Abstract
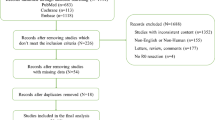
Rectal cancer is a common tumor within a difficult anatomic constraint. Total mesorectal excision with longitudinal and circumferential free margins is considered imperative for good prognosis. In this article, the authors systematically reviewed all published literature with specific Mesh terms until the end of year 2019. Thereafter, retrieved articles were assessed using the Newcastle–Ottawa Scale and meta-analysis was conducted comparing local recurrence among 1-cm, 5-mm, and narrow (< 1-mm)/infiltrated margins. Thirty-nine articles were included in the study. Macroscopic distal margin < 1 cm carried a higher incidence of recurrence for those who did not receive neoadjuvant radiation, without affecting neither estimated overall nor disease-free survival. Less than 5-mm margin after radiation therapy is accepted oncologically. Infiltrated margins and narrow margins (< 1 mm) microscopically are associated with higher incidence of local recurrence and shorter overall and disease-free survival. Surgeons should aim at 1-cm safety margin in radiotherapy-naïve patients and microscopic free margin > 1 mm for those who received neoadjuvant therapy. The cost/benefit of reoperation for patients with infiltrated margins is still inadequately studied.



Similar content being viewed by others
References
Zeng WG et al (2017) A distal resection margin of ≤1 mm and rectal cancer recurrence after sphincter-preserving surgery: the role of a positive distal margin in rectal cancer surgery. Dis Colon Rectum 60(11):1175–1183
Manegold P et al (2019) The minimum distal resection margin in rectal cancer surgery and its impact on local recurrence-a retrospective cohort analysis. Int J Surg 69:77–83
Bhamre R et al (2019) Impact of length of distal margin on outcomes following sphincter preserving surgery for middle and lower third rectal cancers. Indian J Surg Oncol 10(2):335–341
Hojo K (1986) Anastomotic recurrence after sphincter-saving resection for rectal cancer. Dis Colon Rectum 29(1):11–14
Kameda K et al (1990) Proposed distal margin for resection of rectal cancer. Jpn J Cancer Res 81(1):100–104
Bujko K et al (2012) Is the 1-cm rule of distal bowel resection margin in rectal cancer based on clinical evidence? A systematic review. Ann Surg Oncol 19(3):801–808
Kiran RP, Lian L, Lavery IC (2011) Does a subcentimeter distal resection margin adversely influence oncologic outcomes in patients with rectal cancer undergoing restorative proctectomy? Dis Colon Rectum 54(2):157–163
Rutkowski A et al (2008) Distal bowel surgical margin shorter than 1 cm after preoperative radiation for rectal cancer: is it safe? Ann Surg Oncol 15(11):3124–3131
Pricolo VE, Abodeely A, Resnick M (2010) Distal margins in radical resections for rectal cancer after chemoradiation therapy: how short is long enough? Dig Surg 27(3):185–189
Smith F et al (2014) Depth and lateral spread of microscopic residual rectal cancer after neoadjuvant chemoradiation: implications for treatment decisions. Colorectal Dis 16(8):610–615
Liu R et al (2014) Clinicopathological study of safe resectional margin in mid and low rectal cancer after neoadjuvant chemoradiotherapy. Zhonghua wei Chang wai ke za zhi= Chinese Journal of Gastrointestinal Surgery 17(6):561–564
Kim T et al (2014) The adequacy of the distal resection margin after preoperative chemoradiotherapy for rectal cancer. Colorectal Dis 16(8):O257–O263
Moher D et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS med 6(7):e1000097
Pollett WG, Nicholls R (1983) The relationship between the extent of distal clearance and survival and local recurrence rates after curative anterior resection for carcinoma of the rectum. Ann Surg 198(2):159
Williams N, Dixon M, Johnston D (1983) Reappraisal of the 5 centimetre rule of distal excision for carcinoma of the rectum: a study of distal intramural spread and of patients’ survival. Br J Surg 70(3):150–154
McDermott F et al (1985) Local recurrence after potentially curative resection for rectal cancer in a series of 1008 patients. Br J Surg 72(1):34–37
Heimann TH et al (1986) Local recurrence following surgical treatment of rectal cancer. Dis Colon Rectum 29(12):862–864
Secco GB et al (1989) Factors influencing local recurrence after curative surgery for rectal cancer. Oncology 46(1):10–13
Karanjia N et al (1990) ‘Close shave’ in anterior resection. Br J Surg 77(5):510–512
Vemava A et al (1992) A prospective evaluation of distal margins in carcinoma of the rectum. Surg Gynecol Obstet 175(4):333–336
Bozzetti F et al (1997) Impact of distal clearance margin on oncologic outcome after restorative resection of the rectum. Tumori Journal 83(6):907–911
Kuvshinoff B et al (2001) Distal margin requirements after preoperative chemoradiotherapy for distal rectal carcinomas: are≤ 1 cm distal margins sufficient? Ann Surg Oncol 8(2):163–169
Andreola S et al (2001) Adenocarcinoma of the lower third of the rectum surgically treated with a< 10-MM distal clearance: preliminary results in 35 N0 patients. Ann Surg Oncol 8(7):611–615
Stocchi L et al (2001) Impact of surgical and pathologic variables in rectal cancer: a United States community and cooperative group report. J Clin Oncol 19(18):3895–3902
Phang PT et al (2002) Effects of positive resection margin and tumor distance from anus on rectal cancer treatment outcomes. The American journal of surgery 183(5):504–508
Glehen O et al (2003) Long-term results of the Lyons R90–01 randomized trial of preoperative radiotherapy with delayed surgery and its effect on sphincter-saving surgery in rectal cancer. Br J Surg 90(8):996–998
Moore HG et al (2003) Adequacy of 1-cm distal margin after restorative rectal cancer resection with sharp mesorectal excision and preoperative combined-modality therapy. Ann Surg Oncol 10(1):80–85
Chiappa A et al (2005) Results of treatment of distal rectal carcinoma since the introduction of total mesorectal excision: a single unit experience, 1994–2003. Int J Colorectal Dis 20(3):221–230
Huh JW et al (2008) Sphincter-preserving operations following preoperative chemoradiation: an alternative to abdominoperineal resection for lower rectal cancer? World J Surg 32(6):1116–1123
Leo E et al (2009) Distal clearance margin of 1 cm or less: a safe distance in lower rectum cancer surgery. Int J Colorectal Dis 24(3):317
Kim YW et al (2009) Factors associated with anastomotic recurrence after total mesorectal excision in rectal cancer patients. J Surg Oncol 99(1):58–64
Nash GM et al (2010) Close distal margin and rectal cancer recurrence after sphincter-preserving rectal resection. Dis Colon Rectum 53(10):1365–1373
Silberfein EJ et al (2010) Long-term survival and recurrence outcomes following surgery for distal rectal cancer. Ann Surg Oncol 17(11):2863–2869
Tsutsumi S et al (2011) Tumor response and negative distal resection margins of rectal cancer after hyperthermochemoradiation therapy. Anticancer Res 31(11):3963–3967
Bernstein TE et al (2012) What is a safe distal resection margin in rectal cancer patients treated by low anterior resection without preoperative radiotherapy? Colorectal Dis 14(2):e48-55
Rutkowski A et al (2012) Acceptance of a 5-mm distal bowel resection margin for rectal cancer: is it safe? Colorectal Dis 14(1):71–78
Kwak JY et al (2012) Oncologically safe distal resection margins in rectal cancer patients treated with chemoradiotherapy. J Gastrointest Surg 16(10):1947–1954
Lim JW et al (2012) Close distal margins do not increase rectal cancer recurrence after sphincter-saving surgery without neoadjuvant therapy. Int J Colorectal Dis 27(10):1285–1294
Mezhir JJ et al (2012) Whole-mount pathologic analysis of rectal cancer following neoadjuvant therapy: implications of margin status on long-term oncologic outcome. Ann Surg 256(2):274–279
Han JW et al (2013) Association between a close distal resection margin and recurrence after a sphincter-saving resection for t3 mid- or low-rectal cancer without radiotherapy. Ann Coloproctol 29(6):231–237
Debove C et al (2015) What happens after R1 resection in patients undergoing laparoscopic total mesorectal excision for rectal cancer? A study in 333 consecutive patients. Colorectal Dis 17(3):197–204
Hong KS et al (2015) Oncologic outcomes in rectal cancer with close distal resection margins: a retrospective analysis. Ann Surg Treat Res 89(1):23–29
Kang DW et al (2017) Oncologic outcomes in rectal cancer patients with a ≤1-cm distal resection margin. Int J Colorectal Dis 32(3):325–332
Grosek J et al (2017) The influence of the distal resection margin length on local recurrence and long- term survival in patients with rectal cancer after chemoradiotherapy and sphincter- preserving rectal resection. Radiol Oncol 51(2):169–177
Manegold P et al (2019) The minimum distal resection margin in rectal cancer surgery and its impact on local recurrence - a retrospective cohort analysis. Int J Surg 69:77–83
Metwally IH et al (2019) Clinico-epidemiologic criteria and predictors of survival of rectal cancer among Egyptians in Delta region. Journal of Coloproctology 39(4):339–345
Shirouzu K, Isomoto H, Kakegawa T (1995) Distal spread of rectal cancer and optimal distal margin of resection for sphincter-preserving surgery. Cancer 76(3):388–392
Hayden DM et al (2012) Tumor scatter after neoadjuvant therapy for rectal cancer: are we dealing with an invisible margin? Dis Colon Rectum 55(12):1206–1212
Fekete Z et al (2013) What is the significance of a microscopically positive resection margin in the curative-intent treatment of rectal adenocarcinoma? A retrospective study. J buon 18(4):989–995
Fitzgerald TL, Brinkley J, Zervos EE (2011) Pushing the envelope beyond a centimeter in rectal cancer: oncologic implications of close, but negative margins. J Am Coll Surg 213(5):589–595
Tilly C et al (2014) R1 rectal resection: look up and don't look down. Ann Surg 260(5):794–800
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
An abstract of the article has been presented as an E-poster in the European Society of Coloproctology (ESCP) 2021 16th Annual Scientific Conference.
Rights and permissions
About this article
Cite this article
Metwally, I.H., Zuhdy, M., Hamdy, O. et al. The Impact of Narrow and Infiltrated Distal Margin After Proctectomy for Rectal Cancer on Patients’ Outcomes: a Systematic Review and Meta-analysis. Indian J Surg Oncol 13, 750–760 (2022). https://doi.org/10.1007/s13193-022-01565-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-022-01565-z