Abstract
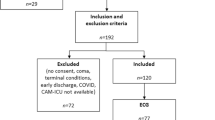
Stroke-induced immunodepression is a major risk factor for severe infectious complications in the immediate post-stroke period. We investigated the predictive value of heart rate variability (HRV) to identify patients at risk of post-stroke infection, systemic inflammatory response syndrome, or severe sepsis during the post-acute interval from days 3 to 5 after stroke onset. A prospective, observational monocentric cohort study was conducted in a university hospital stroke unit of patients with ischemic infarction in the territory of the middle cerebral artery without an ongoing infection at admission. Standard HRV indices were processed from Holter ECG. Recording started within the first day after the onset of stroke. Infection (primary endpoint: pneumonia, urinary tract, unknown localization) was assessed between days 3 and 5. The predictive value of HRV adjusted for clinical data was analyzed by logistic regression models and area under the receiver operating characteristic curve (AUC). From 287 eligible patients, data of 89 patients without event before completion of 24-h Holter ECG were appropriate for prediction of infection (34 events). HRV was significantly associated with incident infection even after adjusting for clinical covariates. Very low frequency (VLF) band power adjusted for both, the National Institutes of Health Stroke Scale (NIHSS) at admission and diabetes predicted infection with AUC = 0.80 (cross-validation AUC = 0.74). A model with clinical data (diabetes, NIHSS at admission, involvement of the insular cortex) performed similarly well (AUC = 0.78, cross-validation AUC = 0.71). Very low frequency HRV, an index of integrative autonomic-humoral control, predicts the development of infectious complications in the immediate post-stroke period. However, the additional predictive value of VLF band power over clinical risk factors such as stroke severity and insular involvement was marginal. The continuous HRV monitoring starting immediately after admission might probably increase the predictive performance of VLF band power. That needs to be clarified in further investigations.


Similar content being viewed by others
References
Harms H, Prass K, Meisel C, Klehmet J, Rogge W, Drenckhahn C, et al. Preventive antibacterial therapy in acute ischemic stroke: a randomized controlled trial. PLoS One. 2008;3:e2158.
Kumar S, Selim MH, Caplan LR. Medical complications after stroke. Lancet Neurol. 2010;9:105–18.
Heikinheimo T, Broman J, Haapaniemi E, Kaste M, Tatlisumak T, Putaala J. Preceding and poststroke infections in young adults with first-ever ischemic stroke: effect on short-term and long-term outcomes. Stroke. 2013;44:3331–7.
Westendorp WF, Nederkoorn PJ, Vermeij JD, Dijkgraaf MG, van de Beek D. Post-stroke infection: a systematic review and meta-analysis. BMC Neurol. 2011;11:110.
Diener HC, Weimar C. Leitlinien für Diagnostik und Therapie in der Neurologie. Thieme; 2012.
Westendorp WF, Vermeij JD, Vermeij F, Den Hertog HM, DWJ D, van de Beek D, et al. Antibiotic therapy for preventing infections in patients with acute stroke. Cochrane Db Syst Rev. 2012;1:CD008530.
Wartenberg KE, Stoll A, Funk A, Meyer A, Schmidt JM, Berrouschot J. Infection after acute ischemic stroke: risk factors, biomarkers, and outcome. Stroke Res Treat. 2011;2011:830614.
Hoffmann S, Malzahn U, Harms H, Koennecke HC, Berger K, Kalic M, et al. Development of a clinical score (A2DS2) to predict pneumonia in acute ischemic stroke. Stroke. 2012;43:2617–23.
Hoffmann S, Harms H, Ulm L, Nabavi DG, Mackert BM, Schmehl I, et al. Stroke-induced immunodepression and dysphagia independently predict stroke-associated pneumonia—the PREDICT study. J Cereb Blood Flow Metab. 2016:271678X16671964.
Harms H, Grittner U, Droge H, Meisel A. Predicting post-stroke pneumonia: the PANTHERIS score. Acta Neurol Scand. 2013;128:178–84.
Meisel C, Schwab JM, Prass K, Meisel A, Dirnagl U. Central nervous system injury-induced immune deficiency syndrome. Nat Rev Neurosci. 2005;6:775–86.
Dirnagl U, Klehmet J, Braun JS, Harms H, Meisel C, Ziemssen T, et al. Stroke-induced immunodepression: experimental evidence and clinical relevance. Stroke. 2007;38:770–3.
Benarroch EE. Autonomic-mediated immunomodulation and potential clinical relevance. Neurology. 2009;73:236–42.
Colivicchi F, Bassi A, Santini M, Caltagirone C. Cardiac autonomic derangement and arrhythmias in right-sided stroke with insular involvement. Stroke. 2004;35:2094–8.
Lanza GA, Cianflone D, Rebuzzi AG, Angeloni G, Sestito A, Ciriello G, et al. Prognostic value of ventricular arrhythmias and heart rate variability in patients with unstable angina. Heart. 2006;92:1055–63.
Stein PK, Barzilay JI, Chaves PH, Mistretta SQ, Domitrovich PP, Gottdiener JS, et al. Novel measures of heart rate variability predict cardiovascular mortality in older adults independent of traditional cardiovascular risk factors: the Cardiovascular Health Study (CHS). J Cardiovasc Electrophysiol. 2008;19:1169–74.
Frasure-Smith N, Lesperance F, Irwin MR, Talajic M, Pollock BG. The relationships among heart rate variability, inflammatory markers and depression in coronary heart disease patients. Brain Behav Immun. 2009;23:1140–7.
Kop WJ, Stein PK, Tracy RP, Barzilay JI, Schulz R, Gottdiener JS. Autonomic nervous system dysfunction and inflammation contribute to the increased cardiovascular mortality risk associated with depression. Psychosom Med. 2010;72:626–35.
von Kanel R, Carney RM, Zhao S, Whooley MA. Heart rate variability and biomarkers of systemic inflammation in patients with stable coronary heart disease: findings from the Heart and Soul Study. Clin Res Cardiol. 2011;100:241–7.
Lieb DC, Parson HK, Mamikunian G, Vinik AI. Cardiac autonomic imbalance in newly diagnosed and established diabetes is associated with markers of adipose tissue inflammation. Exp Diabetes Res. 2012;2012:878760.
Young LC, Roediger MP, Grandits G, Baker J, Somboonwit C, Williams I, et al. Relationship between inflammatory and coagulation biomarkers and cardiac autonomic function in HIV-infected individuals. Biomark Med. 2014;8:1073–83.
Cooper TM, McKinley PS, Seeman TE, Choo TH, Lee S, Sloan RP. Heart rate variability predicts levels of inflammatory markers: evidence for the vagal anti-inflammatory pathway. Brain Behav Immun. 2015;49:94–100.
Saito I, Hitsumoto S, Maruyama K, Eguchi E, Kato T, Okamoto A, et al. Impact of heart rate variability on C-reactive protein concentrations in Japanese adult nonsmokers: the Toon Health Study. Atherosclerosis. 2016;244:79–85.
Griffin MP, O’Shea TM, Bissonette EA, Harrell FE Jr, Lake DE, Moorman JR. Abnormal heart rate characteristics preceding neonatal sepsis and sepsis-like illness. Pediatr Res. 2003;53:920–6.
Schmidt JM, Sow D, Crimmins M, Albers D, Agarwal S, Claassen J, et al. Heart rate variability for preclinical detection of secondary complications after subarachnoid hemorrhage. Neurocrit Care. 2014;20:382–9.
Günther A, Salzmann I, Nowack S, Schwab M, Surber R, Hoyer H, et al. Heart rate variability—a potential early marker of sub-acute post-stroke infections. Acta Neurol Scand. 2012;126:189–96.
Brämer D, Hoyer H, Gunther A, Nowack S, Brunkhorst FM, Witte OW, et al. Study protocol: prediction of stroke associated infections by markers of autonomic control. BMC Neurol. 2014;14:9.
TaskForce. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation. 1996;93:1043–65.
Reinhart K, Brunkhorst FM, Bone HG, Bardutzky J, Dempfle CE, Forst H, et al. Prevention, diagnosis, therapy and follow-up care of sepsis: 1st revision of S-2k guidelines of the German Sepsis Society (Deutsche Sepsis-Gesellschaft e.V. (DSG)) and the German Interdisciplinary Association of Intensive Care and Emergency Medicine (Deutsche Interdisziplinare Vereinigung fur Intensiv- und Notfallmedizin (DIVI)). Ger Med Sci. 2010;8:Doc14.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–9.
Tateishi Y, Oda S, Nakamura M, Watanabe K, Kuwaki T, Moriguchi T, et al. Depressed heart rate variability is associated with high IL-6 blood level and decline in the blood pressure in septic patients. Shock. 2007;28:549–53.
Sloan RP, McCreath H, Tracey KJ, Sidney S, Liu K, Seeman T. RR interval variability is inversely related to inflammatory markers: the CARDIA study. Mol Med. 2007;13:178–84.
Stein PK, Barzilay JI, Chaves PH, Traber J, Domitrovich PP, Heckbert SR, et al. Higher levels of inflammation factors and greater insulin resistance are independently associated with higher heart rate and lower heart rate variability in normoglycemic older individuals: the Cardiovascular Health Study. J Am Geriatr Soc. 2008;56:315–21.
Fairchild KD, Srinivasan V, Moorman JR, Gaykema RP, Goehler LE. Pathogen-induced heart rate changes associated with cholinergic nervous system activation. Am J Phys Regul Integr Comp Phys. 2011;300:R330–R9.
Stein PK, Schmieg RE Jr, El-Fouly A, Domitrovich PP, Buchman TG. Association between heart rate variability recorded on postoperative day 1 and length of stay in abdominal aortic surgery patients. Crit Care Med. 2001;29:1738–43.
Kleiger RE, Stein PK, Bigger JT Jr. Heart rate variability: measurement and clinical utility. Ann Noninvasive Electrocardiol. 2005;10:88–101.
Godin PJ, Buchman TG. Uncoupling of biological oscillators: a complementary hypothesis concerning the pathogenesis of multiple organ dysfunction syndrome. Crit Care Med. 1996;24:1107–16.
Schmidt H, Muller-Werdan U, Hoffmann T, Francis DP, Piepoli MF, Rauchhaus M, et al. Autonomic dysfunction predicts mortality in patients with multiple organ dysfunction syndrome of different age groups. Crit Care Med. 2005;33:1994–2002.
Chamorro A, Amaro S, Vargas M, Obach V, Cervera A, Gomez-Choco M, et al. Catecholamines, infection, and death in acute ischemic stroke. J Neurol Sci. 2007;252:29–35.
Emsley HC, Hopkins SJ. Acute ischaemic stroke and infection: recent and emerging concepts. Lancet Neurol. 2008;7:341–53.
Walter U, Kolbaske S, Patejdl R, Steinhagen V, Abu-Mugheisib M, Grossmann A, et al. Insular stroke is associated with acute sympathetic hyperactivation and immunodepression. Eur J Neurol. 2013;20:153–9.
Harms H, Reimnitz P, Bohner G, Werich T, Klingebiel R, Meisel C, et al. Influence of stroke localization on autonomic activation, immunodepression, and post-stroke infection. Cerebrovasc Dis. 2011;32:552–60.
Werdan K, Schmidt H, Ebelt H, Zorn-Pauly K, Koidl B, Hoke RS, et al. Impaired regulation of cardiac function in sepsis, SIRS, and MODS. Can J Physiol Pharmacol. 2009;87:266–74.
Hoyer D, Frank B, Baranowski R, Zebrowski JJ, Stein PK, Schmidt H. Autonomic information flow rhythms. From heart beat interval to circadian variation. IEEE Eng Med Biol Mag. 2007;26:19–24.
Alamili M, Rosenberg J, Gogenur I. Day-night variation in heart rate variability changes induced by endotoxaemia in healthy volunteers. Acta Anaesthesiol Scand. 2015;59:457–64.
Rahman SA, Castanon-Cervantes O, Scheer FA, Shea SA, Czeisler CA, Davidson AJ, et al. Endogenous circadian regulation of pro-inflammatory cytokines and chemokines in the presence of bacterial lipopolysaccharide in humans. Brain Behav Immun. 2015;47:4–13.
Yaniv Y, Lakatta EG. The end effector of circadian heart rate variation: the sinoatrial node pacemaker cell. BMB Rep. 2015;48:677–84.
Stein PK. Challenges of heart rate variability research in the ICU. Crit Care Med. 2013;41:666–7.
Acknowledgements
We thank Cornelia Eichhorn of the Center for Clinical Studies, Jena University Hospital, for the data management and Nasim Kroegel for carefully editing the manuscript.
Funding
The work was funded by the Federal Ministry of Education and Research (BMBF), Germany (FKZ: 01EO1002).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol was approved by the local ethic committee of the Jena University Hospital and registered at the German Clinical Trial Register DRKS00003392. Each patient gave written informed consent.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The study was registered under the acronym PRED-SEP (German Clinical Trials Register DRKS00003392).
Appendix
Appendix
Two logistic regression models for the prediction of incident infection occurring first within day 3 to day 5 after the onset of stroke
HRV-based model with covariates 1 = diabetes (no = 0, yes = 1) x2 = NIHSS at admission x3 = VLF (daytime)/10 Logistic regression model Logit P (infection from day 3 to 5) = − 0.822 − 1.537 × x1 + 0.165 × x2 − 0.042 × x3 Model performance AUC (95% CI) model = 0.80 (0.70–0.91), AUC cross-validation = 0.74 (0.62–0.86) Hosmer-Lemeshow p = 0.67, R2 (max-rescaled) = 0.35 | |
Clinical data based model with covariates x1 = diabetes (no = 0, yes = 1) x2 = NIHSS at admission x3 = involvement of the insular cortex (no = 0, yes = 1) Logistic regression model Logit P (infection from day 3 to 5) = − 2.466 − 1.096 × x1 + 0.138 × x2 + 1.190 × x3 Model performance AUC (95% CI) model = 0.78 (0.68–0.89), AUC cross-validation = 0.71 (0.59–0.83) Hosmer-Lemeshow p = 0.91, R2 (max-rescaled) = 0.28 |
Rights and permissions
About this article
Cite this article
Brämer, D., Günther, A., Rupprecht, S. et al. Very Low Frequency Heart Rate Variability Predicts the Development of Post-Stroke Infections. Transl. Stroke Res. 10, 607–619 (2019). https://doi.org/10.1007/s12975-018-0684-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-018-0684-1