Abstract
Objective
Plasma glucose and insulin concentrations are clinical markers used to diagnose metabolic diseases, particularly prediabetes and diabetes. In this paper, we conducted a cluster analysis using plasma glucose and insulin data collected during both fasting and 2-h postprandial periods.
Methods
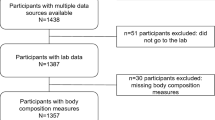
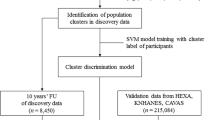
Different clustering experiments were performed by changing the attributes, from one (fasting glucose) to four (fasting and postprandial glucose and insulin) attributes input to a k-means clustering algorithm. Based on the elbow and silhouette methods, three clusters were chosen to perform the clustering experiments. The Pearson correlation coefficient was utilized to evaluate the association between the levels of glucose and insulin within each created cluster.
Results
Results show that one cluster comprised individuals with prediabetes, another cluster consisted of individuals with diabetes, while subjects without prediabetes and diabetes were assigned to a separate cluster. Despite not being used as an attribute, we observed varying age ranges among subjects in the three clusters. Furthermore, significant correlations were found between fasting and postprandial insulin levels, as well as between fasting and postprandial glucose levels, suggesting a consistent relationship between these variables, and highlighting their interdependence in the context of glucose metabolism.
Conclusion
The clustering analysis successfully differentiated individuals into distinct clusters based on their metabolic conditions, confirming that the approach effectively captured the underlying patterns in the plasma glucose and insulin data. Furthermore, despite not being a considered attribute, the varying age ranges observed within the clusters indicate that age may play a role in the development and progression of diabetes. Additionally, the fasting and postprandial associations in insulin and glucose levels exhibited greater strength in the cluster encompassing individuals with diabetes, where insulin production or action is compromised.
Similar content being viewed by others
Data availability
The dataset used in this study is freely available at https://ieee-dataport.org/documents/fasting-and-postprandial-glucose-and-insulin-dataset.
Code availability
The code used in this study is freely available at https://doi.org/10.24433/CO.7408455.v1 and at https://github.com/miguelaltuve/ClusterAnalysisBasedFastingPostprandialGlucoseInsulin.
References
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, Collins BS, Hilliard ME, Isaacs D, Johnson EL, Kahan S, Khunti K, Leon J, Lyons SK, Perry ML, Prahalad P, Pratley RE, Seley JJ, Stanton RC, Gabbay RA. 2. Classification and diagnosis of diabetes: standards of care in diabetes–2023. Diabetes Care. 2023;46:19–40. https://doi.org/10.2337/dc23-S002.
Fonseca VA. Defining and characterizing the progression of type 2 diabetes. Diabetes Care. 2009;32(suppl 2):151–6. https://doi.org/10.2337/dc09-S301.
Bansal N. Prediabetes diagnosis and treatment: a review. World J Diabetes. 2015;6(2):296–303. https://doi.org/10.4239/wjd.v6.i2.296.
Huang Y, Cai X, Mai W, Li M, Hu Y. Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. BMJ. 2016;355:5953. https://doi.org/10.1136/bmj.i5953.
Hulman A, Vistisen D, Glümer C, Bergman M, Witte DR, Færch K. Glucose patterns during an oral glucose tolerance test and associations with future diabetes, cardiovascular disease and all-cause mortality rate. Diabetologia. 2018;61(1):101–7. https://doi.org/10.1007/s00125-017-4468-z.
Cho N, Shaw J, Karuranga S, Huang Y, da Rocha Fernandes J, Ohlrogge A, Malanda B. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81. https://doi.org/10.1016/j.diabres.2018.02.023.
Yip W, Sequeira I, Plank L, Poppitt S. Prevalence of pre-diabetes across ethnicities: a review of impaired fasting glucose (IFG) and impaired glucose tolerance (IGT) for classification of dysglycaemia. Nutrients. 2017;9(11):1273. https://doi.org/10.3390/nu9111273.
Shakeel PM, Baskar S, Dhulipala VS, Jaber MM. Cloud based framework for diagnosis of diabetes mellitus using K-means clustering. Health Inf Sci Syst. 2018;6(1):16. https://doi.org/10.1007/s13755-018-0054-0.
Santhanam T, Padmavathi M. Application of K-means and genetic algorithms for dimension reduction by integrating SVM for diabetes diagnosis. Procedia Comput Sci. 2015;47:76–83. https://doi.org/10.1016/j.procs.2015.03.185.
Wildberg C, Masuch A, Budde K, Kastenmüller G, Artati A, Rathmann W, Adamski J, Kocher T, Völzke H, Nauck M, et al. Plasma metabolomics to identify and stratify patients with impaired glucose tolerance. J Clin Endocrinol Metab. 2019. https://doi.org/10.1210/jc.2019-01104.
Cahn A, Shoshan A, Sagiv T, Yesharim R, Raz I, Goshen R. Use of a machine learning algorithm improves prediction of progression to diabetes. American Diabetes Association. 2018. https://doi.org/10.2337/db18-1286-P.
Ahlqvist E, Storm P, Käräjämäki A, Martinell M, Dorkhan M, Carlsson A, Vikman P, Prasad RB, Aly DM, Almgren P, et al. Novel subgroups of adult-onset diabetes and their association with outcomes: a data-driven cluster analysis of six variables. Lancet Diabetes Endocrinol. 2018;6(5):361–9. https://doi.org/10.1016/S2213-8587(18)30051-2.
Altuve M, Severeyn E. Joint analysis of fasting and postprandial plasma glucose and insulin concentrations in Venezuelan women. Diabetes Metab Syndr: Clin Res Rev. 2019;13(3):2242–8. https://doi.org/10.1016/j.dsx.2019.05.029.
Altuve M, Severeyn E. Fasting and postprandial glucose and insulin dataset. IEEE Dataport. 2019. https://doi.org/10.21227/5g52-jc59
Bandodkar AJ, Imani S, Nunez-Flores R, Kumar R, Wang C, Mohan AV, Wang J, Mercier PP. Re-usable electrochemical glucose sensors integrated into a smartphone platform. Biosens Bioelectron. 2018;101:181–7. https://doi.org/10.1016/j.bios.2017.10.019.
Yang J. Blood glucose monitoring with smartphone as glucometer. Electrophoresis. 2019;40(8):1144–7. https://doi.org/10.1002/elps.201800295.
Farandos NM, Yetisen AK, Monteiro MJ, Lowe CR, Yun SH. Contact lens sensors in ocular diagnostics. Adv Healthc Mater. 2015;4(6):792–810. https://doi.org/10.1002/adhm.201400504.
Badugu R, Reece EA, Lakowicz JR. Glucose-sensitive silicone hydrogel contact lens toward tear glucose monitoring. J Biomed Opt. 2018;23(5):057005. https://doi.org/10.1117/1.JBO.23.5.057005.
Altuve M. Cluster analysis based on fasting and postprandial plasma glucose and insulin concentrations [Source Code]. 2024. https://doi.org/10.24433/CO.7408455.v1
Altuve M. Cluster analysis based on fasting and postprandial plasma glucose and insulin concentrations [Source Code]. 2024. https://github.com/miguelaltuve/ClusterAnalysisBasedFastingPostprandialGlucoseInsulin
Ha KH, Kim DJ. Trends in the diabetes epidemic in Korea. Endocrinol Metab. 2015;30(2):142–6. https://doi.org/10.3803/EnM.2015.30.2.142.
Czech MP. Insulin action and resistance in obesity and type 2 diabetes. Nat Med. 2017;23(7):804–14. https://doi.org/10.1038/nm.4350.
Muller D, Elahi D, Tobin J, Andres R. The effect of age on insulin resistance and secretion: a review. Semin Nephrol. 1996;16(4):289–98.
Johnson JD. On the causal relationships between hyperinsulinaemia, insulin resistance, obesity and dysglycaemia in type 2 diabetes. Diabetologia. 2021;64:2138–46. https://doi.org/10.1007/s00125-021-05505-4.
DeFronzo RA, Ferrannini E, Groop L, Henry RR, Herman WH, Holst JJ, Hu FB, Kahn CR, Raz I, Shulman GI, et al. Type 2 diabetes mellitus. Nat Rev Dis Primers. 2015;1:15019. https://doi.org/10.1038/nrdp.2015.19.
Padhi S, Nayak AK, Behera A. Type II diabetes mellitus: a review on recent drug based therapeutics. Biomed Pharmacother. 2020;131:110708. https://doi.org/10.1016/j.biopha.2020.110708.
Halban PA, Polonsky KS, Bowden DW, Hawkins MA, Ling C, Mather KJ, Powers AC, Rhodes CJ, Sussel L, Weir GC. \(\beta \)-cell failure in type 2 diabetes: postulated mechanisms and prospects for prevention and treatment. J Clin Endocrinol Metab. 2014;99(6):1983–92. https://doi.org/10.1210/jc.2014-1425.
Hall C, Yu H, Choi E. Insulin receptor endocytosis in the pathophysiology of insulin resistance. Exp Mol Med. 2020;52(6):911–20. https://doi.org/10.1038/s12276-020-0456-3.
Balsan GA, Vieira JLdC, Oliveira AMd, Portal VL. Relationship between adiponectin, obesity and insulin resistance. Rev Assoc Med Bras. 2015;61:72–80. https://doi.org/10.1590/1806-9282.61.01.072.
Yaribeygi H, Atkin SL, Simental-Mendía LE, Sahebkar A. Molecular mechanisms by which aerobic exercise induces insulin sensitivity. J Cell Physiol. 2019;234(8):12385–92. https://doi.org/10.1002/jcp.28066.
Ketema EB, Kibret KT. Correlation of fasting and postprandial plasma glucose with hba1c in assessing glycemic control; systematic review and meta-analysis. Arch Pub Health. 2015;73(1):43. https://doi.org/10.1186/s13690-015-0088-6.
Author information
Authors and Affiliations
Contributions
Miguel Altuve carried out the experiments and contributed to the conception of the study and the writing and revising of the manuscript. Erika Severeyn contributed to the conception of the study, the analysis of the results, and the writing and revising of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
All the procedures performed in the study were adjusted to the ethical standards of the University Hospital of Caracas and the Declaration of Helsinki of 1964 and its subsequent amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Altuve, M., Severeyn, E. Cluster analysis based on fasting and postprandial plasma glucose and insulin concentrations. Int J Diabetes Dev Ctries (2024). https://doi.org/10.1007/s13410-024-01322-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13410-024-01322-8