Abstract
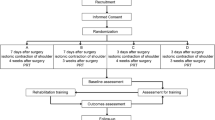
Breast cancer ranks highest in incidence and mortality among females and second among both genders. Lebanon has the second highest rate of breast cancer worldwide for those 35–39 years old and the highest for those 40–49. Mastectomy often results in deceased shoulder and arm mobility and decreased quality of life. The objective of this study was to assess the effect of an educational program of therapeutic exercises on the quality of life and functional ability in women after a mastectomy. Sixty women undergoing a mastectomy were randomly assigned to either an intervention or control group. The intervention group received extensive pre-surgery education as well as training on therapeutic exercises. Follow-up phone calls to the intervention group were made to ensure that the exercises were being done. Both groups were visited at home at two and four weeks to obtain the outcome variables. The Breast Cancer Patient Version was used to assess quality of life, and the “Goniometer” was used to assess the range of motion of the affected shoulder. At two and four weeks after surgery, women in the intervention group had significant improvements in their shoulder range of motion: flexion, extension, and abduction were significantly different between the control and intervention group at p = 0.04–0.00. For quality of life, physical, psychological, psychological, social, and spiritual well-being were significantly higher for the intervention group at both two and four weeks after surgery, p < 0.001. In a middle-income country, one-to-one education provided by a nurse, which included demonstrations, back demonstrations, and weekly phone calls had a positive impact on women’s shoulder range of motion and quality of life. NCT04184102

Similar content being viewed by others
References
Cancer. World Health Organization. [Internet]. Published September 12, 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/cancer. Accessed Apr 2020
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA-Cancer J Clin 68:394–424
Breast cancer statistics. World Cancer Research Fund International. Available from: http://www.wcrf.org/int/cancer-facts-figures/data-specific-cancers/breast-cancer-statistics. Accessed Jan 2020
Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H et al (2013) Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer 49:1374–1403
Salem C, Atallah D, Safi J, Chahine G, Haddad A, El Kassis N et al (2017) Breast density and breast cancer incidence in the Lebanese population: results from a retrospective multicenter study. Biomed Res Int 2017:7594953
Yee J, Davis GM, Hackett D, Beith JM, Wilcken N, Currow D, Emery J, Phillips J, Martin A, Hui R, Harrison M, Segelov E, Kilbreath SL (2019) Physical activity for symptom management in women with metastatic breast cancer: a randomised feasibility trial. J Pain Symptom Manag 58:929–939
Cho O, Yoo Y, Kim N (2006) Efficacy of comprehensive group rehabilitation for women with early breast cancer in South Korea. Nurs Health Sci 8:140–146
National Cancer Institute. Breast cancer prevention (PDQ)-patient version. [Internet]. 2018. Available from https://www.cancer.gov/types/breast/patient/breast-prevention-pdq. Accessed Nov 2018
Montgomery GH, Schnur JB, Erblich J, Diefenbach MA, Bovbjerg DH (2010) Pre surgery: psychological factors predict pain, nausea, and fatigue one week following breast cancer surgery. J Pain Symptom Manag 39(6):1043–1052
Group TW (1998) Development of the World Health Organization WHOQoL-BREF quality of life assessment. Psychol Med 28:551–558
Cheema BS, Gaul CA (2006) Full-body exercise training improves fitness and quality of life in survivors of breast cancer. J Strength Cond Res 20:14
Haddou Rahou B (2016) E, Rhazi K, Ouasmani F, Nejjari C, Bekkali R, Montazeri A, et al. Quality of life in Arab women with breast cancer: a review of the literature. Health Qual Life Outcomes 14:64–64
Leysen L, Lahousse A, Nijs J, Adriaenssens N, Mairesse O, Ivakhnov S et al (2019) Prevalence and risk factors of sleep disturbances in breast cancer survivors: systematic review and meta-analyses. Support Care Cancer 27:4401–4433. https://doi.org/10.1007/s00520-019-04936-5
Lovelace DL, McDaniel LR, Golden D (2019) Long-Term Effects of Breast Cancer Surgery, Treatment, and Survivor Care. J Midwifery Wom Heal 64:713–724
Mishra SI, Scherer RW, Geigle PM, Berlanstein DR, Topaloglu O, Gotay CC et al (2012) Exercise interventions on health-related quality of life for cancer survivors. Cochrane Database Syst Rev 2012(8):CD007566. https://doi.org/10.1002/14651858
Dieli-Conwright CM, Orozco BZ (2015) Exercise after breast cancer treatment: current perspectives. Breast Cancer (Dove Medical Press) 7:353–362
Furmaniak AC, Menig M, Markes MH (2016) Exercise for women receiving adjuvant therapy for breast cancer. Cochrane Database Syst Rev 9:CD005001
Claudio B, Robert M, Brett P, Jordan L, Christina SM, Anthony H (2014) Twenty-five years of research on the effects of exercise training in breast cancer survivors. World J Clin Oncol 5:177–190
Yang A, Sokolof J, Gulati A (2018) The effect of preoperative exercise on upper extremity recovery following breast cancer surgery: a systematic review. Int J Rehabil Res 41:189–196
Badr LK, Bourdeanu L, Alatrash M, Bekarian G (2018) Breast cancer risk factors: a cross-cultural comparison between the West and the East. Asian Pac J Cancer Prev 19:2109–2116
Donnelly TT, Al-Thani ABM, Benjamin K, Al-Khater AH, Fung TS, Ahmedna M et al (2018) Arab female and male perceptions of factors facilitating and inhibiting their physical activity: findings from a qualitative study in the Middle East. PLoS One 13:e0199336
Pace do Amaral MT, Freire de Oliveira MM, Ferreira Nde O, Guimarães RV, Sarian LO, Gurgel MS (2012) Manual therapy associated with upper limb exercises vs. exercises alone for shoulder rehabilitation in postoperative breast cancer. Physiother Theory Pract 28:299–306
Ferrell BR, Dow KH, Grant M. Quality of life instrument - breast cancer patient version [Internet]. Measurement Instrument Database for the Social Science. Available from http://www.midss.org/content/quality-life-instrument-breast-cancer-patient-version-QoL-bc. Accessed Feb 2017
Ferrell BR, Dow KH, Grant M (1996) Measurement of the quality of life in cancer survivors. Qual Life Res 4:523–531
Awad MA, Denic S, El Taji H (2008) Validation of the European organization for research and treatment of cancer quality of life questionnaires for Arabic-speaking populations. Ann N Y Acad Sci 1138:146–154
Haddou Rahou B, El Rhazi K, Ouasmani F, Nejjari C, Bekkali R, Montazeri A et al (2016) Quality of life in Arab women with breast cancer: a review of the literature. Health Qual Life Outcomes 14:64
Shariat A, Tamrin SB, Arumugam M, Danaee M, Ramasamy R (2016) Comparative reliability of different instruments used to measure the severity of musculoskeletal disorders in office workers. Work. 54(3):753–758. https://doi.org/10.3233/WOR-162313
Kizil R, Dilek B, Şahin E, Engin O, Soylu AC, Akalin E, Alper S (2018) Is continuous passive motion effective in patients with lymphedema? A randomized controlled trial. Lymphat Res Biol 16:263–269
Mazor M, Lee JQ, Peled A, Zerzan S, Irwin C, Chesney MA, Serrurier K, Sbitany H, Dhruva A, Sacks D, Smoot B (2018) The effect of yoga on arm volume, strength, and range of motion in women at risk for breast cancer-related lymphedema. J Altern Complement Med 24:154–160
Lee BK, Lee JS, Kim TS (2013) The influence of 4 weeks complex therapeutic exercises on visual analog scale of pain and range of motion for middle-aged women with breast cancer-related lymphedema. J Korean Soc Phys Med 8:153–161
Park JH (2017) The effects of complex exercise on shoulder range of motion and pain for women with breast cancer-related lymphedema: a single-blind, randomized controlled trial. Breast Cancer 24:608–614
Baima J, Reynolds SG, Edmiston K, Larkin A, Ward BM, O’Connor A (2017) Teaching of independent exercises for prehabilitation in breast cancer. J Cancer Educ 32:252–256
Mahdy N, Sattar R (2012) Effect of pre-discharge guidelines on women’s knowledge and self-care practices regarding arm lymphedema prevention post mastectomy. J Am Sci 8:1003–1017
Shamseddine A, Saleh A, Charafeddine M, Seoud M, Mukherji D, Temraz S, Sibai AM (2014) Cancer trends in Lebanon: a review of incidence rates for the period of 2003-2008 and projections until 2018. Popul Health Metrics 12:4
Taha N, Azeaz M, Hassan A, Shaban A (2013) Effect of educational program regarding therapeutic exercises on women’s pain, fatigue and shoulder function undergoing mastectomy. J Am Sci 9:412–425
Abbass Reslan H, Moustafa SM, Saghieh S, Sharara ES, Badr LK (2018) Does intervention improve the outcomes of patients after total knee replacement surgery? Int J Orthop Trauma Nurs 31:26–31
Nemli A, Tekinsoy Kartin P (2019) Effects of exercise training and follow-up calls at home on physical activity and quality of life after a mastectomy. Jpn J Nurs Sci 16:322–328
Dieli-Conwright CM, Courneya KS, Demark-Wahnefried W et al (2018) Aerobic and resistance exercise improves physical fitness, bone health, and quality of life in overweight and obese breast cancer survivors: a randomized controlled trial. Breast Cancer Res 20(1):124 Published 2018 Oct 19
De Groef A, Van Kampen M, Dieltjens E et al (2015) Effectiveness of postoperative physical therapy for upper-limb impairments after breast cancer treatment: a systematic review. Arch Phys Med Rehabil 96(6):1140–1153. https://doi.org/10.1016/j.apmr.2015.01.006
Mullaney MJ, McHugh MP, Johnson CP, Tyler TF (2010) Reliability of shoulder range of motion comparing a goniometer to a digital level. Physiother Theory Pract 26(5):327–333. https://doi.org/10.3109/09593980903094230
Bluethmann SM, Vernon SW, Gabriel KP, Murphy CC, Bartholomew LK (2015) Taking the next step: a systematic review and meta-analysis of physical activity and behavior change interventions in recent post-treatment breast cancer survivors. Breast Cancer Res Treat 149:331–342. https://doi.org/10.1007/s10549-014-3255-5
Sisman H, Sahin B, Duman BB, Tanriverdi G (2012) Nurse-assisted education and exercise decrease the prevalence and morbidity of lymphedema following breast cancer surgery. J Balkan Union Oncol 17:565
Yildiz İ, Varol U, Alacacioglu A (2014) Assessment of the quality of life in Turkish breast cancer patients. J Breast Health 10:216–221. https://doi.org/10.5152/tjbh.2014.2012
Brandstätter M, Kögler M, Baumann U, Fensterer V, Küchenhoff H, Borasio GD, Fegg MJ (2014) Experience of meaning in life in bereaved informal caregivers of palliative care patients. Support Care Cancer 22:1391–1399. https://doi.org/10.1007/s00520-013-2099-6
Eyigor S, Karapolat H, Yesil H, Uslu R, Durmaz B (2010) Effects of Pilate’s exercises on functional capacity, flexibility, fatigue, depression and quality of life in female breast cancer patients: a randomized controlled study. Eur J Phys Rehabil Med 46:481
Garlick M, Wall K, Corwin D, Koopman C (2011) Psycho-spiritual integrative therapy for women with primary breast cancer. J Clin Psychol Med Settings 18:78–90. https://doi.org/10.1007/s10880-011-9224-9
Benton MJ, Schlairet MC, Graham HL (2019) Physical activity-related quality of life in breast cancer survivors compared to healthy women. Eur J Cancer Care e13142. https://doi.org/10.1111/ecc.13142
Breitbart W (2002) Spirituality and meaning in supportive care: spirituality and meaning centered group psychotherapy interventions in advanced cancer. Support Care Cancer 10:272–280
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Quick points
• Nurses can play an important role in teaching women who are undergoing a mastectomy, exercises that may improve their physical and psychological outcomes.
• This study in a middle-income country found that women who underwent a mastectomy and received education, and exercise training had better range of motion in their affected shoulder and better quality of life.
• This randomized control trial study adds to body of evidence regarding the effect of exercise and education on the outcome of women undergoing mastectomies, which has not been conclusively established.
Rights and permissions
About this article
Cite this article
Majed, M., Neimi, C.A., Youssef, S.M. et al. The Impact of Therapeutic Exercises on the Quality of Life and Shoulder Range of Motion in Women After a Mastectomy, an RCT. J Canc Educ 37, 843–851 (2022). https://doi.org/10.1007/s13187-020-01894-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-020-01894-z