Abstract
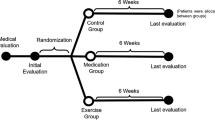
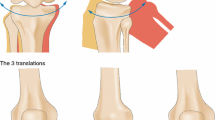
The Infrapatellar Fat Pad (IFP) lies between patella, femur, meniscus and tibia and properly fills the space between these structures. This fatty structure facilitates distribution of synovial fluid and may act to absorb impulsive actions generated through the joint. In case of Osteoarthritis (OA), IFP is found to be affected by inflammation, hypertrophy and fibrosis. The aim of the present study is to analyze the correlation between microscopic characteristics and mechanical properties of the IFP in healthy and OA conditions. The microscopic anatomy of the IFP was analyzed through histological methods, whose results showed that the IFP affected by OA maintains similar lobules configuration but thicker interlobular septa. Geometrical data together with the morphological analysis of lobules and septa represented the basic data to provide numerical micro-models of the IFP. Numerical analyses were developed to evaluate the mechanical behavior considering the characteristic loading conditions as compressive, torsion and shear actions. The results were applied to identify the parameters of a homogenized hyperelastic constitutive formulation that interprets the IFP mechanics. The constitutive formulation was implemented within a finite element model of the knee, which was applied to evaluate the overall mechanical functionality of the knee structures. The results pointed out the actual mechanical relevance of IFP and the loss of proper stress–strain behavior of the OA IFP under mechanical loads.









Similar content being viewed by others
References
Hoffa A (1904) The influence of the adipose tissue with regard to the pathology of the knee joint. J Am Med Assoc 43:795–796
Platzer W (1999) Atlas van de anatomie, 7th edn. Intro, Baarn
Clements KM, Ball AD, Jones HB, Brickmann S, Read SJ, Murray F (2009) Cellular and histopathological changes in the infrapatellar fat pad in the monoiodoacetate model of osteoarthritis pain. Osteoarthr Cartil 17:805–812
Clockaerts S, Bastiaansen-Jenniskens YM, Runhaar J, Van Osch GJVM, Van Offel J:F, Verhaar JAN, De Clerck LS, Somville J (2010) The infrapatellar fat pad should be considered as an active osteoarthritic joint tissue: a narrative review. Osteoarthr Cartil 18:876–882
Ioan-Facsinay A, Kloppenburg M (2013) An emerging player in knee osteoarthritis: the infrapatellar fat pad. Arthritis Res Ther 15(6):225
Goldring MB, Goldring SR (2007) Osteoarthritis. J Cell Physiol 213:626–634
Macchi V, Porzionato A, Sarasin G, Petrelli L, Guidolin D, Rossato M, Fontanella CG, Natali A, De Caro R (2016) The infrapatellar adipose body: an histotopographic study. Cell Tissue Organs 201:220–231
Gurumurthy B, Bierdeman P, Janorkar AV (2017) Spheroid model for osteogenic evaluation of human adipose derived stem cells. J Biomed Mat Res A 105(4):1230–1236
Favero M, El Hadi H, Belluzzi E, Granzotto M, Porzionato A, Sarasin G, Iacobellis C, Cigolotti A, Fontanella CG, Natali AN, Ramonda R, Ruggieri P, De Caro R, Rossato M, Macchi V (2017) Infrapatellar fat pad features in osteoarthritis: a histopathological and molecular study. Rheumatology 56(10):1784–1793
Fontanella CG, Nalesso F, Carniel EL, Natali AN (2016) Biomechanical behavior of plantar fat pad in healthy and degenerative foot conditions. Med Biol Eng Comput 54:653–661
Fontanella CG, Carniel EL, Frigo A, Macchi V, Porzionato A, Sarasin G, Rossato M, De Caro R, Natali AN (2017) Investigation of biomechanical response of Hoffa’s fat pad and comparative characterization. J Mech Beh Biomed Mater 67:1–9
Natali AN, Fontanella CG, Carniel EL (2012) A numerical model for investigating the mechanics of calcaneal fat pad region. J Mech Behav Biomed 5:216–223
Wang Y-N, Lee K, Ledoux WR (2011) Histomorphological evaluation of diabetic and non-diabetic plantar soft tissue. Foot Ankle Int 32(8):802–810
De Caro R, Macchi V, Porzionato A (2009) Promotion of body donation and use of cadavers in anatomical education at the University of Padova. Anat Sci Educ 2:91–92
Porzionato A, Macchi V, Stecco C, Mazzi A, Rambaldo A, Sarasin G, Parenti A, Scipioni A, De Caro R (2012) Quality management of body donation program at the University of Padova. Anat Sci Educ 5:264–272
Dobrin PB (1996) Effect of histologic preparation on the cross-sectional area of arterial rings. J Surg Res 61:413–415
Comley K, Fleck NA (2010) A micromechanical model for the Young’s modulus of adipose tissue. Int J Solids Struct 47:2982–2990
Miller Young JE, Duncan NA, Baroud G (2002) Material properties of the human calcaneal fat pad in compression: experiment and theory. J Biomech 35:1523–1531
Sommer G, Eder M, Kovacs L, Pathak H, Bonitz L, Mueller C, Regitnig P, Holzapfel GA (2013) Multiaxial mechanical properties and constitutive modeling of human adipose tissue: a basis for preoperative simulations in plastic and reconstructive surgery. Acta Biomater 9:9036–9048
Comley K, Fleck NA (2012) The compressive response of porcine adipose tissue from low to high strain rate. Int J Impact Eng 46:1–10
Geerlings M, Peters GWM, Ackermans PAJ, Oomens CWJ, Baaijens FPT (2008) Linear viscoelastic response of adipose tissue. Biorheology 45(6):677–688
Funk JR, Hall GW, Crandall JR, Pilkey WD (2000) Linear and quasi-linear visco-elastic characterization of ankle ligament. J Biomed Eng 122:15–22
Liao H, Zakhaleva J, Chen W (2009) Cells and tissue interactions with glycated collagen and their relevance to delayed diabetic wound healing. Biomaterials 30:1689–1696
Stevenson K, Schweitzer M, Hamarneh G (2006) Multi-Angle deformation analysis if Hoffa’s fat pad. Proc. of SPIE 6143:614329
Pai S, Ledoux WR (2012) The shear mechanical properties of diabetic and non-diabetic plantar soft tissue. J Biomech 45(2):364–370
Fontanella CG, Carniel EL, Forestiero A, Natali AN (2014) Investigation of the mechanical behaviour of the foot skin. Skin Res Technol 20(4):445–452
Dam EB, Folkesson J, Pettersen MD, Christiansen C (2007) Automatic morphometric cartilage quantification in the medial tibial plateau from MRI for osteoarthritis grading. Osteoarthr Cartil 15:808–818
Hunter DJ, Buck R, Vignon E, Eckstein F, Brand K, Mazzuca AS, Wyman BT, Otterness I, Hellio MP, Le Graverand MPH (2009) Relation of regional articular cartilage morphometry and meniscal position by MRI to joint space width in knee radiographs. Osteoarthr Cartil 17:1170–1176
Galbusera F, Freutel M, DUrselen L, D’aiuto M, Croce D, Villa T, Sansone V, Innocenti B (2014) Material models and properties in the finite ligament analysis of knee ligaments: a literature review. Front Bioeng Biotechnol 2:54
Natali AN, Carniel EL, Pavan PG (2010) Modelling of mandibole bone properties in the numerical analysis of oral implant biomechanics. Comput Methods Biomech Biomed Eng 100(2):158–165
Forestiero A, Carniel EL, Natali AN (2014) Biomechanical behaviour of ankle ligaments: constitutive formulation and numerical modelling. Comput Methods Biomech Biomed Eng 14(4):395–404
Fontanella CG, Forestiero A, Carniel EL, Natali AN (2013) Analysis of heel pad tissues mechanics at the heel strike in bare and shod conditions. Med Eng Phys 35:441–447
Jacobson JA, Lenchik L, Ruhoy MK, Schweitzer ME, Resnick D (1997) MR Imaging of the infrapatellar fat pad of Hoffa. Radiographics 17:675–691
Moverley R, Williams D, Bardakos N, Field R (2014) Removal of the infrapatella fat pad during total knee arthroplasty: does it affect patient outcomes? Int Orthop 38:2483–2487
Pinsornsak P, Naratrikun K, Chumchuen S (2014) The effect of infrapatellar fat pad excision on complications after minimally invasive TKA: a randomized controlled trial. Clin Orthop Relat Res 472:695–701
Ye C, Zhang W, Wu W, Xu M, Nonso NS, He R (2016) Influence of the infrapatellar fat pad resection during total knee arthroplasty: a systematic review and meta-analysis. PLoS ONE 11(10):e0163515
Fung YC (2013) Biomechanics: mechanical properties of living tissues. Springer, New York
Beidokhti HN, Janssen D, Khoshgoftar M, Sprenders A, Perdahcioglu ES, Van den Boogaard T, Verdonschot N (2016) A comparison between dynamic implicit and explicit finite element simulations of the native knee joint. Med Eng Phys 38:1123–1130
Kiapour A, Kiapour AM, Kaul V, Quatman CE, Wordeman SC, Hewett TE, Demetropoulos CK, Goel VK (2014) Finite element model of the knee for investigation of injury mechanisms: development and validation. J Biomech Eng 136:011002
Acknowledgements
The authors are grateful to Dr. Gloria Sarasin for her skillful technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Fontanella, C.G., Macchi, V., Carniel, E.L. et al. Biomechanical behavior of Hoffa’s fat pad in healthy and osteoarthritic conditions: histological and mechanical investigations. Australas Phys Eng Sci Med 41, 657–667 (2018). https://doi.org/10.1007/s13246-018-0661-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-018-0661-8