Abstract
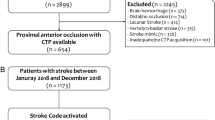
Cerebral reperfusion and arterial recanalization are radiological features of the effectiveness of thrombolysis in acute ischemic stroke (AIS) patients. Here, an investigation of the prognostic role of early recanalization/reperfusion on clinical outcome was performed. In AIS patients (n = 55), baseline computerized tomography (CT) was performed ≤ 8 h from symptom onset, whereas CT determination of reperfusion/recanalization was assessed at 24 h. Multiple linear and logistic regression models were used to correlate reperfusion/recanalization with radiological (i.e., hemorrhagic transformation, ischemic core, and penumbra volumes) and clinical outcomes (assessed as National Institutes of Health Stroke Scale [NIHSS] reduction ≥ 8 points or a NIHSS ≤ 1 at 24 h and as modified Rankin Scale [mRS] < 2 at 90 days). At 24 h, patients achieving radiological reperfusion were n = 24, while the non-reperfused were n = 31. Among non-reperfused, n = 15 patients were recanalized. Radiological reperfusion vs. recanalization was also confirmed by early increased levels of circulating inflammatory biomarkers (i.e., serum osteopontin). In multivariate analysis, ischemic lesion volume reduction was associated with both recanalization (β = 0.265; p = 0.014) and reperfusion (β = 0.461; p < 0.001), but only reperfusion was independently associated with final infarct volume (β = − 0.333; p = 0.007). Only radiological reperfusion at 24 h predicted good clinical response at day 1 (adjusted OR 16.054 [1.423–181.158]; p = 0.025) and 90-day good functional outcome (adjusted OR 25.801 [1.483–448.840]; p = 0.026). At ROC curve analysis the AUC of reperfusion was 0.777 (p < 0.001) for the good clinical response at 24 h and 0.792 (p < 0.001) for 90-day clinical outcome. Twenty-four-hour radiological reperfusion assessed by CT is associated with good clinical response on day 1 and good functional outcome on day 90 in patients with ischemic stroke.




Similar content being viewed by others
References
Bhaskar S, Stanwell P, Cordato D, Attia J, Levi C. Reperfusion therapy in acute ischemic stroke: dawn of a new era? BMC Neurol. 2018;18(1):8.
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early Management of Patients with Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46–e110.
El Amki M, Wegener S. Improving cerebral blood flow after arterial recanalization: a novel therapeutic strategy in stroke. Int J Mol Sci 2017; 18(12).
Horsch AD, Dankbaar JW, Niesten JM, van Seeters T, van der Schaaf I, van der Graaf Y, et al. Predictors of reperfusion in patients with acute ischemic stroke. AJNR Am J Neuroradiol. 2015;36(6):1056–62.
Iglesias-Rey R, Rodriguez-Yanez M, Rodriguez-Castro E, et al. Worse outcome in stroke patients treated with rt-PA without early reperfusion: associated factors. Transl Stroke Res. 2017.
Janjua N, Alkawi A, Suri MF, Qureshi AI. Impact of arterial reocclusion and distal fragmentation during thrombolysis among patients with acute ischemic stroke. AJNR Am J Neuroradiol. 2008;29(2):253–8.
Bouleti C, Mewton N, Germain S. The no-reflow phenomenon: state of the art. Arch Cardiovasc Dis. 2015;108(12):661–74.
Tomsick T. TIMI, TIBI, TICI: I came, I saw, I got confused. AJNR Am J Neuroradiol. 2007;28(2):382–4.
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372(24):2285–95.
Campbell BCV, Donnan GA, Lees KR, Hacke W, Khatri P, Hill MD, et al. Endovascular stent thrombectomy: the new standard of care for large vessel ischaemic stroke. Lancet Neurol. 2015;14(8):846–54.
Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378(1):11–21.
Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378(8):708–18.
Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870–947.
Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46(10):3020–35.
Benson JC, Payabvash S, Mortazavi S, Zhang L, Salazar P, Hoffman B, et al. CT perfusion in acute lacunar stroke: detection capabilities based on infarct location. AJNR Am J Neuroradiol. 2016;37(12):2239–44.
Morelli N, Rota E, Michieletti E, Guidetti D. The “Vexata Quaestio” on lacunar stroke: the role of CT perfusion imaging. AJNR Am J Neuroradiol. 2017;38(2):E11–2.
Cho TH, Nighoghossian N, Mikkelsen IK, Derex L, Hermier M, Pedraza S, Fiehler J, Østergaard L, Berthezène Y, Baron JC: Reperfusion within 6 hours outperforms recanalization in predicting penumbra salvage, lesion growth, final infarct, and clinical outcome Stroke 2015, 46(6):1582–1589.
Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35–41.
Brott T, Adams HP Jr, Olinger CP, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20(7):864–70.
Katzan IL, Lapin B. PROMIS GH (Patient-Reported Outcomes Measurement Information System Global Health) scale in stroke: a validation study. Stroke. 2018;49(1):147–54.
Dargazanli C, Arquizan C, Gory B, Consoli A, Labreuche J, Redjem H, et al. Mechanical thrombectomy for minor and mild stroke patients harboring large vessel occlusion in the anterior circulation: a multicenter cohort study. Stroke. 2017;48(12):3274–81.
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009–18.
Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003;34(8):e109–37.
Wintermark M, Flanders AE, Velthuis B, Meuli R, van Leeuwen M, Goldsher D, et al. Perfusion-CT assessment of infarct core and penumbra: receiver operating characteristic curve analysis in 130 patients suspected of acute hemispheric stroke. Stroke. 2006;37(4):979–85.
Brott T, Marler JR, Olinger CP, Adams HP, Tomsick T, Barsan WG, et al. Measurements of acute cerebral infarction: lesion size by computed tomography. Stroke. 1989;20(7):871–5.
Soares BP, Tong E, Hom J, Cheng SC, Bredno J, Boussel L, et al. Reperfusion is a more accurate predictor of follow-up infarct volume than recanalization: a proof of concept using CT in acute ischemic stroke patients. Stroke. 2010;41(1):e34–40.
Choi JS, Kim HY, Cha JH, Choi JY, Lee MY. Transient microglial and prolonged astroglial upregulation of osteopontin following transient forebrain ischemia in rats. Brain Res. 2007;1151:195–202.
Baliga SS, Merrill GF, Shinohara ML, Denhardt DT. Osteopontin expression during early cerebral ischemia-reperfusion in rats: enhanced expression in the right cortex is suppressed by acetaminophen. PLoS One. 2011;6(1):e14568.
Carbone F, Rigamonti F, Burger F, Roth A, Bertolotto M, Spinella G, et al. Serum levels of osteopontin predict major adverse cardiovascular events in patients with severe carotid artery stenosis. Int J Cardiol. 2018;255:195–9.
Nagar VA, McKinney AM, Karagulle AT, Truwit CL. Reperfusion phenomenon masking acute and subacute infarcts at dynamic perfusion CT: confirmation by fusion of CT and diffusion-weighted MR images. AJR Am J Roentgenol. 2009;193(6):1629–38.
Pan J, Konstas AA, Bateman B, Ortolano GA, Pile-Spellman J. Reperfusion injury following cerebral ischemia: pathophysiology, MR imaging, and potential therapies. Neuroradiology. 2007;49(2):93–102.
Yemisci M, Gursoy-Ozdemir Y, Vural A, Can A, Topalkara K, Dalkara T. Pericyte contraction induced by oxidative-nitrative stress impairs capillary reflow despite successful opening of an occluded cerebral artery. Nat Med. 2009;15(9):1031–7.
Ito U, Hakamata Y, Kawakami E, Oyanagi K. Temporary [corrected] cerebral ischemia results in swollen astrocytic end-feet that compress microvessels and lead to delayed [corrected] focal cortical infarction. J Cereb Blood Flow Metab. 2011;31(1):328–38.
Tachibana M, Ago T, Wakisaka Y, Kuroda J, Shijo M, Yoshikawa Y, et al. Early reperfusion after brain ischemia has beneficial effects beyond rescuing neurons. Stroke. 2017;48(8):2222–30.
Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012;380(9849):1241–9.
Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, Walker GA, et al. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet. 2012;380(9849):1231–40.
Angermaier A, Khaw AV, Kirsch M, Kessler C, Langner S. Influence of recanalization and time of cerebral ischemia on tissue outcome after endovascular stroke treatment on computed tomography perfusion. J Stroke Cerebrovasc Dis. 2015;24(10):2306–12.
Golitz P, Muehlen I, Gerner ST, Knossalla F, Doerfler A. Ultraearly assessed reperfusion status after middle cerebral artery recanalization predicting clinical outcome. Acta Neurol Scand. 2018;137:609–17. https://doi.org/10.1111/ane.12907.
De Silva DA, Fink JN, Christensen S, et al. Assessing reperfusion and recanalization as markers of clinical outcomes after intravenous thrombolysis in the echoplanar imaging thrombolytic evaluation trial (EPITHET). Stroke. 2009;40(8):2872–4.
Eilaghi A, Brooks J, d'Esterre C, et al. Reperfusion is a stronger predictor of good clinical outcome than recanalization in ischemic stroke. Radiology. 2013;269(1):240–8.
An H, Ford AL, Eldeniz C, Chen Y, Vo KD, Zhu H, et al. Reperfusion beyond 6 hours reduces infarct probability in moderately ischemic brain tissue. Stroke. 2016;47(1):99–105.
Dankbaar JW, Horsch AD, van den Hoven AF, Kappelle LJ, van der Schaaf I, van Seeters T, et al. Prediction of clinical outcome after acute ischemic stroke: the value of repeated noncontrast computed tomography, computed tomographic angiography, and computed tomographic perfusion. Stroke. 2017;48(9):2593–6.
Kalogeris T, Baines CP, Krenz M, Korthuis RJ. Ischemia/reperfusion. Compr Physiol. 2016;7(1):113–70.
Carbone F, Vuilleumier N, Burger F, Roversi G, Tamborino C, Casetta I, et al. Serum osteopontin levels are upregulated and predict disability after an ischaemic stroke. Eur J Clin Investig. 2015;45(6):579–86.
Suezawa C, Kusachi S, Murakami T, Toeda K, Hirohata S, Nakamura K, et al. Time-dependent changes in plasma osteopontin levels in patients with anterior-wall acute myocardial infarction after successful reperfusion: correlation with left-ventricular volume and function. J Lab Clin Med. 2005;145(1):33–40.
Mizuma A, Yenari MA. Anti-inflammatory targets for the treatment of reperfusion injury in stroke. Front Neurol. 2017;8:467.
Montecucco F, Liberale L, Bonaventura A, Vecchie A, Dallegri F, Carbone F. The role of inflammation in cardiovascular outcome. Curr Atheroscler Rep. 2017;19(3):11.
Nour M, Scalzo F, Liebeskind DS. Ischemia-reperfusion injury in stroke. Interv Neurol. 2013;1(3–4):185–99.
Marchal G, Young AR, Baron JC. Early postischemic hyperperfusion: pathophysiologic insights from positron emission tomography. J Cereb Blood Flow Metab. 1999;19(5):467–82.
Gaudinski MR, Henning EC, Miracle A, Luby M, Warach S, Latour LL. Establishing final infarct volume: stroke lesion evolution past 30 days is insignificant. Stroke. 2008;39(10):2765–8.
Soares BP, Dankbaar JW, Bredno J, Cheng SC, Bhogal S, Dillon WP, et al. Automated versus manual post-processing of perfusion-CT data in patients with acute cerebral ischemia: influence on interobserver variability. Neuroradiology. 2009;51(7):445–51.
Pezzini A, Busto G, Zedde M, Gamba M, Zini A, Poli L, et al. Vulnerability to infarction during cerebral ischemia in migraine sufferers. Stroke. 2018;49(3):573–8.
Padroni M, Bernardoni A, Tamborino C, Roversi G, Borrelli M, Saletti A, et al. Cerebral blood volume ASPECTS is the best predictor of clinical outcome in acute ischemic stroke: a retrospective, combined semi-quantitative and quantitative assessment. PLoS One. 2016;11(1):e0147910.
Shin YJ, Kim HL, Choi JS, Choi JY, Cha JH, Lee MY. Osteopontin: correlation with phagocytosis by brain macrophages in a rat model of stroke. Glia. 2011;59(3):413–23.
Funding
Analysis and interpretation of data were supported by a grant from the European Commission to Prof F. Mach (FP7-INNOVATION I HEALTH-F2-2013-602114.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Research Involving Human Participants and/or Animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent was obtained from all individual participants included in the study.
This article does not contain any studies with animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Carbone, F., Busto, G., Padroni, M. et al. Radiologic Cerebral Reperfusion at 24 h Predicts Good Clinical Outcome. Transl. Stroke Res. 10, 178–188 (2019). https://doi.org/10.1007/s12975-018-0637-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-018-0637-8