Abstract
Objectives
Despite extensive research aimed at clarifying (failing) pelvic organ support, the complete aetiology of pelvic organ prolapse (POP) is still not fully understood. During vaginal delivery, the pelvic floor can be irreversibly traumatised, resulting in pubovisceral muscle avulsions. The aetiology of these avulsions is discussed in this pictorial overview. Normal female pelvic floor anatomy is described and variations are exemplified using magnetic resonance (MR) images. The clinical relevance of detecting pubovisceral muscle avulsions is specified.
Methods
T2-weighted MR imaging has multiplanar capabilities with high diagnostic accuracy allowing for detailed visualisation of the pelvic floor. Together with the use of a three-dimensional (3D) post-processing program, the presence and severity of pubovisceral muscle avulsions can be quantified.
Results
Pelvic floor MR imaging is a non-invasive method that enables adequate identification of pubovisceral muscle avulsions which are known risk factors for the development of POP. They can be scored with good to excellent inter- and intra-observer reliability.
Conclusions
Radiologists and urogynaecology subspecialists should be familiar with MR imaging findings of pubovisceral muscle avulsions as this birth-related trauma is observed in over 36 % of vaginally parous women.
Teaching Points
• Pelvic organ prolapse (POP) is a growing problem for both patients and for our healthcare system
• Pubovisceral muscle avulsions are known risk factors for pelvic organ prolapse (POP)
• T2-weighted MR imaging visualises pubovisceral muscle avulsions adequately
• Pubovisceral muscle avulsions are scored with good to excellent inter- and intra-observer reliability
Similar content being viewed by others
Introduction
The opening within the bony pelvis comprises the biggest potential hiatus within the human body. It is closed off by the pelvic floor which acts as a supportive layer to all pelvic and abdominal organs. The pelvic floor must maintain urinary and faecal continence, but also permit urination and defecation. Furthermore, in women, intercourse and vaginal birth should be possible. It is understandable that with these contradicting properties the pelvic floor is prone to failure, which could ultimately lead to symptoms of pelvic floor dysfunction [1].
Pelvic organ prolapse (POP), urinary incontinence (UI) and faecal incontinence (FI) are the most common of all disorders assembled under the term “pelvic floor dysfunction”. Up to 20 % of the female population will have symptoms of POP and/or UI severe enough to require surgery [2]. Another one out of six women will undergo additional surgery because of postoperative POP recurrence [3, 4]. Even though a vast amount of research has increased our knowledge on pelvic floor dysfunction since the first documentation in the Kahun Gynaecological Papyrus (ca. 1800 B.C. [fragments of the Kahun Papyri were discovered by Flinders Petri in 1889 and are kept at the University College London]), the complete disease mechanism of POP is still not fully understood: women with several risk factors may have normal pelvic organ support, whereas others develop POP even though they exhibit none of the known contributors.
Pelvic organ prolapse has both non-obstetric and obstetric causes. The former group includes conditions suggestive of weak connective tissue and a family history of POP (congenital factors), but also advancing age, heavy lifting and chronically increased intra-abdominal pressure [5, 6]. Furthermore, smoking, being from middle-European descent and a higher body mass index are reported contributors [5, 7, 8]. But of all these factors, none has as big a negative impact on pelvic organ support as vaginal delivery. Women who have given birth vaginally are 4–11 times more likely to develop POP [9].
But how do these risk factors influence pelvic organ support? What alters in the pelvic floor that leads to a lacking supportive function? And how can we visualise these alterations? One explanation lies in the damage to the pubovisceral component of the levator ani muscle. Avulsions are (partial) detachments of the pubovisceral muscle from their insertion on the pubis. Pubovisceral muscle avulsions can occur during vaginal delivery and are readily visualised using magnetic resonance (MR) imaging [10].
In this pictorial overview, we describe how the presence and severity of pubovisceral muscle avulsions can be interpreted on pelvic floor MR imaging. Both normal female pelvic floor anatomy and pubovisceral muscle avulsions are visualised. Furthermore, clinical implications are discussed.
Normal female pelvic floor anatomy
The pelvic floor includes all structures that support the pelvic and abdominal organs: the pelvic bones, connective tissue and the pelvic floor muscles, i.e. the levator ani and (ischio-)coccygeal muscles. All muscles are connected to the bony pelvis and overly the obturator internus muscles bilaterally (Fig. 1). The levator ani is a striated muscle that is in a constant state of contraction. It provides upward support by automatically adjusting its activity to variations in abdominal pressure and body position. The pelvic and abdominal organs are hereby prevented from herniating outside the body. The levator ani is one of the most complex muscle groups in the human body and as a result also one of the most poorly understood. It comprises several muscle parts that are often difficult to discern and which have, over the years, been given several names, making understanding even more difficult. The levator ani is composed of the iliococcygeal muscles laterally and the pubococcygeal muscles medially (Fig. 2). The most medial parts of the pubococcygeal muscles are attached to the inside of the pubis. From the site of insertion, they course around the anal canal intertwining with the muscle fibres of the external anal muscle. The resulting V-shaped muscle has been named the pubovisceral or puborectal muscle interchangeably and has the function to pull the anorectal junction ventrally and cranially. It surrounds the levator hiatus through which the urethra, vagina and anal canal pass. In nulliparous women, the levator hiatus has a mean area of 11 cm2 at rest and 14 cm2 on maximal Valsalva [11]. Reportedly, women with (symptoms of) POP have a larger hiatus than those with normal pelvic organ support. The hiatus is also larger in women with postoperative POP recurrence [11, 12].
Schematic representation of the pelvic floor (coronal plane). The obturator internus muscles are bilaterally connected to the bony pelvis. The levator ani muscle is funnel-shaped and can be found between the obturator internus muscles and the vagina. C cervix, V vagina, LAM levator ani muscle, OIM obturator internus muscle, DTPM deep transverse perineal muscle
Cranial view of the female pelvic floor, consisting of the levator ani muscle and the (ischio-) coccygeal muscles (axial plane). The right side of the patient illustrates a more cranial level. The most medial part of the pubococcygeal muscle is formed by the pubovisceral muscle, which surrounds the levator hiatus through which the urethra, vagina, and anal canal pass. PB pubic bone, PVM pubovisceral part of levator ani muscle, PCM pubococcygeal muscle, ICM iliococcygeal muscle, OIM obturator internus muscles, (I)CM (ischio-)coccygeal muscle, PM piriformis muscle
Failing pelvic organ support
To understand the complex entity of pelvic organ support, Professor Peggy Norton (Salt Lake City, UT, USA) introduced the “boat in dry dock” concept (Fig. 3), in which the boat represents the pelvic and abdominal organs. The organs are supported by water (portraying the levator ani) and stabilised by cables, i.e. the pelvic ligaments. When water is drained from the dry dock (laxity of levator ani muscle), the entire weight of the boat is put on the cables (ligaments), hereby exerting immense forces. In the female body, if the levator ani is injured, the pelvic ligaments can restrain the accompanying forces for a period of time. However, adequate pelvic organ support is eventually lost, resulting in POP.
Schematic representation of how pelvic organ prolapse is a multi-factorial problem. The water represents the support of the pelvic floor to the pelvic and abdominal organs (the boat). When the pelvic floor is traumatised, i.e. the water is drained from the dry dock, all weight is put on the pelvic ligaments (the cables stabilising the boat). The pelvic ligaments can restrain the accompanying forces, but when the intra-abdominal pressure increases (black arrows), the cables at some point will be significantly damaged, resulting in pelvic organ prolapse
The term POP is commonly used to describe any degree of downward pelvic movement of a vaginal compartment with the pelvic organs protruding into the vagina or even past the introitus. With anterior compartment prolapse, the bladder and/or urethra are involved, whereas in POP of the central compartment, the vaginal vault with the uterus or cuff scar (in case of prior hysterectomy) descents. The latter may contain the small intestine, bladder or sigmoid. In case of posterior compartment prolapse, the rectum, with or without the small intestine, descents into the vagina. Multiple vaginal compartments are often affected [13].
Previously, when a woman suffered from symptoms of pelvic floor dysfunction, imaging techniques such as cystourethrography and defecography were used in case physical examination was non-conclusive. However, pelvic floor MR imaging provides an overview of the entire pelvic floor, which is especially useful when patients have symptoms that indicate the involvement of multiple vaginal compartments. Julia Fielding explained when to use MR imaging and how to interpret these images in case of signs and symptoms of pelvic floor dysfunction [14]. Nowadays, diffusions tensor MR imaging even allows three-dimensional (3D) visualisation and quantification of the female pelvic floor [15]. The current article is an addition to the paper of Fielding and is aimed at the interpretation of pubovisceral muscle avulsions on T2-weighted pelvic floor MR imaging.
Pathogenesis and clinical implications of pubovisceral muscle avulsions
During vaginal delivery or even during an attempt at such, the levator hiatus of the labouring woman is stretched to enable the fetus to pass. The area of the average fetal head measures 70–100 cm2 [16], which is several times larger than the original area of the levator hiatus [11]. Using an MR imaging-based computer model, Lien et al. [17] found that the pubovisceral muscle has to stretch up to 3.3 times its initial length during crowning of the fetal head. It is understandable that the pubovisceral muscle may hereby be damaged. The prevalence of levator ani muscle injury is reported to be up to 36 % in vaginally parous women and presents as a detachment, i.e. avulsion, of the pubovisceral component of the levator ani muscle [18, 19]. These pubovisceral muscle avulsions can be observed as a complete loss of connection to the pubis or as a partial detachment with apparent loss of muscle bulk, either unilaterally or bilaterally. Besides this direct type of injury, in which the pubovisceral muscle is torn off from its insertion on the pubis, the muscle can be indirectly injured due to denervation resulting in atrophy, or by ischaemia with reperfusion damage. The indirect types of injury are, however, not subject of this paper.
Several intrapartum factors have been found to be associated with pubovisceral muscle avulsions: the use of forceps, increased maternal age at first delivery and prolonged second stage of labour (dilation phase). Vacuum delivery, epidural analgesia or oxytocin administration did not increase the odds for pubovisceral muscle avulsions. In a recent study, we found that episiotomy, prior anterior vaginal wall reconstructive surgery, presence of POP symptoms and increasing POP of the central vaginal compartment on physical examination were correlated with more severe pubovisceral muscle avulsions. In case of symptoms of obstructive defecation, it was more likely that there was no defect of the levator ani muscle on pelvic floor MR imaging [20]. The study was performed among a group of patients who had either recurrent POP or a discrepancy between clinical signs and symptoms of POP.
Pubovisceral muscle avulsions are more often observed in women with POP. DeLancey et al. [10] found an adjusted odds ratio of 7.3 for major pubovisceral muscle avulsions in women with POP compared with a matched control group. Furthermore, women with pubovisceral muscle avulsions were reportedly more susceptible to postoperative POP recurrence of the anterior vaginal compartment, as they were more often submitted to pelvic floor reconstructive surgery [21, 22].
Diagnostic methods for evaluating pubovisceral muscle avulsions
Pubovisceral muscle avulsions were first described in the 1940s by Gainey [23], but have only recently found their way into our textbooks [24]. Thus, so far there is little awareness for the daily occurrence of this birth related injury. Fortunately, research has been growing steadily, hereby increasing our knowledge. Avulsions can be diagnosed by both palpation and imaging techniques.
Palpation is performed by placing the distal phalynx of the index finger in the lower one-third of the vagina, as this is the site where the insertion of the pubovisceral muscle to the pubis is expected (Fig. 4) [25]. Even though palpation can be easily implemented in routine physical examination, the value of this method as opposed to imaging appears limited due to its considerable learning curve and only moderate agreement between different observers, even after substantial training [25, 26]. The latter might be explained by the fact that palpation of a defect supposedly relies on the comparison with an intact contra lateral side. Dietz et al. [27] did, however, recently suggest to use palpation as a screening method in case surgical intervention for POP is considered. They proposed that in case of one finger space or more between the urethra and the pubovisceral muscle, some form of muscle detachment is probable. However, van Delft et al. [28] found that up to 20 % of nulliparous women would hereby be classified as having some form of pubovisceral muscle avulsion. To us, this is indicative of a natural variation of muscle insertion. Imaging should thus be used to prevent false-positive findings.
Demonstration of how to palpate pubovisceral muscle avulsions. a The model gives a representation of an intact pubovisceral muscle (PVM) on the left side, while the right side shows a pubovisceral muscle avulsion. The pubovisceral muscle can be palpated by placing the index finger in the lower one-third of the vagina immediately lateral to the urethra (U), while pressing against the pubic bone (PB) (b). In case of a pubovisceral muscle avulsion, the index finger will meet no resistance and slide laterally along the pubic ramus (c). LH levator hiatus. Model supplied by courtesy of Professor Hans Peter Dietz, Sydney
MR imaging was the first imaging technique used to detect pubovisceral muscle avulsions. Significant advantages of MR imaging include its native multiplanar capabilities and superior soft-tissue differentiation, whereas considerable costs and limited availability during routine clinical care are cons. These disadvantages can be overcome by 3D perineal ultrasonography (US). Due to technical improvements, 3D US now enables us to visualise the pelvic floor in the axial plane as well [29]. It is therefore more and more used in the research setting. Its capability to distinguish between different tissues remains inferior to MR imaging, but the clinical relevance of this might be limited. The Translabial 3D-Ultrasonography for Diagnosing Levator Defects (TRUDIL) study is currently being performed to estimate the diagnostic accuracy of 3D US compared with MR imaging [30]. Specific MR imaging techniques can be used to evaluate pubovisceral muscle avulsions, such as endoanal MR imaging [31]. In this paper, however, images obtained with T2-weighted MR imaging using an external surface coil were used.
Pelvic floor MR imaging protocol
There is no international standardised pelvic floor MR imaging protocol that can be used for women with symptoms and/or signs of pelvic floor dysfunction. The following represents the protocol of the Radboud University Medical Centre, Nijmegen, The Netherlands.
MR imaging is performed after voiding with the patient in the supine position. No oral or intravenous contrast agents are administered. For bowel preparation, 10 mg bisacodyl is taken the day before imaging and 1 ml scopolaminebutyl is injected intramuscularly directly prior to imaging to reduce intestinal movement. Patients are asked to retain from ingesting fluids and eating solid food up to 1 and 4 h before the examination, respectively. Image quality is hereby enhanced. As the entire protocol also includes a dynamic phase, the anal canal is opacified with 120 ml ultrasound gel. The dynamic images are used to identify a possible enterocele and/or rectal intussusception. Only the static images are used for the grading of pubovisceral muscle avulsions. In our experience, the presence of ultrasound gel never interfered with the grading of pubovisceral muscle avulsions.
Static images of the pelvic floor are acquired in the axial plane using T2-weighted turbo spin-echo (TSE) sequences on a 3-T (TRIO; Siemens Medical Solutions, Erlangen, Germany) MR imaging unit (repetition time [ms]/echo time [ms] (TR/TE), 2,000/90; field of view (FOV), 200 × 200 mm; slice thickness 3 mm, no image spacing; 320 × 320 matrix; flip angle 150°). A 3D SPACE sequence is acquired of the entire pelvis with 1 mm isotropic voxels. Section orientation is parallel and perpendicular to the plane of the anal canal. A phased-array surface coil for signal reception is centred low on the pelvis. The entire MR examination time is approximately 25 min.
Images were imported and analysed in a 3D imaging post-processing program (TeraRecon, San Mateo, CA, USA). Hereby, the observers were able to reconstruct the 3D datasets to acquire images in the plane of minimal hiatal dimensions. This plane is defined as the angled axial plane with anteriorly the inferior aspect of the pubis and posteriorly the inner aspect of the pubovisceral muscle at the anorectal angle (Fig. 5) [32]. This plane is thought to represent the true levator hiatus [11, 29].
Plane of minimal hiatal dimensions (sagittal plane). Pubovisceral muscle avulsions are scored in the axial plane at the level of minimal hiatal dimensions (white line). This plane shows the inferior aspect of the pubis anteriorly and the inner aspect of the pubovisceral muscle at the anorectal angle posteriorly and can be best observed in the sagittal plane
Pubovisceral muscle avulsions can be scored with adequate inter-observer reliability among women with either POP or urinary incontinence, and healthy controls [33]. We recently extended the use of the levator defect scoring system to a group of women with recurrent POP or with a discrepancy between clinical signs and symptoms of POP. One of the observers in our study was a novice examiner who had no radiology experience, but who did participate in a case-based course. This was followed by the jointly scoring of 15 MR datasets with the second observer, an experienced abdominal radiologist. Again, good to excellent inter-observer reliability was obtained [34].
Scoring pubovisceral muscle avulsions
To illustrate normal anatomy of the pubovisceral muscle, the following T2-weighted MR images are from a 34-year-old woman with normal pelvic organ support. The pubovisceral muscle can be observed between the vagina and the obturator internus muscles as shown in Fig. 6. In the following paragraphs, we will clarify how the presence and severity of pubovisceral muscle avulsions can be evaluated on pelvic floor MR imaging.
Axial T2-weighted MR images with schematic representations of the pelvic floor of a 34-year-old woman (axial and coronal planes). The pubovisceral muscle (PVM) inserts on the pubic bone (PB) and courses behind the anal canal (AC) (a, b). The V-shaped pubovisceral muscle encloses the urethra (U) anteriorly, the vagina (V) and the anal canal posteriorly. The obturator internus muscles (OIM) are well defined and can be used for orientation. They overlie the obturator foramen on the inner surface of the pelvic bones. The pubovisceral muscle courses around the anal canal and shows overall normal muscle bulk. In the coronal plane, the pubovisceral muscle is again observed medially from the obturator internus muscle (c, d). GM gluteus maximus muscle
The research group of Professor John DeLancey (Ann Arbor, MI, USA) developed the levator defect scoring system to assess pubovisceral muscle avulsions. This scoring system does not just observe the amount of muscle present, as this is known to vary among nulliparous women and most likely to vary even more among vaginally parous women [35]. Instead, it focuses on the type of injury seen after vaginal delivery and uses a scoring system that estimates what percentage of the expected muscle bulk is missing. Both the axial and coronal planes are used for scoring. The sagittal plane was not found to be useful for avulsion assessment.
The arcuate pubic ligament is used as a reference point, as this can be precisely localised in every patient. This structure is a thickened continuation of the periosteum and connects the caudal parts of the two pubic bones. When moving from caudal to cranial in the axial plane, the arcuate pubic ligament can be found at the level where a connection between the pubic bones is first observed (Fig. 7). The insertion of the pubovisceral muscle may be identified 10–25 mm cranial to this plane [36].
As the scoring system relies on the estimation of the percentage of muscle missing, normal pubovisceral muscle bulk is ascertained for each woman individually. This can be best observed in the axial plane at the level where the pubovisceral muscle courses behind the anal canal. Examples of normal muscle bulk are shown in Fig. 8a and b. In Fig. 8b, it is clearly illustrated why we should not use standardised values. This would have led to the classification of some degree of pubovisceral muscle avulsion even though this woman was nulliparous and had thus never sustained injury to the pelvic floor.
a T2-weighted axial MR image of a 65-year-old woman who has overall significant muscle bulk of the pubovisceral muscle (axial plane). There is bilateral connection of the muscle to the pubis with normal muscle bulk. b Image of a 59-year-old woman who also had bilateral attachment of the pubovisceral muscle to the pubis and preservation of normal muscle bulk. The normal amount of muscle bulk in this woman is, however, almost 50 % less than that of the woman in a. Both images are in the plane of minimal hiatal dimensions
After assessing normal muscle bulk, the connection of both pubovisceral muscle parts to the pubis is explored. In case of a complete detachment from the insertion on the pubis, the maximum score is appointed, i.e. a unilateral score of 3 (Table 1). Considerable loss of muscle bulk due to atrophy of the muscle is often observed in these cases. This is however not obligatory for the maximum score. In case of some degree of connection of the pubovisceral muscle to the pubis, the amount of muscle bulk missing is quantified (Table 1). Figure 9a–d show a schematic representation of the unilateral scores 0–3. In all figures, there is an intact pubovisceral muscle on the right side while the left muscle side is affected in varying degrees.
Schematic representations of varying degrees of pubovisceral muscle avulsions. In each figure, the right muscle part has full attachment to the pubis and normal muscle bulk (unilateral avulsion severity score of 0). a A bilateral intact pubovisceral muscle; b–d the left pubovisceral muscle parts are affected to varying degrees. This birth-related trauma can result in the loss of <50 % (b) or ≥50 % (c) of the muscle bulk (unilateral avulsion severity score of 1 and 2, respectively). Note that there is still a visible connection between the muscle and the pubis. The left pubovisceral muscle part in d is detached from the pubis, therefore having a unilateral avulsion severity score of 3. Usually, when the pubovisceral muscle is completely detached from the pubis, the remaining muscle part has lost a significant amount of its original muscle bulk, but this is not obligatory
A final score is obtained by adding up the unilateral scores (total score: range 0–6). An ordinal classification system as shown in Table 2 was created by DeLancey et al. [37] to categorise the abnormalities. A total score of 0 indicates normal bilateral pubovisceral muscles (no defect) (Fig. 10a), whereas a total score of 1, 2, or 3 is categorised as a minor avulsion (Fig. 10b). Exception to the rule is a unilateral score of 3 with an intact muscle on the other side (Fig. 10c). This score is regarded as a major pubovisceral muscle avulsion as it clinically behaved similar to major avulsions when looking at risk factors for injury and occurrence of POP [37]. Total scores of 4–6 are also considered major avulsions (Fig. 10d).
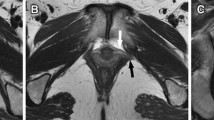
T2-weighted MR images of the different types of pubovisceral muscle avulsions (axial plane). No defect of the pubovisceral muscle (a) and minor (b) and major (c, d) pubovisceral avulsions. The score of each side is depicted in each image separately and the white arrows point to (the remnants of) the pubovisceral muscle. In a both muscle parts have a full connection to the pubic bone and there is normal muscle bulk. The right pubovisceral muscle in b has a normal connection and normal muscle bulk and was therefore scored a 0, whereas the right muscle shows ≥50 % loss of muscle bulk. There is, however, still attachment of the muscle to the pubic bone. The situation in b was classified as a minor pubovisceral avulsion (total score of 2). c A normal muscle on the left side, whereas the right muscle side is completely detached from its insertion on the pubis and has also lost significant amount of muscle bulk (major avulsion). In d, the pubovisceral muscle is equally damaged on both sides with only minimal connection of both muscle parts to the pubic bone and significant loss of muscle bulk bilaterally. This is a good example of a major pubovisceral avulsion. Notice that the size of the levator hiatus has increased compared with the one of the woman in a
In case a defect is suspected in the axial plane, the presence and severity of muscle damage have to be confirmed based on the coronal images [37]. Identifying asymmetric muscle appearance due to asymmetric placement of the patient in the scanner and not to muscle loss are hereby avoided. The arcuate pubic ligament is again used as reference. Ideally, the pubovisceral muscle appears as an eyebrow-shaped structure with its lateral brim pointing upwards (Fig. 11). The scoring system requires multiple images to assign a score. This also applies to the coronal plane.
Pubovisceral avulsions that are suspected in the axial plane have to be confirmed using the coronal images. In this plane, the inferior connection between the two pubic bones is again used as a reference. When moving from anterior to posterior, the pubovisceral muscle appears as an eyebrow-shaped structure with its lateral brim pointing upwards
Challenges in scoring pubovisceral muscle avulsions
To avoid false-positive scorings due to asymmetric muscle appearance for other reasons than avulsion, we used a 3D imaging post-processing program. This allowed us to reconstruct the MR images and to perform volumetric analyses. Any pelvic rotation was corrected for by joining corresponding bony landmarks in different directions, e.g. the femoral heads. Hereafter, the plane of minimal hiatal dimensions was determined in the sagittal plane (Fig. 5). Figure 12a and b give an axial overview of the pelvis before and after 3D modelling. In Fig. 12a, the pubovisceral muscle is not visible entirely. Normal muscle bulk behind the anal canal cannot be determined in this plane, but an attachment of both muscle sides to the pubis is observed. Obviously, the patient’s placement in the MR scanner was asymmetrical relative to the plane in which the entire pubovisceral muscle can be observed. After 3D modelling, with just one look, it became clear that there was no actual damage to the pubovisceral muscle on the left side, but that the right pubovisceral muscle side had sustained minor trauma. Three-dimensional modelling is also of added value in case of significant POP, especially posterior vaginal compartment prolapse, because the anorectal junction descents. Without 3D modelling, we would often not be able to observe the entire pubovisceral muscle in one plane. Figure 13 shows the downward descent of the plane of minimal hiatal dimensions (white line) in a woman with stage III POP of both the anterior and posterior vaginal compartment. This plane is several degrees angled downwards compared with the plane of minimal hiatal dimensions demonstrated in Fig. 5. Confirmation using the coronal plane might become redundant when using 3D modelling. However, we did use both planes to assign a score.
Pubovisceral muscle in the axial plane before and after 3D modelling. Essential for scoring presence and severity of pubovisceral muscle avulsions is the connection of the muscle to the inner surface of the pubis. Furthermore, normal muscle bulk should be determined using the muscle at the level where it courses behind the anal canal. In a An image is shown that was obtained using the regular protocol and was selected as the correct image to assess insertion of the muscle on the pubis. The entire pubovisceral muscle is not depicted. b An image of the same patient after 3D modelling with the orientation parallel to the direction of the plane of minimal hiatal dimensions. Connection of both muscle sides can be observed, as well as the normal muscle bulk of the pubovisceral muscle
MR images of a 63-year old woman who was diagnosed with POP of both the anterior and posterior vaginal compartment. The sagittal plane shows a downward descent of the pelvic floor and thus the plane of minimal hiatal dimensions. Three-dimensional modelling was essential to adequately score pubovisceral muscle avulsions
Besides causing pubovisceral muscle avulsions, vaginal delivery often causes hiatal ballooning [12]. Hiatal ballooning is an independent risk factor for POP and it further complicates the assessment of pubovisceral muscle avulsions [38]. Figure 14 shows the pelvic floor in the axial plane of a woman with significant hiatal ballooning. The area of the levator hiatus was 47.4 cm2. Even though at first glance there appears to be significant bilateral damage, after 3D modelling, we found that this woman had a thin pubovisceral muscle behind the anal canal at the level of the anorectal junction. Together with the presence of an attachment to the pubis bilaterally, this was appointed a score of 1 on both sides, resulting in a classification as a minor pubovisceral avulsion (total score of 2) instead of a major avulsion.
Axial MR image of the pelvic floor of a 57-year old parous woman. Three-dimensional modelling was used to obtain the plane of minimal hiatal dimensions. The levator hiatus is encircled in white and has a 47,4 cm2 area. The patient has an overall thin pubovisceral muscle and only minor loss of muscle bulk on both sides. She was diagnosed with stage III POP of the posterior vaginal compartment
Conclusions
We have provided a structured overview on the anatomy, pathogenesis and diagnosis of pubovisceral muscle avulsions with a special emphasis on MR imaging. Assessing presence and severity of pubovisceral muscle avulsions can be easily learned when the provided scoring system is used. Good to excellent inter- and intra-observer reliability can hereby be obtained. Women with major pubovisceral muscle avulsions are more likely to develop POP and have previously undergone pelvic floor reconstructive surgery more often than those without levator trauma. The clinical implications of being diagnosed with a pubovisceral muscle avulsion remains topic of future research.
References
Patel DA, Xu X, Thomason AD, Ransom SB, Ivy JS, DeLancey JO (2006) Childbirth and pelvic floor dysfunction: an epidemiologic approach to the assessment of prevention opportunities at delivery. Am J Obstet Gynecol 195(1):23–28
de Boer TA, Slieker-Ten Hove MC, Burger CW, Kluivers KB, Vierhout ME (2011) The prevalence and factors associated with previous surgery for pelvic organ prolapse and/or urinary incontinence in a cross-sectional study in The Netherlands. Eur J Obstet Gynecol Reprod Biol 158(2):343–349
Clark AL, Gregory T, Smith VJ, Edwards R (2003) Epidemiologic evaluation of reoperation for surgically treated pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol 189(5):1261–1267
Denman MA, Gregory WT, Boyles SH, Smith V, Edwards SR, Clark AL (2008) Reoperation 10 years after surgically managed pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol 198(5):555 e551–e555
Miedel A, Tegerstedt G, Maehle-Schmidt M, Nyren O, Hammarstrom M (2009) Nonobstetric risk factors for symptomatic pelvic organ prolapse. Obstet Gynecol 113(5):1089–1097
Lince SL, van Kempen LC, Vierhout ME, Kluivers KB (2012) A systematic review of clinical studies on hereditary factors in pelvic organ prolapse. Int Urogynecol J 23(10):1327–1336
Bump RC (1993) Racial comparisons and contrasts in urinary incontinence and pelvic organ prolapse. Obstet Gynecol 81(3):421–425
Jelovsek JE, Maher C, Barber MD (2007) Pelvic organ prolapse. Lancet 369(9566):1027–1038
Mant J, Painter R, Vessey M (1997) Epidemiology of genital prolapse: observations from the Oxford Family Planning Association Study. Br J Obstet Gynaecol 104(5):579–585
DeLancey JO, Morgan DM, Fenner DE, Kearney R, Guire K, Miller JM et al (2007) Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol 109(2 Pt 1):295–302
Dietz HP, Shek C, Clarke B (2005) Biometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasound. Ultrasound Obstet Gynecol 25(6):580–585
Delancey JO, Hurd WW (1998) Size of the urogenital hiatus in the levator ani muscles in normal women and women with pelvic organ prolapse. Obstet Gynecol 91(3):364–368
Maglinte DD, Kelvin FM, Fitzgerald K, Hale DS, Benson JT (1999) Association of compartment defects in pelvic floor dysfunction. AJR Am J Roentgenol 172(2):439–444
Fielding JR (2002) Practical MR imaging of female pelvic floor weakness. Radiographics 22(2):295–304
Zijta FM, Lakeman MM, Froeling M, van der Paardt MP, Borstlap CS, Bipat S et al (2012) Evaluation of the female pelvic floor in pelvic organ prolapse using 3.0-Tesla diffusion tensor imaging and fibre tractography. Eur Radiol 22(12):2806-2813
Chitty LS, Altman DG, Henderson A, Campbell S (1994) Charts of fetal size: 2. Head measurements. Br J Obstet Gynaecol 101(1):35–43
Lien KC, Mooney B, DeLancey JO, Ashton-Miller JA (2004) Levator ani muscle stretch induced by simulated vaginal birth. Obstet Gynecol 103(1):31–40
DeLancey JO, Kearney R, Chou Q, Speights S, Binno S (2003) The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol 101(1):46–53
Dietz HP, Lanzarone V (2005) Levator trauma after vaginal delivery. Obstet Gynecol 106(4):707–712
Lammers K, Futterer JJ, Inthout J, Prokop M, Vierhout ME, Kluivers KB (2013) Correlating signs and symptoms with pubovisceral muscle avulsions on magnetic resonance imaging. Am J Obstet Gynecol 208(2):148.e1-e7
Weemhoff M, Vergeldt TF, Notten K, Serroyen J, Kampschoer PH, Roumen FJ (2012) Avulsion of puborectalis muscle and other risk factors for cystocele recurrence: a 2-year follow-up study. Int Urogynecol J 23(1):65–71
Dietz HP, Chantarasorn V, Shek KL (2010) Levator avulsion is a risk factor for cystocele recurrence. Ultrasound Obstet Gynecol 36(1):76–80
Gainey HL (1943) Post-partum observation of pelvic tissue damage. Am J Obstet Gynecol 46:457–466
Dietz HP, Hoyte LPJ, Steensma AB (2008) Atlas of pelvic floor ultrasound. Springer, London
Kearney R, Miller JM, DeLancey JO (2006) Interrater reliability and physical examination of the pubovisceral portion of the levator ani muscle, validity comparisons using MR imaging. Neurourol Urodyn 25(1):50–54
Dietz HP, Shek C (2008) Validity and reproducibility of the digital detection of levator trauma. Int Urogynecol J Pelvic Floor Dysfunct 19(8):1097–1101
Dietz HP, Moegni F, Shek KL (2012) Diagnosis of levator avulsion injury: a comparison of three methods. Ultrasound Obstet Gynecol 40(6):693–698
van Delft K, Schwertner-Tiepelmann N, Thakar R, Sultan AH (2013) Inter-rater reliability of assessment of levator ani muscle strength and attachement to the pubic bone in nulliparous women. Ultrasound Obstet Gynecol. doi: 10.1002/uog.12426
Dietz HP (2004) Ultrasound imaging of the pelvic floor. Part II: three-dimensional or volume imaging. Ultrasound Obstet Gynecol 23(6):615–625
Notten KJ, Weemhoff M, Kluivers KB, Schweitzer KJ, Mulder F, Stoker J et al (2011) Protocol for Translabial 3D-Ultrasonography for diagnosing levator defects (TRUDIL): a multicentre cohort study for estimating the diagnostic accuracy of translabial 3D-ultrasonography of the pelvic floor as compared to MR imaging. BMC Womens Health 11:23
Terra MP, Beets-Tan RG, Vervoorn I, Deutekom M, Wasser MN, Witkamp TD et al (2008) Pelvic floor muscle lesions at endoanal MR imaging in female patients with faecal incontinence. Eur Radiol 18(9):1892–1901
Kruger JA, Heap SW, Murphy BA, Dietz HP (2008) Pelvic floor function in nulliparous women using three-dimensional ultrasound and magnetic resonance imaging. Obstet Gynecol 111(3):631–638
Morgan DM, Umek W, Stein T, Hsu Y, Guire K, DeLancey JO (2007) Interrater reliability of assessing levator ani muscle defects with magnetic resonance images. Int Urogynecol J Pelvic Floor Dysfunct 18(7):773–778
Lammers K, Kluivers KB, Vierhout ME, Prokop M, Futterer JJ (2013) Inter- and intraobserver reliability for diagnosing levator ani changes on magnetic resonance imaging. Ultrasound Obstet Gynecol. doi: 10.1002/uog.12462
Tunn R, DeLancey JO, Howard D, Shton-Miller JA, Quint LE (2003) Anatomic variations in the levator ani muscle, endopelvic fascia, and urethra in nulliparas evaluated by magnetic resonance imaging. Am J Obstet Gynecol 188(1):116–121
Chou Q, DeLancey JO (2001) A structured system to evaluate urethral support anatomy in magnetic resonance images. Am J Obstet Gynecol 185(1):44–50
Kearney R, Miller JM, Ashton-Miller JA, DeLancey JO (2006) Obstetric factors associated with levator ani muscle injury after vaginal birth. Obstet Gynecol 107(1):144–149
Dietz HP, Franco AV, Shek KL, Kirby A (2012) Avulsion injury and levator hiatal ballooning: two independent risk factors for prolapse? An observational study. Acta Obstet Gynecol Scand 91(2):211–214
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Lammers, K., Prokop, M., Vierhout, M.E. et al. A pictorial overview of pubovisceral muscle avulsions on pelvic floor magnetic resonance imaging. Insights Imaging 4, 431–441 (2013). https://doi.org/10.1007/s13244-013-0261-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13244-013-0261-9