP treatment [25, 26].
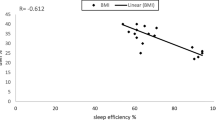
Lung hyperinflation (ratio of inspiratory capacity to total lung capacity) due to more severe pulmonary impairment in patients with overlap syndrome results in greater sleep disturbance and poorer sleep quality (i.e. lower sleep efficiency). This relationship remained significant after adjusting for BMI, AHI, FEV1% predicted and SaO2 nadir [27]. Lastly, OSA is associated with an elevated economic burden in patients with COPD, including higher medical service claims and higher medical costs compared to those without OSA [28].
Restless legs syndrome
Restless legs syndrome (RLS) is characterized by an unpleasant sensation or discomfort in the lower extremities (less commonly can also involve the arms) that occurs during rest, is worse at night, and is relieved transiently with movement of the affected limbs. An estimated 29 % to 36 % of patients with COPD may experience RLS-type symptoms and, in one study, up to 54 % of patients complain of RLS during acute exacerbations [29]. In another report, compared to healthy individuals, persons with COPD were more likely to have RLS (36 % vs. 11 %; P < 0.001), had more severe RLS symptoms (International Restless Legs Syndrome Study [IRLSS] severity scale score of 20.5 ± 2.8 vs. 18 ± 3.5; P = 0.016), and reported worse daytime sleepiness (ESS score of 11.8 ± 1.1 vs. 8.6 ± 3.6; P = 0.009) [30]. Patients with COPD and RLS symptoms have significantly higher PSQI scores compared to COPD patients without RLS [29]. Another study reported a prevalence rate of 30 % with 81 % of cases being of moderate-severe severity (IRLSS rating scale > 11). Patients with RLS reported poorer sleep quality (PSQI > 5 in 59 %), more fatigue (Fatigue Severity Scale, FSS > 27 in 51 %), greater depressive symptoms (Beck Depression Inventory, BDI-II >10 in 14.4 %) and more severe dyspnea [31].
The mechanisms responsible for these observations are unknown. Restless legs syndrome is believed to arise from defective central nervous system dopaminergic function; however, there is no reason to suspect that patients with COPD are more likely to develop this type of neurotransmitter imbalance than patients without COPD. Medication use may play a contributory role in some but not all patients. Lack of activity and immobility during the daytime have been postulated as a possible factor responsible for the higher prevalence and greater severity of RLS in COPD patients; these, however, are not applicable to all COPD patients with RLS. Diagnosis of RLS relies on a compatible clinical history as well as responsiveness to empiric dopaminergic agonist therapy. It is important to exclude medical disorders that could either mimic RLS symptoms (peripheral neuropathy, akathisia related to the use of neuroleptic agents or dopamine receptor antagonists, nocturnal leg cramps, and positional leg discomfort) or exacerbate its symptoms (anemia, diabetes, and renal failure).
Evaluation of sleep disturbance
Several validated questionnaires can assist in identifying the presence of sleep disturbance in patients with COPD. These include measures of sleepiness (Epworth Sleepiness Scale), fatigue (Fatigue Severity Scale), sleep quality (Pittsburgh Sleep Quality Index), OSA (Berlin or STOP-BANG questionnaires) and RLS (International Restless Legs Syndrome Study). Although polysomnography (PSG) is not indicated in persons with COPD, it should be considered in those with clinical symptoms suggestive of OSA, complications from unexplained hypoxemia, or pulmonary hypertension that is out of proportion to the degree of airflow limitation. Polysomnography, performed with diaphragm electromyogram and transcutaneous carbon dioxide monitoring, may also be used to help adjust ventilator settings in COPD patients who have marked morning deventilation dyspnea or unrewarded efforts during home nocturnal non-invasive bi-level positive pressure ventilation for chronic hypercapnic respiratory failure. In these patients, inappropriate ventilator settings may give rise to progressive hyperinflation, patient-ventilator asynchrony and ineffectual inspiratory efforts [32].
Sleep architecture may be normal or polysomnography may demonstrate prolonged sleep onset latency, decreased sleep efficiency, reduced total sleep time, more frequent sleep stage changes, arousals and awakenings, and less REM sleep [19, 33]. Portable sleep apnea testing is not recommended to diagnose OSA in COPD patients. Investigators have reported high recording failure rates using portable sleep testing in this population. However, for patients in whom data were analyzable, there was significant correlation between AHIs obtained from laboratory PSG and portable monitoring [34]. Similarly, concerns have been raised regarding the reliability of automated analysis of PSG data in COPD patients. Agreement between manual and computer-aided analysis using the Matrix Sleep Analysis software was poor in COPD patients for a number of sleep and respiratory parameters, including sleep latency, sleep efficiency, number of arousals, AHI and ODI [35].
Poor sleep architecture can also be apparent with actigraphy, which may show lower sleep efficiency and shorter sleep duration among COPD patients with insomnia [12•]. Chronic obstructive pulmonary disease may also be associated with other actigraphic findings, such as prolonged sleep onset latency and greater wake after sleep onset compared to non-COPD healthy controls. Severity of dyspnea may influence actigraphic measures sleep efficiency and total sleep time [36].
Overnight oximetry is recommended in COPD patients with daytime hypercapnia and/or hypoxemia, pulmonary and/or systemic hypertension or right heart failure. Oxygen saturation during a 6-min walk test (6MWT) helps to identify patients with COPD who might have significant nocturnal O2 desaturation. One group of investigators noted that when the lowest SaO2 during 6MWT was ≤ 88 %, 47 % of patients experienced an SaO2 < 90 % for ≥ 30 % of sleep time, yielding a positive likelihood ratio of 3.77 (95 % CI 1.87 to 7.62) compared with those with lowest SaO2 during 6MWT of > 88 % [37].
Treatment of sleep disturbance
The primary treatment goal for nighttime exacerbation of COPD symptoms and its accompanying sleep disturbance is better overall control of the underlying respiratory disorder. General measures such as smoking cessation and instructions on proper sleep hygiene are helpful. Long-acting beta-agonists, theophylline or long-acting anticholinergic agents can reduce nocturnal cough, dyspnea and wheezing, but might not necessarily improve nighttime sleep quality. Inhaled long-acting beta-agonist (salmeterol) therapy for COPD was noted to improve nocturnal SaO2 (both mean SaO2 and percentage of sleep spent with SaO2 < 90 %) and static lung volumes without significantly changing sleep quality [38].
Oxygen therapy is indicated for significant nocturnal oxygen desaturation. Although arousals are strongly associated with periods of O2 desaturation present during room air, O2 therapy to correct nocturnal hypoxemia has no consistent effect on sleep quality or frequency of arousals. It has been recommended to routinely increase O2 flow rate during the night compared to daytime values to avoid sleep-related hypoxemia. While this may increase nocturnal SaO2, it may also give rise to next-morning hypercapnia and acidosis in persons with severe COPD and chronic hypercapnic respiratory failure. Perhaps because of hypersensitivity to changes in ventilatory drive and pulmonary mechanics, COPD patients may be more likely to develop hypercapnia during O2 therapy for nocturnal oxygen desaturation. In one study, 21 % of clinical stable COPD patients with hypercapnic respiratory failure demonstrated nocturnal hypoventilation (i.e., increase in PaCO2 >10 mmHg compared to awake levels). In logistic regression analysis, higher BMI and lower diurnal increase of PaO2 after O2 administration were the variables that best discriminated this phenomenon [39]. Another study compared the effect of providing the COPD patients’ usual daytime O2 flow rates or an additional liter and showed that the latter improved nighttime SaO2, percentage of sleep time spent with SaO2 < 90 %, and PaO2 at awakening but resulted in worse hypercapnia and acidosis during the subsequent morning [40]. In the National Emphysema Treatment Trial, sleep quality and nocturnal O2 levels improved following lung volume reduction surgery in patients with emphysema [41].
Overlap syndrome generally requires positive airway pressure therapy or, less commonly, noninvasive ventilation. Oxygen supplementation can be provided as needed. It has been demonstrated that treatment of patients with overlap syndrome using CPAP can result in beneficial effects on daytime PaO2 and PaCO2, nocturnal SaO2, mean PA pressure, maximal inspiratory pressure and daytime sleepiness [42]. Positive airway pressure therapy can lower levels of inflammatory mediators, such as C-reactive protein, in patients with overlap syndrome [43]. Positive airway pressure therapy of OSA in hypoxemic COPD patients improves survival. In a prospective, cohort study, patients with overlap syndrome and chronic hypoxemia who were compliant with CPAP therapy had better survival compared to patients who were non-compliant to therapy (5-year survival rates of 71 % vs. 26 % [P < 0.01]). Risk of death was significantly lower among CPAP users (hazard ratio of death vs. nontreated patients of 0.19 [0.08 – 0.48]) [44]. In one randomized, crossover study comparing average volume assured pressure support (AVAPS) versus pressure support (PS) ventilation in patients with stable hypercapnic COPD, perceived sleep efficiency was better with AVAPS with no difference in usage or improvement in PaCO2 between the two modalities [45]. Although automatic continuous positive airway pressure (APAP) devices are not recommended for patients with COPD, some investigators have shown good results when the former were used to determine optimal fixed CPAP settings in patients with the overlap syndrome [46].
In COPD patients with respiratory failure treated with long-term non-invasive positive pressure ventilation, interruption of the latter led to increases in nocturnal transcutaneous CO2 and daytime blood gas bicarbonate in the short-term and increased daytime PaCO2 and worsened health status (St. George's Respiratory Questionnaire score) during long-term follow-up [47]. There appears to be no difference in sleep quality whether high (mean inspiratory positive airway pressure [IPAP] of 29 ± 4 mbar) or low (mean IPAP of 14 mbar) inspiratory pressures are selected for long-term non-invasive positive pressure ventilation; however, the former are more effective in maintaining alveolar ventilation in patients with hypercapnic COPD compared to lower pressures [48].
Cognitive behavioral therapy is effective for insomnia in patients with COPD, and has been demonstrated to improve insomnia severity, global sleep quality, beliefs and attitudes about sleep, sleep efficiency, wake after sleep onset, and fatigue [49]. Cognitive behavioral therapy of insomnia consists of various combinations of sleep restriction, cognitive therapy, stimulus control and relaxation techniques. Some patients may require short courses of hypnotic therapy. When starting pharmacotherapy, it is essential to use the lowest effective dose, regularly monitor drug efficacy and adverse effects, and adjust dosing with changes in clinical status. Dopaminergic agents are considered first-line therapy for RLS. Patients with mild RLS symptoms may benefit from counter stimulation, such as warm baths, massage or stretching. Anemia (serum ferritin < 50 ng/mL) should be corrected if present.
Conclusions
Nocturnal symptoms and sleep disturbance are common in patients with COPD. Diagnosis may be missed unless clinicians are vigilant of this and understands the indications for the use of different subjective and objective tests of sleep quality, sleepiness and sleep disorders. Effective therapy is available for most patients presenting with sleep disturbance.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Agusti A, Hedner J, Marin JM, Barbé F, Cazzola M, Rennard S. Night-time symptoms: a forgotten dimension of COPD. Eur Respir Rev. 2011;20(121):183–94.
Tusiewicz K, Moldofsky H, Bryan AC, Bryan MH. Mechanics of the rib cage and diaphragm during sleep. J Appl Physiol Respir Environ Exerc Physiol. 1977;43:600–2.
Douglas NJ, White DP, Weil JV, et al. Hypoxic ventilatory response decreases during sleep in normal men. Am Rev Respir Dis. 1982;125(3):286–9.
Douglas NJ, White DP, Weil JV, et al. Hypercapneic ventilatory response in sleeping adults. Am Rev Respir Dis. 1982;126(5):758–62.
Hudgel DW, Martin RJ, Johnson BJ, Hill P. Mechanics of the respiratory system and breathing pattern during sleep in normal humans. J Appl Physiol Respir Environ Exerc Physiol. 1984;56:133–7.
Greenberg H, Cohen RI. Nocturnal asthma. Curr Opin Pulm Med. 2012;18(1):57–62.
Corda L, Novali M, Montemurro LT, La Piana GE, Redolfi S, Braghini A, et al. Predictors of nocturnal oxyhemoglobin desaturation in COPD. Respir Physiol Neurobiol. 2011;179(2–3):192–7.
•• Lacasse Y, Sériès F, Vujovic-Zotovic N, Goldstein R, Bourbeau J, Lecours R, et al. Evaluating nocturnal oxygen desaturation in COPD–revised. Respir Med. 2011;105(9):1331–7. About a third of patients with moderate-severe COPD and no obstructive sleep apnea had nocturnal oxygen desaturation. Another 16 % of COPD with nocturnal hypoxemia had obstructive sleep apnea.
Nunes DM, Mota RM, de Pontes Neto OL, Pereira ED, de Bruin VM, de Bruin PF. Impaired sleep reduces quality of life in chronic obstructive pulmonary disease. Lung. 2009;187(3):159–63.
Cormick W, Olson LG, Hensley MJ, Saunders NA. Nocturnal hypoxaemia and quality of sleep in patients with chronic obstructive lung disease. Thorax. 1986;41(11):846–54.
Ito K, Kawayama T, Shoji Y, Fukushima N, Matsunaga K, Edakuni N, et al. Depression, but not sleep disorder, is an independent factor affecting exacerbations and hospitalization in patients with chronic obstructive pulmonary disease. Respirology. 2012;17(6):940–9.
• Budhiraja R, Parthasarathy S, Budhiraja P, Habib MP, Wendel C, Quan SF. Insomnia in patients with COPD. Sleep. 2012;35(3):369–75. Insomnia was reported by 27 % of patients with stable COPD and was associated with impaired daytime functioning, frequent daytime sleepiness and worse quality of life.
Dodge R, Cline MG, Quan SF. The natural history of insomnia and its relationship to respiratory symptoms. Arch Intern Med. 1995;155(16):1797–800.
Klink M, Quan SF. Prevalence of reported sleep disturbances in a general adult population and their relationship to obstructive airways diseases. Chest. 1987;91(4):540–6.
Omachi TA, Blanc PD, Claman DM, Chen H, Yelin EH, Julian L, et al. Disturbed sleep among COPD patients is longitudinally associated with mortality and adverse COPD outcomes. Sleep Med. 2012;13(5):476–83.
Scharf SM, Maimon N, Simon-Tuval T, Bernhard-Scharf BJ, Reuveni H, Tarasiuk A. Sleep quality predicts quality of life in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2010;6:1–12.
Lee H, Kim I, Lim Y, Jung HY, Park HK. Depression and sleep disturbance in patients with chronic obstructive pulmonary disease. Geriatr Nurs. 2011;32(6):408–17.
De S. Subjective assessment of quality of sleep in chronic obstructive pulmonary disease patient and its relationship with associated depression. Lung India. 2012;29(4):332–5.
McSharry DG, Ryan S, Calverley P, Edwards JC, McNicholas WT. Sleep quality in chronic obstructive pulmonary disease. Respirology. 2012;17(7):1119–24.
Krachman SL, Chatila W, Martin UJ, Permut I, D'Alonzo GE, Gaughan JP, et al. Physiologic correlates of sleep quality in severe emphysema. COPD. 2011;8(3):182–8.
Sharma B, Feinsilver S, Owens RL, Malhotra A, McSharry D, Karbowitz S. Obstructive airway disease and obstructive sleep apnea: effect of pulmonary function. Lung. 2011;189(1):37–41.
McNicholas WT. Chronic obstructive pulmonary disease and obstructive sleep apnea: overlaps in pathophysiology, systemic inflammation, and cardiovascular disease. Am J Respir Crit Care Med. 2009;180(8):692–700.
Sharma B, Neilan TG, Kwong RY, Mandry D, Owens RL, McSharry D, Bakker JP, Malhotra A. Evaluation of right ventricular remodeling using cardiac magnetic resonance imaging in co-existent chronic obstructive pulmonary disease and obstructive sleep apnea. COPD. 2012 Dec 28.
Shiina K, Tomiyama H, Takata Y, Yoshida M, Kato K, Nishihata Y, et al. Overlap syndrome: additive effects of COPD on the cardiovascular damages in patients with OSA. Respir Med. 2012;106(9):1335–41.
Marin JM, Soriano JB, Carrizo SJ, Boldova A, Celli BR. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am J Respir Crit Care Med. 2010;182(3):325–31.
Owens RL, Malhotra A. Sleep-disordered breathing and COPD: the overlap syndrome. Respir Care. 2010;55(10):1333–44.
Kwon JS, Wolfe LF, Lu BS, Kalhan R. Hyperinflation is associated with lower sleep efficiency in COPD with co-existent obstructive sleep apnea. COPD. 2009;6(6):441–5.
Shaya FT, Lin PJ, Aljawadi MH, Scharf SM. Elevated economic burden in obstructive lung disease patients with concomitant sleep apnea syndrome. Sleep Breath. 2009;13(4):317–23.
Aras G, Kadakal F, Purisa S, Kanmaz D, Aynaci A, Isik E. Are we aware of restless legs syndrome in COPD patients who are in an exacerbation period? Frequency and probable factors related to underlying mechanism. COPD. 2011;8(6):437–43.
Lo Coco D, Mattaliano A, Lo Coco A, Randisi B. Increased frequency of restless legs syndrome in chronic obstructive pulmonary disease patients. Sleep Med. 2009;10(5):572–6.
Cavalcante AG, de Bruin PF, de Bruin VM, Pereira ED, Cavalcante MM, Nunes DM, et al. Restless legs syndrome, sleep impairment, and fatigue in chronic obstructive pulmonary disease. Sleep Med. 2012;13(7):842–7.
Adler D, Perrig S, Takahashi H, Espa F, Rodenstein D, Pépin JL, et al. Polysomnography in stable COPD under non-invasive ventilation to reduce patient-ventilator asynchrony and morning breathlessness. Sleep Breath. 2012;16(4):1081–90.
Fleetham J, West P, Mezon B, Conway W, Roth T, Kryger M. Sleep, arousals, and oxygen desaturation in chronic obstructive pulmonary disease. The effect of oxygen therapy. Am Rev Respir Dis. 1982;126(3):429–33.
Oliveira MG, Nery LE, Santos-Silva R, Sartori DE, Alonso FF, Togeiro SM, et al. Is portable monitoring accurate in the diagnosis of obstructive sleep apnea syndrome in chronic pulmonary obstructive disease? Sleep Med. 2012;13(8):1033–8.
Stege G, Vos PJ, Dekhuijzen PN, Hilkens PH, van de Ven MJ, Heijdra YF, van den Elshout FJ. Manual vs. automated analysis of polysomnographic recordings in patients with chronic obstructive pulmonary disease. Sleep Breath. 2012 May 10.
Nunes DM, de Bruin VM, Louzada FM, Peixoto CA, Cavalcante AG, Castro-Silva C, de Bruin PF. Actigraphic assessment of sleep in chronic obstructive pulmonary disease. Sleep Breath. 2012 Feb 16.
Scott AS, Baltzman MA, Chan R, Wolkove N. Oxygen desaturation during a 6 min walk test is a sign of nocturnal hypoxemia. Can Respir J. 2011;18(6):333–7.
Ryan S, Doherty LS, Rock C, Nolan GM, McNicholas WT. Effects of salmeterol on sleeping oxygen saturation in chronic obstructive pulmonary disease. Respiration. 2010;79(6):475–81.
Tarrega J, Anton A, Guell R, Mayos M, Samolski D, Marti S, et al. Predicting nocturnal hypoventilation in hypercapnic chronic obstructive pulmonary disease patients undergoing long-term oxygen therapy. Respiration. 2011;82(1):4–9.
Samolski D, Tárrega J, Antón A, Mayos M, Martí S, Farrero E, et al. Sleep hypoventilation due to increased nocturnal oxygen flow in hypercapnic COPD patients. Respirology. 2010;15(2):283–8.
Krachman S, Minai OA, Scharf SM. Sleep abnormalities and treatment in emphysema. Proc Am Thorac Soc. 2008;5(4):536–42.
Toraldo DM, De Nuccio F, Nicolardi G. Fixed-pressure nCPAP in patients with obstructive sleep apnea (OSA) syndrome and chronic obstructive pulmonary disease (COPD): a 24-month follow-up study. Sleep Breath. 2010;14(2):115–23.
Nural S, Günay E, Halici B, Celik S, Unlü M. Inflammatory processes and effects of continuous positive airway pressure (CPAP) in overlap syndrome. Inflammation. 2012 Aug 11.
Machado MC, Vollmer WM, Togeiro SM, Bilderback AL, Oliveira MV, Leitão FS, et al. CPAP and survival in moderate-to-severe obstructive sleep apnoea syndrome and hypoxaemic COPD. Eur Respir J. 2010;35(1):132–7.
Crisafulli E, Manni G, Kidonias M, Trianni L, Clini EM. Subjective sleep quality during average volume assured pressure support (AVAPS) ventilation in patients with hypercapnic COPD: a physiological pilot study. Lung. 2009;187(5):299–305.
Guerrero A, Montserrat JM, Farre R, Masa F, Duran J, Embid C. Automatic CPAP performance in patients with sleep apnea plus COPD. COPD. 2012;9(4):382–9.
Oscroft NS, Quinnell TG, Shneerson JM, Smith IE. The effects of withdrawing long-term nocturnal non-invasive ventilation in COPD patients. COPD. 2010;7(2):111–6.
Dreher M, Ekkernkamp E, Walterspacher S, Walker D, Schmoor C, Storre JH, et al. Noninvasive ventilation in COPD: impact of inspiratory pressure levels on sleep quality. Chest. 2011;140(4):939–45.
Kapella MC, Herdegen JJ, Perlis ML, Shaver JL, Larson JL, Law JA, et al. Cognitive behavioral therapy for insomnia comorbid with COPD is feasible with preliminary evidence of positive sleep and fatigue effects. Int J Chron Obstruct Pulmon Dis. 2011;6:625–35.
Conflict of Interest
Teofilo Lee-Chiong has declared the following possible conflicts of interest: Chief Medical Liaison and research grants, Philips Respironics Consultant, Elsevier and CareCore National.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee-Chiong, T. Chronic obstructive pulmonary disease and sleep. Curr Respir Care Rep 2, 123–129 (2013). https://doi.org/10.1007/s13665-013-0048-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-013-0048-y