Abstract
Context
Evidence-based research on psycho-oncology in last three decades lays emphasis upon the critical role of psychological services for better illness adjustment, improved quality of life, reduced distress and cognitive problems among the rapidly increasing pediatric cancer population.
Justification
This review aims to summarize the evidence-based psychological interventions in childhood cancer over the two decades and addresses the wide gap that existed between intervention studies worldwide and India, thus highlighting the need for research and appropriate services.
Evidence acquisition
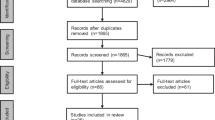
We searched electronic databases such as MedLine, PubMed, PsycINFO, and Google Scholar. Key search terms were pediatric cancer, psycho-oncology, children with cancer + psychological intervention, or multimodal treatment, psychotherapy, cognitive training, behavioral, social skills+ feasibility study, pilot, randomized controlled trial, case study, systematic reviews.
Results
28 full papers published between 1996 to 2016, including survivors and under-treatment children below 18 years, were reviewed. Various types of key interventions were psychosocial, physical, cognitive behavioral, cognitive, music art therapy and play therapy. Generally, intervention settings were either hospital or home, and were designed to promote psychological well-being. Psychological interventions were more in customised formats in these studies. A generic intervention module was not available for replication.
Conclusion
Development of culture-specific generic intervention module and using the same in randomized control studies with larger effect size are needed in India for larger coverage of patients.
Similar content being viewed by others
References
Satyanarayana L, Asthana S, Labani PS. Childhood cancer incidence in India: A review of population-based cancer registries. Indian Pediatr. 2014;51:218–20.
Arora RS, Eden TO, Kapoor G. Epidemiology of childhood cancer in India. Indian J Cancer. 2009;46:264–73.
Mehta M, Abrol BM. Emotional reaction and adjustment problems of patients with laryngeal carcinoma. Indian J Clinical Psychol. 1982;9:107–12.
Patel MJ, Sinha BK, Shah PM, Vankar GK, Parikh BJ. Patterns of psychological disturbance among leukemia patients and their relatives. Indian J Cancer. 1987;24: 264–71.
Satpathy S, Das IB. Psychological correlates in leukemia. Journal of Indian Psychiatric Society-Orissa. 1997;6:5–20.
Li HC, Chung OK, Chiu SY. The impact of cancer on children’s physical, emotional, and psychosocial wellbeing. Cancer Nurs. 2010;33:47–54.
Kazak A. Surviving Cancer Competently Intervention Program–Newly Diagnosed (SCCIP–ND) treatment manual. J Pediatr Psychol (JPP), 1998–2002. Editor’s vale dictum. J Pediatr Psychol. 2002;27:653–63.
Varni JW, Katz ER, Colegrove R Jr, Dolgin M. The impact of social skills training on the adjustment of children with newly diagnosed cancer. J Pediatr Psychol. 1993;18:751–67.
Kazak AE, Penati B, Boyer BA, Himelstein B, Brophy P, Waibel MK, et al. A psychological and pharmacological intervention protocol for procedural distress in pediatric leukemia. J Pediatr Psychol. 1996;21:615–31.
Die-Trill M, Bromberg J, Lavally B, Portales LA, Sanfeliz A, Patenaude AF. Development of social skills in boys with brain tumors. J Psychosoc Oncol. 1996;14:23–41.
Barrera M. Brief Clinical Report: Procedural pain and anxiety management with mother and sibling as cotherapists. J Pediatric Psychology. 2000; 25:117–21.
Favara-Scacco C, Smirne G, Schilirò G, Di Cataldo A. Art therapy as support for children with leukemia during painful procedures. Med Pediatr Oncol. 2001;36:474–80.
Barakat LP, Hetzke JD, Foley B, Carey ME, Gyato K, Phillips PC. Evaluation of a social-skills training group intervention with children treated for brain tumors: A pilot study. J Pediatr Psychol. 2003;28:299–307.
Kazak AE, Simms S, Alderfer MA, Rourke MT, Crump T, McClure K, et al. Feasibility and preliminary outcomes from a pilot study of a brief psychological intervention for families of children newly diagnosed with cancer. J Pediatric Psychol. 2005a;30:644–55.
Hinds PS, Hockenberry M, Rai SN, Zhang L, Razzouk BI, Cremer L, et al. Clinical field testing of an enhancedactivity intervention in hospitalized children with cancer. J Pain Symptom Management. 2007;33:686–97.
Butler WR, Copeland DR, Fairclough DL, Mulhern RK, Katz ER, Kazak AE, et al. A multicenter, randomized clinical trial of a cognitive remediation program for childhood survivors of a pediatric malignancy. J Consult Clin Psychol. 2008;76:367–78.
Barrera M, Schulte F. A group social skills intervention program for survivors of childhood brain tumors. J Pediatric Psychol. 2009;34:1108–18.
Thygeson MV, Hooke MC, Clapsaddle J, Robbins A, Moquist K. Peaceful Play Yoga: Serenity and balance for children with cancer and their parents. J Pediatric Oncolology Nursing. 2010; 27:276–84.
Speyer E, Herbinet A, Vuillemin A, Briançon S, Chastagner P. Effect of adapted physical activity (apa) sessions in the hospital on health-related quality of life for children with cancer: A cross-over randomized trial. Pediatr Blood Cancer. 2010;55:1160–66.
Braam KI, Dijk EM, Veening MA, Bierings MB, Merks JHM, Grootenhuis MA, et al. Design of the Quality of Life in Motion (QLIM) study: A randomized controlled trial to evaluate the effectiveness and cost-effectiveness of a combined physical exercise and psychosocial training program to improve physical fitness in children with cancer. BMC Cancer. 2010;10:624.
O’Callaghan C, Baron A, Barry P, Dun B. Music’s relevance for pediatric cancer patients: a constructivist and mosaic research approach. Support Care Cancer. 2011;19:779–88.
Yeh CH, Man Wai JP, Lin US, Chiang YC. A pilot study to examine the feasibility and effects of a home-based aerobic program on reducing fatigue in children with acute lymphoblastic leukemia. Cancer Nurs. 2011;34:3–12.
Gohar SF, Comito M, Price J, Marchese V. Feasibility and parent satisfaction of a physical therapy intervention program for children with acute lymphoblastic leukemia in the first 6 months of medical treatment. Pediatr Blood Cancer. 2011;56:799–804.
Hardy KK, Willard VW, Bonner MJ. Computerized cognitive training in survivors of childhood cancer: a pilot study. J Pediatr Oncol Nurs. 2011;28:27–33.
Moore IM, Hockenberry MJ, Anhalt C, McCarthy K, Krull KR. Mathematics intervention for prevention of neurocognitive deficits in childhood leukemia. Pediatr Blood Cancer. 2012;59:278–84.
Shockey DP, Menzies V, Glick DF, Taylor AG, Boitnott A, Rovnyak V. Preprocedural distress in children with cancer: an intervention using biofeedback and relaxation. J Pediatr Oncol Nurs. 2013;30:129–38.
Chari U, Hirisave U, Appaji L. Exploring play therapy in pediatric oncology: a preliminary endeavour. Indian J Pediatr. 2013;80:303–8.
Malboeuf-Hurtubise C, Achille M, Sultan S, Vadnais M. Mindfulness-based intervention for teenagers with cancer: study protocol for a randomized controlled trial. Trials. 2013;14:135–43.
Hardy KK, Willard VW, Allen TM, Bonnar MJ. Working memory training in survivors of pediatric cancer: a randomized pilot study. Psycho-oncology. 2013;22:1856–65.
Huang JS, Dillon L, Terrones L, Schubert L, Roberts W, Finklestein J, et al. Fit 4 Life: A weight loss intervention for children who have survived childhood leukemia. Pediatr Blood Cancer. 2014;61:894–900.
Nekah SMA, Kamali F, Jansouz F. The effects of structured cognitive-behavioural group play therapy on anxiety and depression in children with cancer: A pilot study. J Evid Based Care. 2015;5:39–50.
Van Dijk-Lokkart EM, Braam KI, Kaspers GJ, Van Dulmen-den BE, Takken T, Grootenhuis MA, et al. Applicability and evaluation of a psychosocial intervention program for childhood cancer patients. Support Care Cancer. 2015;23:2327.
Polat S, Gürol A, Celebioglu A, Yildirim ZK. The effect of therapeutic music on anxiety in children with acute lymphoblastic leukaemia. Indian J Traditional Knowledge. 2015;14:42–6.
Vallet C, André N, Gentet JC, Verschuur A, Michel G, Sotteau F, et al. Pilot evaluation of physical and psychological effects of a physical trek programme including a dog sledding expedition in children and teenagers with cancer. Ecancer. 2015; 9:558.
Akard TF, Mary S, Dietrich D, Friedman L, Pamela SH, Barbara G, et al. Digital Storytelling: An Innovative Legacy-Making Intervention for Children with Cancer. Pediatr Blood Cancer. 2015;62:658–65.
The National Comprehensive Cancer Network USA, Annual Report. 2013. Available from: http://www.nccn.org/about/annual_report/index.html#20. Accessed August 23, 2017.
Erickson SJ, Steiner H. Trauma and personality correlates in long term pediatric cancer survivors. Child Psychiatry Hum Dev. 2001;31:195–213.
Kazak AE, Prusak A, McSherry M, Simms S, Beele D, Rourke M, et al. The psychosocial assessment tool (PAT): Pilot data on a brief screening instrument for identifying high-risk families in pediatric oncology. Fam Syst Health. 2001;19:303–17.
Kazak AE, Alderfer M, Rourke MT, Simms S, Streisand R, Grossman JR. Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. J Pediatr Psychol. 2004;29:211–9.
Meeske KA, Patel SK, Palmer SN, Nelson MB, Parow AM. Factors associated with health-related quality of life in pediatric cancer survivors. Pediatr Blood Cancer. 2007;49:298–305.
Meeske K, Stuber ML. PTSD, Quality of Life and Psychological outcome in young adult survivors of pediatric cancer. Oncol Nurs Forum. 2001;28:481–9.
Kazak AE, Boeving CA, Alderfer MA, Hwang WT, Reilly A. Posttraumatic stress symptoms during treatment in parents of children with cancer. J Clin Oncol. 2005;23:7405–10.
Aung LL, Saw SM, Chan MY, Khaing T, Quah T, Verkooijen HM. The hidden impact of childhood cancer on the family: A multi-institutional study from Singapore. Ann Acad Med Singapore. 2012;41:170–5.
Jantien Vrijmoet-Wiersma CM, Jeanine MM, van Klink, Annemarie MK, Hendrik MK, Lynne MB, et al. Assessment of parental psychological stress in pediatric cancer: A review. J Pediatr Psychol. 2008;33:694–706.
Butler RW, Mulhern RN. Neurocognitive interventions for children and adolescents surviving cancer. J Pediatr Psychology. 2005;30:65–78.
Nathan PC1, Patel SK, Dilley K, Goldsby R, Harvey J, Jacobsen C, et al. Children’s oncology group long-term follow-up guidelines task force on neurocognitive/behavioral complications after childhood cancer. guidelines for identification of, advocacy for, and intervention in neurocognitive problems in survivors of childhood cancer: a report from the Children’s Oncology Group. Arch Pediatr Adolesc Med. 2007;161:798–806.
Janzen LA, Spiegler BJ. Neurodevelopmental sequel of pediatric acute lymphoblastic leukemia and its treatment. Des Dis Rev Res Rev. 2008;14:185–95.
Nazemi KJ, Butler RW. Neuropsychological rehabilitation for survivors of childhood and adolescent brain tumors: a view of the past and a vision for a promising future. J Pediatr Rehabil Med. 2011;4:37–46.
Sansom-Daly UM, Wakefield CE, Bryant RA, Butow P, Sawyer S, Patterson P, et al. Online group-based cognitivebehavioural therapy for adolescents and young adults after cancer treatment: A multicenter randomised controlled trial of Recapture Life-AYA. BMC Cancer. 2012;12:339–51.
Kazak AE, Rourke MT, Alderfer MA, Pai ALH, Reilly AF, Meadows AT. Evidence-based assessment, intervention and psychosocial care in pediatric oncology: a blueprint for comprehensive services across treatment. J Pediatr Psychol. 2007;32:1099–110.
Marsac ML, Hildenbrand AK, Clawson K, Jackson L, Kohser K, Barakat L. Acceptability and feasibility of family use of The Cellie Cancer Coping Kit. Support Care Cancer. 2012;012:1475.
Hildenbrand AK, Alderfer MA, Deatrick JA, Marsac ML. A mixed methods assessment of coping with pediatric cancer. J Psychosoc Oncol. 2014;32:37–58.
Pai K, Mehrotra S, Vidyasagar MS. Conducting brief group interventions for hospitalized cancer patients in India: An examination of short term psychological outcome of a controlled trial. J Pers Soc Psychol. 2005;21:1–7.
Kahalley LS, Wilson SJ, Tyc VL, Conklin HM, Hudson MM, Shengjie Wu, et al. Are the Psychological Needs of adolescent survivors of pediatric cancer adequately identified and treated? Psycho-oncology. 2013; 22:447–58.
Srivastava V, Ansari MA, Kumar A, Shah AG, Meena RK, Sevach P, et al. Study of anxiety and depression among breast cancer patients from North India. J Clin Psychiatry. 2016;2:1–7.
Singh RPB, Singh H, Singh CJ, Kaur KT. Screening of psychological distress in cancer patients during chemotherapy: A cross-sectional study. Indian J Palliative Care. 2015;21:305–10.
Pandey M, Sarita GP, Devi N, Thomas BC, Hussain BM, Krishnan R. Distress, anxiety, and depression in cancer patients undergoing chemotherapy. World J Surg Oncol. 2006;26:4–68.
Pandey M, Devi N, Thomas BC, Kumar SV, Krishnan R, Ramdas K. Distress overlaps with anxiety and depression in patients with head and neck cancer. Psychooncology. 2007;16:582–6.
Batra P, Kumar B, Gomber S, Bhatia MS. Assessment of quality of life during treatment of pediatric oncology patients. Indian J Public Health. 2014;58:168–73.
Rajajee S, Ezhilarasi S, Indumathi D. Psychosocial problems in families of children with cancer. Indian J Pediatr. 2007;74:837–9.
Abraham A, Appaji L. Cognitive assessment of children with acute lymphoblastic leukemia: Preliminary findings. Indian J Med Paediatr Oncol. 2009;30:14–9.
Seth T. Communication to pediatric cancer patients and their families: A cultural perspective. Indian J Palliat Care. 2010;16:26–9.
Patil AB, Tole AP, Advani SH. Occupational therapy intervention program for a better quality of life for acute lymphoblastic leukemia survivors. Indian J Occupational Therapy. 2003;35:13–4.
Helgeson VS. Recent advances in psychosocial oncology. J Consult Clin Psychol. 2005;73:268–71.
Kohlsdorf M, Costa ALJ. Psychosocial impact of pediatric cancer on parents-A literature review. Paideia. 2012;22:119–29.
Cernvall M. Symptoms of posttraumatic stress in parents of children on cancer treatment. factor structure, experiential avoidance, and internet-based guided self-help. Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1051. 65 pp. 2014; Uppsala: Acta Universitatis Upsaliensis.
Haegen VM, Stress LO. Psychosocial mediators, and cognitive mediators in parents of child cancer patients and cancer survivors: Attention and working memory pathway perspectives. J Psychosoc Oncol. 2015;33:504–50.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Satapathy, S., Kaushal, T., Bakhshi, S. et al. Non-pharmacological Interventions for Pediatric Cancer Patients: A Comparative Review and Emerging Needs in India. Indian Pediatr 55, 225–232 (2018). https://doi.org/10.1007/s13312-018-1323-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13312-018-1323-3