Abstract
Ulcerative colitis (UC) is an idiopathic, chronic, relapsing disease. In most cases, only the distal colon is affected, and the colonic stasis or fast colonic transit through the inflamed colon usually results in reduced exposure of the distal inflamed colon. Although the immunosuppressant cyclosporine A (CsA) has been used in patients with severe colitis who do not respond to corticosteroids, the clinical application of CsA remains limited due to the systemic toxicities and insufficient accumulation at the site of action for the intravenous and oral routes. In this study, we loaded CsA into the amphipathic poly(ethylene glycol)-poly(ε-caprolactone) (PEG-PCL) micelles and then embedded them in hydrogels consisting of chitosan, poloxamer 188, and poloxamer 407 to construct a thermosensitive and mucoadhesive hydrogel drug delivery system (PLCP). The PLCP presented a high drug-loading capacity and showed a stable and rapid gelation rate after rectal administration into the body. Compared to CsA-loaded micelles and Sandimmun (Neoral®), the developed thermosensitive gel exhibited prolonged retention on the inflamed colon, as seen from in vitro adhesion and in vivo distribution experiments. It also fast mitigated colitis symptoms in TNBS-treated mice by regulating the expression levels of proinflammatory cytokines (TNF-α, IL-1β, COX-2, and iNOS2), anti-inflammatory cytokines (IL-10, Nrf2, NQO1, and HO-1), and other relevant biochemical factors. Our results suggested that CsA-loaded micelle thermal hydrogel system could be a promising strategy by enhancing the retention in the diseased colon and promoting the relief and recovery of UC.
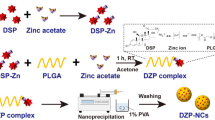
Graphical Abstract








Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this published article.
References
Shibolet O, Regushevskaya E, Brezis M, Soares-Weiser K. Cyclosporine A for induction of remission in severe ulcerative colitis. Cochrane Database Syst Rev. 2005(1):CD004277. https://doi.org/10.1002/14651858.CD004277.pub2.
Hindryckx P, Jairath V, D’Haens G. Acute severe ulcerative colitis: from pathophysiology to clinical management. Nat Rev Gastroenterol Hepatol. 2016;13(11):654–64. https://doi.org/10.1038/nrgastro.2016.116.
Zhang Y, Li X, Zhou Y, Fan Y, Wang X, Huang Y, et al. Cyclosporin A-loaded poly(ethylene glycol)-b-poly(d, l-lactic acid) micelles: preparation, in vitro and in vivo characterization and transport mechanism across the intestinal barrier. Mol Pharm. 2010;7(4):1169–82. https://doi.org/10.1021/mp100033k.
Fukata N, Uchida K, Kusuda T, Koyabu M, Miyoshi H, Fukui T, et al. The effective therapy of cyclosporine A with drug delivery system in experimental colitis. J Drug Target. 2011;19(6):458–67. https://doi.org/10.3109/1061186X.2010.511224.
Guada M, Beloqui A, Alhouayek M, Muccioli GG, Dios-Vieitez Mdel C, Preat V, et al. Cyclosporine A-loaded lipid nanoparticles in inflammatory bowel disease. Int J Pharm. 2016;503(1–2):196–8. https://doi.org/10.1016/j.ijpharm.2016.03.012.
Kornbluth A. Cyclosporine in inflammatory bowel disease. Curr Gastroenterol Rep. 1999;1(6):486–90. https://doi.org/10.1007/s11894-999-0008-4.
Guada M, Lana H, Gil AG, Dios-Vieitez Mdel C, Blanco-Prieto MJ. Cyclosporine A lipid nanoparticles for oral administration: pharmacodynamics and safety evaluation. Eur J Pharm Biopharm. 2016;101:112–8. https://doi.org/10.1016/j.ejpb.2016.01.011.
Zhang Y, Chen D, Wang F, Li X, Xue X, Jiang M et al. Comparison of the efficiency of different enemas on patients with distal ulcerative colitis. Cell Prolif. 2019;52(2):e12559. https://doi.org/10.1111/cpr.12559.
Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel J-F. Ulcerative colitis. The Lancet. 2017;389(10080):1756–70. https://doi.org/10.1016/s0140-6736(16)32126-2.
Lawrance IC. Topical agents for idiopathic distal colitis and proctitis. J Gastroenterol Hepatol. 2011;26(1):36–43. https://doi.org/10.1111/j.1440-1746.2010.06497.x.
Zhai J, Mantaj J, Vllasaliu D. Ascorbyl palmitate hydrogel for local, intestinal delivery of macromolecules. Pharmaceutics. 2018;10(4). https://doi.org/10.3390/pharmaceutics10040188.
Xu J, Strandman S, Zhu JX, Barralet J, Cerruti M. Genipin-crosslinked catechol-chitosan mucoadhesive hydrogels for buccal drug delivery. Biomaterials. 2015;37:395–404. https://doi.org/10.1016/j.biomaterials.2014.10.024.
Zhang M, Xu C, Liu D, Han MK, Wang L, Merlin D. Oral delivery of nanoparticles loaded with ginger active compound, 6-Shogaol, attenuates ulcerative colitis and promotes wound healing in a murine model of ulcerative colitis. J Crohns Colitis. 2018;12(2):217–29. https://doi.org/10.1093/ecco-jcc/jjx115.
Marshall JK, Irvine EJ. Putting rectal 5-aminosalicylic acid in its place: the role in distal ulcerative colitis. Am J Gastroenterol. 2000;95(7):1628–36. https://doi.org/10.1111/j.1572-0241.2000.02180.x.
Frei P, Biedermann L, Manser CN, Wilk M, Manz M, Vavricka SR, et al. Topical therapies in inflammatory bowel disease. Digestion. 2012;86(Suppl 1):36–44. https://doi.org/10.1159/000341947.
Zhang S, Langer R, Traverso G. Nanoparticulate drug delivery systems targeting inflammation for treatment of inflammatory bowel disease. Nano Today. 2017;16:82–96. https://doi.org/10.1016/j.nantod.2017.08.006.
Torchilin VP. Multifunctional, stimuli-sensitive nanoparticulate systems for drug delivery. Nat Rev Drug Discov. 2014;13(11):813–27. https://doi.org/10.1038/nrd4333.
Qiu L, Li Q, Huang J, Wu Q, Tu K, Wu Y, et al. In vitro effect of mPEG(2k)-PCL(x) micelles on rat liver cytochrome P450 enzymes. Int J Pharm. 2018;552(1–2):99–110. https://doi.org/10.1016/j.ijpharm.2018.09.052.
Dufort S, Sancey L, Coll JL. Physico-chemical parameters that govern nanoparticles fate also dictate rules for their molecular evolution. Adv Drug Deliv Rev. 2012;64(2):179–89. https://doi.org/10.1016/j.addr.2011.09.009.
Cereijido M, Contreras RG, Flores-Benitez D, Flores-Maldonado C, Larre I, Ruiz A, et al. New diseases derived or associated with the tight junction. Arch Med Res. 2007;38(5):465–78. https://doi.org/10.1016/j.arcmed.2007.02.003.
Pullan RD, Thomas GA, Rhodes M, Newcombe RG, Williams GT, Allen A, et al. Thickness of adherent mucus gel on colonic mucosa in humans and its relevance to colitis. Gut. 1994;35(3):353–9. https://doi.org/10.1136/gut.35.3.353.
Xia W, Liu P, Zhang J, Chen J. Biological activities of chitosan and chitooligosaccharides. Food Hydrocoll. 2011;25(2):170–9. https://doi.org/10.1016/j.foodhyd.2010.03.003.
Xu J, Tam M, Samaei S, Lerouge S, Barralet J, Stevenson MM, et al. Mucoadhesive chitosan hydrogels as rectal drug delivery vessels to treat ulcerative colitis. Acta Biomater. 2017;48:247–57. https://doi.org/10.1016/j.actbio.2016.10.026.
Bobbala S, Gibson B, Gamble AB, McDowell A, Hook S. Poloxamer 407-chitosan grafted thermoresponsive hydrogels achieve synchronous and sustained release of antigen and adjuvant from single-shot vaccines. Immunol Cell Biol. 2018;96(6):656–65. https://doi.org/10.1111/imcb.12031.
Sun J, Jiang G, Wang Y, Ding F. Thermosensitive chitosan hydrogel for implantable drug delivery: blending PVA to mitigate body response and promote bioavailability. J Appl Polym Sci. 2012;125(3):2092–101. https://doi.org/10.1002/app.36297.
Qu J, Zhao X, Liang Y, Zhang T, Ma PX, Guo B. Antibacterial adhesive injectable hydrogels with rapid self-healing, extensibility and compressibility as wound dressing for joints skin wound healing. Biomaterials. 2018;183:185–99. https://doi.org/10.1016/j.biomaterials.2018.08.044.
Cafaggi S, Russo E, Caviglioli G, Parodi B, Stefani R, Sillo G, et al. Poloxamer 407 as a solubilising agent for tolfenamic acid and as a base for a gel formulation. Eur J Pharm Sci. 2008;35(1–2):19–29. https://doi.org/10.1016/j.ejps.2008.05.010.
Dumortier G, Grossiord JL, Agnely F, Chaumeil JC. A review of poloxamer 407 pharmaceutical and pharmacological characteristics. Pharm Res. 2006;23(12):2709–28. https://doi.org/10.1007/s11095-006-9104-4.
Li Q, Sun M, Li G, Qiu L, Huang Z, Gong J, et al. The sub-chronic impact of mPEG2k-PCLx polymeric nanocarriers on cytochrome P450 enzymes after intravenous administration in rats. Eur J Pharm Biopharm. 2019;142:101–13. https://doi.org/10.1016/j.ejpb.2019.06.017.
Wu Y, Sun M, Wang D, Li G, Huang J, Tan S, et al. A PepT1 mediated medicinal nano-system for targeted delivery of cyclosporine A to alleviate acute severe ulcerative colitis. Biomater Sci. 2019;7(10):4299–309. https://doi.org/10.1039/c9bm00925f.
Xiao B, Zhang Z, Viennois E, Kang Y, Zhang M, Han MK, et al. Combination therapy for ulcerative colitis: orally targeted nanoparticles prevent mucosal damage and relieve inflammation. Theranostics. 2016;6(12):2250–66. https://doi.org/10.7150/thno.15710.
Te Velde AA, Verstege MI, Hommes DW. Critical appraisal of the current practice in murine TNBS-induced colitis. Inflamm Bowel Dis. 2006;12(10):995–9. https://doi.org/10.1097/01.mib.0000227817.54969.5e.
Zhang T, Mei Y, Dong W, Wang J, Huang F, Wu J. Evaluation of protein arginine deiminase-4 inhibitor in TNBS- induced colitis in mice. Int Immunopharmacol. 2020;84:106583. https://doi.org/10.1016/j.intimp.2020.106583.
Murano M, Maemura K, Hirata I, Toshina K, Nishikawa T, Hamamoto N, et al. Therapeutic effect of intracolonically administered nuclear factor kappa B (p65) antisense oligonucleotide on mouse dextran sulphate sodium (DSS)-induced colitis. Clin Exp Immunol. 2000;120(1):51–8. https://doi.org/10.1046/j.1365-2249.2000.01183.x.
Dieleman LA, Palmen MJ, Akol H, Bloemena E, Peña AS, Meuwissen SG, et al. Chronic experimental colitis induced by dextran sulphate sodium (DSS) is characterized by Th1 and Th2 cytokines. Clin Exp Immunol. 1998;114(3):385–91. https://doi.org/10.1046/j.1365-2249.1998.00728.x.
Wang D, Sun M, Zhang Y, Chen Z, Zang S, Li G et al. Enhanced therapeutic efficacy of a novel colon-specific nanosystem loading emodin on DSS-induced experimental colitis. Phytomedicine. 2020;78:153293. https://doi.org/10.1016/j.phymed.2020.153293.
Seelig J. Thermodynamics of lipid-peptide interactions. Biochim Biophys Acta. 2004;1666(1–2):40–50. https://doi.org/10.1016/j.bbamem.2004.08.004.
Hua S, Marks E, Schneider JJ, Keely S. Advances in oral nano-delivery systems for colon targeted drug delivery in inflammatory bowel disease: selective targeting to diseased versus healthy tissue. Nanomedicine. 2015;11(5):1117–32. https://doi.org/10.1016/j.nano.2015.02.018.
Giuliano E, Paolino D, Fresta M, Cosco D. Drug-loaded biocompatible nanocarriers embedded in poloxamer 407 hydrogels as therapeutic formulations. Medicines (Basel). 2018;6(1). https://doi.org/10.3390/medicines6010007.
Kolawole OM, Cook MT. In situ gelling drug delivery systems for topical drug delivery. Eur J Pharm Biopharm. 2023;184:36–49. https://doi.org/10.1016/j.ejpb.2023.01.007.
Liu Y, Yang T, Wei S, Zhou C, Lan Y, Cao A, et al. Mucus adhesion- and penetration-enhanced liposomes for paclitaxel oral delivery. Int J Pharm. 2018;537(1–2):245–56. https://doi.org/10.1016/j.ijpharm.2017.12.044.
Neurath MF, Fuss I, Kelsall BL, Stüber E, Strober W. Antibodies to interleukin 12 abrogate established experimental colitis in mice. J Exp Med. 1995;182(5):1281–90. https://doi.org/10.1084/jem.182.5.1281.
Low D, Nguyen DD, Mizoguchi E. Animal models of ulcerative colitis and their application in drug research. Drug Des Devel Ther. 2013;7:1341–57. https://doi.org/10.2147/dddt.S40107.
Valatas V, Bamias G, Kolios G. Experimental colitis models: insights into the pathogenesis of inflammatory bowel disease and translational issues. Eur J Pharmacol. 2015;759:253–64. https://doi.org/10.1016/j.ejphar.2015.03.017.
TM MW, Lau WM, Khutoryanskiy VV. Chitosan and its derivatives for application in mucoadhesive drug delivery systems. Polymers (Basel). 2018;10(3). https://doi.org/10.3390/polym10030267.
Huang J, Mei Q, Han L, Liu X-c, Diao L, Chen M-l et al. Effect of cyclosporin A on the intestinal mucosal permeability of colitis in mice. Chin Pharmacol Bull. 2012;28(10):1468–71. https://doi.org/10.3969/j.issn.1001-1978.2012.10.032.
Keane TJ, Dziki J, Sobieski E, Smoulder A, Castleton A, Turner N, et al. Restoring mucosal barrier function and modifying macrophage phenotype with an extracellular matrix hydrogel: potential therapy for ulcerative colitis. J Crohns Colitis. 2017;11(3):360–8. https://doi.org/10.1093/ecco-jcc/jjw149.
Wang J, Su L, Zhang L, Zeng J, Chen Q, Deng R, et al. Spirulina platensis aqueous extracts ameliorate colonic mucosal damage and modulate gut microbiota disorder in mice with ulcerative colitis by inhibiting inflammation and oxidative stress. J Zhejiang Univ Sci B. 2022;23(6):481–501. https://doi.org/10.1631/jzus.B2100988.
Swindle EJ, Metcalfe DD. The role of reactive oxygen species and nitric oxide in mast cell-dependent inflammatory processes. Immunol Rev. 2007;217:186–205. https://doi.org/10.1111/j.1600-065X.2007.00513.x.
Tian T, Wang Z, Zhang J. Pathomechanisms of oxidative stress in inflammatory bowel disease and potential antioxidant therapies. Oxid Med Cell Longev. 2017;2017:4535194. https://doi.org/10.1155/2017/4535194.
Zanoni I, Foti M, Ricciardi-Castagnoli P, Granucci F. TLR-dependent activation stimuli associated with Th1 responses confer NK cell stimulatory capacity to mouse dendritic cells. J Immunol. 2005;175(1):286–92. https://doi.org/10.4049/jimmunol.175.1.286.
Kulkarni AC, Kuppusamy P, Parinandi N. Oxygen, the lead actor in the pathophysiologic drama: enactment of the trinity of normoxia, hypoxia, and hyperoxia in disease and therapy. Antioxid Redox Signal. 2007;9(10):1717–30. https://doi.org/10.1089/ars.2007.1724.
Jump RL, Levine AD. Mechanisms of natural tolerance in the intestine: implications for inflammatory bowel disease. Inflamm Bowel Dis. 2004;10(4):462–78. https://doi.org/10.1097/00054725-200407000-00023.
Papadakis KA, Targan SR. Role of cytokines in the pathogenesis of inflammatory bowel disease. Annu Rev Med. 2000;51:289–98. https://doi.org/10.1146/annurev.med.51.1.289.
McDaniel DK, Eden K, Ringel VM, Allen IC. Emerging roles for noncanonical NF-kappaB signaling in the modulation of inflammatory bowel disease pathobiology. Inflamm Bowel Dis. 2016;22(9):2265–79. https://doi.org/10.1097/MIB.0000000000000858.
Taniguchi K, Karin M. NF-κB, inflammation, immunity and cancer: coming of age. Nat Rev Immunol. 2018;18(5):309–24. https://doi.org/10.1038/nri.2017.142.
Wang Y, Tang Q, Duan P, Yang L. Curcumin as a therapeutic agent for blocking NF-kappaB activation in ulcerative colitis. Immunopharmacol Immunotoxicol. 2018;40(6):476–82. https://doi.org/10.1080/08923973.2018.1469145.
Nakahara C, Nakamura K, Yamanaka N, Baba E, Wada M, Matsunaga H, et al. Cyclosporin-A enhances docetaxel-induced apoptosis through inhibition of nuclear factor-kappaB activation in human gastric carcinoma cells. Clin Cancer Res. 2003;9(14):5409–16.
Sabat R, Grutz G, Warszawska K, Kirsch S, Witte E, Wolk K, et al. Biology of interleukin-10. Cytokine Growth Factor Rev. 2010;21(5):331–44. https://doi.org/10.1016/j.cytogfr.2010.09.002.
Li W, Khor TO, Xu C, Shen G, Jeong WS, Yu S, et al. Activation of Nrf2-antioxidant signaling attenuates NFkappaB-inflammatory response and elicits apoptosis. Biochem Pharmacol. 2008;76(11):1485–9. https://doi.org/10.1016/j.bcp.2008.07.017.
Pandurangan AK, Saadatdoust Z, Esa NM, Hamzah H, Ismail A. Dietary cocoa protects against colitis-associated cancer by activating the Nrf2/Keap1 pathway. BioFactors. 2015;41(1):1–14. https://doi.org/10.1002/biof.1195.
Strober W, Lúdvíksson BR, Fuss IJ. The pathogenesis of mucosal inflammation in murine models of inflammatory bowel disease and Crohn disease. Ann Intern Med. 1998;128(10):848–56. https://doi.org/10.7326/0003-4819-128-10-199805150-00009.
Granucci F, Zanoni I, Pavelka N, Van Dommelen SL, Andoniou CE, Belardelli F, et al. A contribution of mouse dendritic cell-derived IL-2 for NK cell activation. J Exp Med. 2004;200(3):287–95. https://doi.org/10.1084/jem.20040370.
Acknowledgements
The authors appreciate the staff from the Analysis and Testing Center of Huazhong University of Science and Technology for their technical assistance.
Author information
Authors and Affiliations
Contributions
Project administration and conceptualization: L Q Si and M H Sun; methodology and investigation: C Y Xiao, G Y Li, X Y Li, and D Wang; data collection and analysis: C Y Xiao, G Y Li, and Y Wu; validation and writing—original draft preparation: C Y Xiao, G Y Li; writing review and editing: J G Huang and L Q Si.
Corresponding author
Ethics declarations
Ethics approval
The present investigation was conducted as per the guidelines of the Institutional Animal Ethical Committee of Tongji Medical College. The Institutional Animal Ethical Committee duly approved the experimental protocol.
Consent to publication
All authors have read and agreed to the published version of the manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xiao, C., Li, G., Li, X. et al. A topical thermosensitive hydrogel system with cyclosporine A PEG-PCL micelles alleviates ulcerative colitis induced by TNBS in mice. Drug Deliv. and Transl. Res. 13, 2447–2462 (2023). https://doi.org/10.1007/s13346-023-01317-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-023-01317-8