Abstract
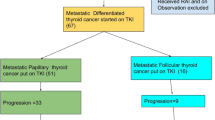
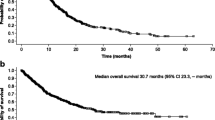
There is a paucity of evidence of the impact of sorafenib on MCT and it is the preferred therapy used in India. We decided to do an audit of all patients of MCT who were referred to us for systemic therapy. The objective of this exercise was to identify the treatment pattern, outcomes, and adverse events with therapy in MCT. Baseline demographics (age, gender, ECOG PS, comorbidities, habits), tumor details (site of metastasis), previous treatment details, clinical features at metastasis (symptomatic or asymptomatic), the pattern of treatment, adverse events (CTCAE version 4.02), date of progression, date of death and status, and follow-up were extracted from the rare tumor database and electronic medical records. Out of 75 patients referred for therapy for MCT, 47 (62.7%) patients were considered for immediate tyrosine kinase inhibitors as they had symptomatic status and 28 (37.3%) patients were kept on observation due to the asymptomatic nature of the disease. Out of the 28 patients, 15 (53.6%, n = 28) patients were subsequently started on TKI while in 13 (46.4%, n = 28) patients observation was continued. In the overall cohort, the median PFS was 18.9 months (95% CI 11.9–29.9) and OS was 26.6 months (95% CI 14.4–39.0). Among variables tested, only female gender had an impact on PFS (hazard ratio = 0.364 95% CI 0.148–0.895; P = 0.028) and the absence of lung metastasis had a positive impact on OS (hazard ratio = 0.443 95% CI 0.207–0.95; P = 0.037). Most commonly used TKI was sorafenib (n = 61) and sunitinib in 1 patient. The most common adverse events with TKI were palmo-plantar dysesthesia (50, 80.6%) and oral mucositis (25, 40.2%). The strategy of treating symptomatic MCT and observing in asymptomatic MCT is associated with reasonable PFS and OS. Sorafenib is the most commonly used TKI in our setup and provides similar outcomes as globally.





Similar content being viewed by others
References
Wells SA Jr, Asa SL, Dralle H et al (2015) Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid 25:567–610
Wells SA Jr, Robinson BG, Gagel RF et al (2012) Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J Clin Oncol 30:134–141
Elisei R, Schlumberger MJ, Müller SP et al (2013) Cabozantinib in progressive medullary thyroid cancer. J Clin Oncol 31:3639–3646
Wirth LJ, Sherman E, Robinson B et al (2020) Efficacy of selpercatinib in RET-altered thyroid cancers. N Engl J Med 383:825–835
Markham A (2020) Pralsetinib: first approval. Drugs 80:1865–1870
Lam ET, Ringel MD, Kloos RT et al (2010) Phase II clinical trial of sorafenib in metastatic medullary thyroid cancer. J Clin Oncol 28:2323–2330
Ahmed M, Barbachano Y, Riddell A et al (2011) Analysis of the efficacy and toxicity of sorafenib in thyroid cancer: a phase II study in a UK based population. Eur J Endocrinol 165:315–322
Ito Y, Onoda N, Ito K-I et al (2017) Sorafenib in Japanese Patients with locally advanced or metastatic medullary thyroid carcinoma and anaplastic thyroid carcinoma. Thyroid 27:1142–1148
Kocsis J, Szekanecz É, Bassam A et al (2019) First line sorafenib treatment for metastatic medullary thyroid cancer: efficacy and safety analysis. Exp Clin Endocrinol Diabetes 127:240–246
Vuong HG, Ho ATN, Tran TTK et al (2019) Efficacy and toxicity of sorafenib in the treatment of advanced medullary thyroid carcinoma: a systematic review and meta-analysis. Head Neck 41:2823–2829
de Castroneves LA, Negrão MV, de Freitas RMC et al (2016) Sorafenib for the treatment of progressive metastatic medullary thyroid cancer: efficacy and safety analysis. Thyroid 26:414–419
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Aditya Pavan Kumar Kanteti and George Abraham are co-first authors.
Rights and permissions
About this article
Cite this article
Kanteti, A.P.K., Abraham, G., Patil, V.M. et al. An Audit of Systemic Therapy in Medullary Carcinoma Thyroid. Indian J Surg Oncol 13, 61–67 (2022). https://doi.org/10.1007/s13193-021-01381-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-021-01381-x