Abstract
Objectives
Research with mindfulness-based programs (MBPs) has found participating in an MBP to predict beneficial outcomes; however, there is currently mixed research regarding the most helpful dose. This review aimed to determine whether different doses related to MBPs significantly predict outcomes.
Methods
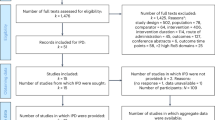
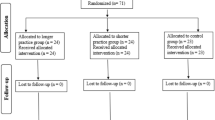
Systematic literature searches of electronic databases and trial registration sites for all randomized controlled trials of MBPs identified 203 studies (N = 15,971). Depression was the primary outcome at post-program and follow-up, with secondary outcomes being mindfulness, anxiety and stress. Doses examined related to session numbers, duration and length, facilitator contact and practice. Dose-response relationships were analyzed using meta-regression in R with separate analyses for inactive and active controls.
Results
Initial meta-analyses found significant between-group differences favoring MBPs for all outcomes. Meta-regression results suggested significant dose-response relationships for the mindfulness outcome for doses relating to face-to-face contact (d = 0.211; C.I.[0.064,0.358]), program intensity (d = 0.895; C.I.[0.315,1.474]) and actual program use (d = 0.013; C.I.[0.001,0.024]). The majority of results for psychological outcomes, including depression, were not significant.
Conclusions
This meta-regression examines dose-response relationships for different types and doses relating to MBPs. Considered together, MBPs appeared helpful compared with controls, supporting previous research. Based on meta-regression results, there was no evidence that larger doses are more helpful than smaller doses for predicting psychological outcomes; a finding consistent with some previous research particularly with non-clinical populations. Additionally, greater contact, intensity and actual use of MBPs predicting increased mindfulness correspond with previous research and theory. Potential limitations and recommendations for future research are explored.















Similar content being viewed by others
References
Abdi, H. (2010). Holm's sequential Bonferroni procedure. In N. Salkind (Ed.), Encyclopedia of research design. Sage.
Banerjee, M., Cavanagh, K., & Strauss, C. (2017). A qualitative study with healthcare staff exploring the facilitators and barriers to engaging in a self-help mindfulness-based intervention. Mindfulness, 8, 1653–1664. https://doi.org/10.1007/s12671-017-0740-z.
Beblo, T., & Schulte, J. (2017). Mindfulness: more practice – better results? Neurology and Rehabilitation, 23(1), 19–26.
Benjamini, Y., & Hochberg, Y. (1995). Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, 57(289), e300. http://www.jstor.org/stable/2346101?origin=JSTOR-pdf.
Berghoff, C. R., Wheeless, L. E., Ritzert, T. R., Wooley, C. M., & Forsyth, J. P. (2017). Mindfulness meditation adherence in a college sample: comparison of a 10-min versus 20-min 2-week daily practice. Mindfulness, 8, 1513–1521. https://doi.org/10.1007/s12671-017-0717-y.
Berlin, J. A., Santanna, J., Schmid, C. H., Szczech, L. A., & Feldman, H. I. (2002). Individual patient- versus group-level data meta-regressions for the investigation of treatment effect modifiers: ecological bias rears its ugly head. Statistics in Medicine, 21(3), 371–387. https://doi.org/10.1002/sim.1023.
Blanck, P., Perleth, S., Heidenreich, T., Kröger, P., Ditzen, B., Bents, H., & Mander, J. (2018). Effects of mindfulness exercises as stand-alone intervention on symptoms of anxiety and depression: systematic review and meta-analysis. Behaviour Research and Therapy, 102, 25–35. https://doi.org/10.1016/j.brat.2017.12.002.
Boggs, J. M., Beck, A., Felder, J. N., Dimidjian, S., Metcalf, C. A., & Segal, Z. V. (2014). Web-based intervention in mindfulness meditation for reducing residual depressive symptoms and relapse prophylaxis: a qualitative study. Journal of Medical Internet Research, 16(3). https://doi.org/10.2196/jmir.3129.
Bondolfi, G., Jermann, F., Van der Linden, M., Gex-Fabry, M., Bizzini, L., Rouget, B. W., Myers-Arrazola, L., Conzalez, C., Segal, Z., Aubrey, J.-M., & Bertschy, G. (2010). Depression relapse prophylaxis with mindfulness-based cognitive therapy: replication and extension in the Swiss health care system. Journal of Affective Disorders, 122, 224–231. https://doi.org/10.1016/j.jad.2009.07.007.
Borenstein, M., Hedges, L. V., Higgins, J. P. T., & Rothstein, H. R. (2009). Introduction to meta-analysis. John Wiley & Sons.
Bruce, N., Shapiro, S. L., Constantino, M. J., & Manber, R. (2010). Psychotherapy mindfulness and the psychotherapy process. Psychotherapy: Theory, Research, Practice, Training, 47(1), 83–97. https://doi.org/10.1037/a0018842.
Carmody, J., & Baer, R. A. (2008). Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine, 31, 23–33. https://doi.org/10.1007/s10865-007-9130-7.
Carmody, J., & Baer, R. A. (2009). How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. Journal of Clinical Psychology, 65(6), 627–638. https://doi.org/10.1002/jclp.20555.
Chang, V. Y., Palesh, O., Caldwell, R., Glasgow, N., Abramson, M., Luskin, F., Gill, M., Burke, A., & Koopman, C. (2004). The effects of a mindfulness-based stress reduction program on stress, mindfulness self-efficacy, and positive states of mind. Stress and Health: Journal of the International Society for the Investigation of Stress, 20, 141–147. https://doi.org/10.1002/smi.1011.
Christley, R. M. (2010). Power and error: increased risk of false positive results in underpowered studies. The Open Epidemiology Journal, 3, 16–19. https://doi.org/10.2174/1874297101003010016.
Clark-Carter, D. (1997). Doing quantitative psychological research: from design to report. Taylor & Francis.
Costa, A., & Barnhofer, T. (2016). Turning towards or turning away: a comparison of mindfulness meditation and guided imagery relaxation in patients with acute depression. Behavioural and Cognitive Psychotherapy, 44(4), 410–419. https://doi.org/10.1017/S1352465815000387.
Crane, C., & Williams, J. M. C. (2010). Factors associated with attrition from mindfulness-based cognitive therapy in patients with a history of suicidal depression. Mindfulness, 1, 1–10. https://doi.org/10.1007/s12671-010-0003-8.
Crane, C., Crane, R. S., Eames, C., Fennell, M. J. V., Silverton, S., Williams, J. M. C., & Barnhofer, T. (2014). The effects of amount of home meditation practice in mindfulness-based cognitive therapy on hazard of relapse to depression in the staying well after depression trial. Behaviour Research and Therapy, 63, 17–24. https://doi.org/10.1016/j.brat.2014.08.015.
Crane, R. S., Brewer, J., Feldman, C., Kabat-Zinn, J., Santorelli, S., Williams, J. M. G., & Kuyken, W. (2017). What defines mindfulness-based programs? The warp and the weft. Psychological Medicine, 47(6), 990–999. https://doi.org/10.1017/S0033291716003317.
Creswell, J. D. (2017). Mindfulness interventions. Annual Review of Psychology, 68, 491–516. https://doi.org/10.1146/annurev-psych-042716-051139.
Cuijpers, P., Huibers, M., Ebert, D. D., Koole, S. L., & Andersson, G. (2013). How much psychotherapy is needed to treat depression? A meta-regression analysis. Journal of Affective Disorders, 149, 1–13. https://doi.org/10.1016/j.jad.2013.02.030.
Dane, E., & Brummel, B. J. (2014). Examining workplace mindfulness and its relations to job performance and turnover intention. Human Relations, 67(1), 105–128. https://doi.org/10.1177/0018726713487753.
Davis, D. M., & Hayes, J. A. (2011). What are the benefits of mindfulness? A practice review of psychotherapy-related research. Psychotherapy, 48(2), 198–208. https://doi.org/10.1037/a0022062.
Dekker, J., Molenaar, P. J., Kool, S., VanAalst, G., Peen, J., & deJonghe, F. (2005). Dose-effect relations in time-limited combined psycho-pharmacological treatment for depression. Psychological Medicine, 35, 47–58. https://doi.org/10.1017/S0033291704002685.
Dimidjian, S., Goodman, S. H., Felder, J. N., Gallop, R., Brown, A. P., & Beck, A. (2016). Staying well during pregnancy and the postpartum: a pilot randomized trial of mindfulness-based cognitive therapy for the prevention of depressive relapse/recurrence. Journal of Consulting and Clinical Psychology, 84(2), 134–145. https://doi.org/10.1037/ccp0000068.
Diz, A. P., Carvajal-Rodriguez, A., & Skibinski, D. O. F. (2011). Multiple hypothesis testing in proteomics: a strategy for experimental work. Molecular & Cellular Proteomics, 10(3), 1–10. https://doi.org/10.1074/mcp.M110.004374.
Dobkin, P. L., Irving, J. A., & Amar, S. (2012). For whom may participation in a mindfulness-based stress reduction program be contraindicated? Mindfulness, 3(1), 44–50. https://doi.org/10.1007/s12671-011-0079-9.
Feldman, C., & Kuyken, W. (2011). Compassion in the landscape of suffering. Contemporary Buddhism, 12(1), 143–155. https://doi.org/10.1080/14639947.2011.564831.
Fried, E. I. (2017). The 52 symptoms of major depression: lack of content overlap among seven common depression scales. Journal of Affective Disorders, 208, 191–197. https://doi.org/10.1016/j.jad.2016.10.019.
Fu, R., Gartlehner, G., Grant, M., Shamliyan, T., Sedrakyan, A., Wilt, T. J., Griffith, L., Oremus, M., Raina, P., Ismaila, P., Santaguida, P., Lau, J., & Trikalinos, T. A. (2010, October 25). Conducting quantitative synthesis when comparing medical interventions: AHRQ and the effective health care program. Methods Guide for Effectiveness and Comparative Effectiveness Reviews. Agency for Healthcare Research and Quality. https://www.ncbi.nlm.nih.gov/pubmed/21433407
Gambrel, L., & Piercy, F. P. (2015). Mindfulness-based relationship education for couples expecting their first child – Part 1: a randomized mixed-methods program evaluation. Journal of Marital and Family Therapy, 41(1), 5–24. https://doi.org/10.1111/jmft.12066.
Glenn, D., Gilinelli, D., Rose, R. D., Roy-Byrne, P., Stein, M. B., Sullivan, G., Bystritksy, A., Sherbourne, C., & Craske, M. G. (2013). Who gets the most out of cognitive-behavioral therapy for anxiety disorders? The role of treatment dose and patient engagement. Journal of Consulting and Clinical Psychology, 81(4), 639–649. https://doi.org/10.1037/a0033403.
Glickmann, M. E., Rao, S. R., & Schultz, M. R. (2014). False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. Journal of Clinical Epidemiology, 67, 850–857. https://doi.org/10.1016/j.jclinepi.2014.03.012.
Godfrin, K. A., & van Heeringen, C. (2010). The effects of mindfulness-based cognitive therapy on recurrence of depressive episodes, mental health and quality of life: a randomized controlled study. Behaviour Research and Therapy, 48, 738–746. https://doi.org/10.1016/j.brat.2010.04.006.
Goldberg, S. B., Tucker, R. P., Greene, P. A., Simpson, T. L., Kearney, D. J., & Davidson, R. J. (2017). Is mindfulness research methodology improving over time? A systematic review. PLoS One, 12(10), e0187298. https://doi.org/10.1371/journal.pone.0187298.
Goldberg, S. B., Tucker, R. P., Greene, P. A., Davidson, R. J., Wampold, B. E., Kearney, D. J., & Simpson, T. L. (2018). Mindfulness-based interventions for psychiatric disorders: a systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60. https://doi.org/10.1016/j.cpr.2017.10.011.
Gotink, R. A., Chu, P., Busschbach, J. J. V., Benson, H., Fricchione, L., & Hunink, M. G. M. (2015). Standardized mindfulness-based interventions in healthcare: an overview of systematic reviews and meta-analyses of RCTs. PLoS One, 10(4), e0124344. https://doi.org/10.1371/journal.pone.0124344.
Gu, J., Strauss, C., Bond, R., & Cavanagh, K. (2015). How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review, 37, 1–12. https://doi.org/10.1016/j.cpr.2015.01.006.
Hazlett-Stevens, H., & Oren, Y. (2017). Effectiveness of mindfulness-based stress reduction bibliotherapy: a preliminary randomized controlled trial. Journal of Clinical Psychology, 73, 626–637. https://doi.org/10.1002/jclp.22370.
Hedges, L. V., & Olkin, I. (1985). Statistical methods for meta-analysis. Academic Press.
Higgins, J. P. T., & Green, S. (2008). Cochrane handbook for systematic reviews of interventions. John Wiley & Sons.
Higgins, J. P. T., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., Savović, J., Schulz, K. F., Weeks, L., & Sterne, J. A. C. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ, 343, d5928. https://doi.org/10.1136/bmj.d5928.
Hofmann, S. G., Sawyer, A. T., Witt, A. A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. Journal of Consulting and Clinical Psychology, 78(2), 169–183. https://doi.org/10.1037/a0018555.
Holm, S. (1979). A simple sequential rejective multiple test procedure. Scandinavian Journal of Statistics, 6, 65–70.
Jain, S., Shapiro, S. L., Swanick, S., Roesch, S. C., Mills, P. J., Bell, I., & Schwartz, G. E. (2007). A randomized controlled trial of mindfulness meditation vs. relaxation training: effects on distress, positive states of mind, rumination, and distraction. Annals of Behavioral Medicine, 33(1), 11–21. https://doi.org/10.1207/s15324796abm3301_2.
Kabat-Zinn, J. (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. General Hospital Psychiatry, 4(1), 33–47. https://doi.org/10.1016/0163-8343(82)90026-3.
Kabat-Zinn, J. (1990). Full catastrophe living. Dell Publishing.
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: past, present, and future. Clinical Psychology: Science and Practice, 10, 144–156. https://doi.org/10.1093/clipsy/bpg016.
Kabat-Zinn, J. (2005). Coming to our senses: healing ourselves and the world through mindfulness. Hyperion.
Kabat-Zinn, J. (2013). Full catastrophe living, revised edition: how to cope with stress, pain and illness using mindfulness meditation. Hachette.
Kabat-Zinn, J., & Chapman-Waldrop, A. (1988). Compliance with an outpatient stress reduction program: rates and predictors of program completion. Journal of Behavioral Medicine, 11, 333–352. https://doi.org/10.1007/bf00844934.
Karlsson, P., & Bergmark, A. (2014). Compared with what? An analysis of control-group types in Cochrane and Campbell reviews of psychosocial treatment efficacy with substance use disorders. Addiction, 110, 420–428. https://doi.org/10.1111/add.12799.
Kempton, M. J., Geddes, J. R., Ettinger, U., Williams, S. C. R., & Grasby, P. M. (2008). Meta-analysis, database, and meta-regression of 98 structural imaging studies in bipolar disorder. JAMA Psychiatry, 65(9), 1017–1032. https://doi.org/10.1001/archpsyc.65.9.1017.
Keng, S. L., Smoski, M. J., & Robins, C. J. (2011). Effects of mindfulness on psychological health: a review of empirical studies. Clinical Psychology Review, 31(6), 1041–1056. https://doi.org/10.1016/j.cpr.2011.04.006.
Khoury, B., Sharma, M., Rush, S. E., & Fournier, C. (2015). Mindfulness-based stress reduction for healthy individuals: a meta-analysis. Journal of Psychosomatic Research, 78(6), 519–529. https://doi.org/10.1016/j.jpsychores.2015.03.009.
Klatt, M. D., Buckworth, J., & Malarky, W. B. (2009). Effects of low-dose mindfulness-based stress reduction (MBSR-ld) on working adults. Health Education & Behavior, 36(3), 601–614. https://doi.org/10.1177/1090198108317627.
Knapp, G., & Hartung, J. (2003). Improved tests for a random effects meta-regression with a single covariate. Statistics in Medicine, 22(17), 2693–2710. https://doi.org/10.1002/sim.1482.
Kubo, A., Kurtovich, E., McGinnis, M., Aghee, A., Altschuler, A., Quesenberry, C., Kolevska, T., & Avins, A. L. (2019). A randomized controlled trial of mhealth mindfulness intervention for cancer patients and informal cancer caregivers: a feasibility study within an integrated health care delivery system. Integrative Cancer Therapies, 18, 1–13. https://doi.org/10.1177/1534735419850634.
Kuyken, W., Byford, S., Taylor, R. S., Watkins, E., Holden, E., White, K., Barrett, B., Byng, R., Evans, A., Mullan, E., & Teasdale, J. D. (2008). Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. Journal of Consulting and Clinical Psychology, 76(6), 966–978. https://doi.org/10.1037/a0013786.
Kuyken, W., Warren, F. C., Taylor, R. S., Whalley, B., Crane, C., Bondolfi, G., Hayes, R., Huijbers, M., Ma, H., Schweizer, S., Segal, Z., Speckens, A., Teasdale, J. D., van Heeringen, K., Williams, M., Byford, S., Byng, R., & Dalgleish, T. (2016). Efficacy of mindfulness-based cognitive therapy in prevention of depressive relapse: an individual patient data meta-analysis from randomized trials. JAMA Psychiatry, 73(6), 565–574. https://doi.org/10.1001/jamapsychiatry.2016.0076.
Kvillemo, P., Brandberg, Y., & Bränström, R. (2016). Feasibility and outcomes of an internet-based mindfulness training program: a pilot randomized controlled trial. JMIR Mental Health, 3(3), e33. https://doi.org/10.2196/mental.5457.
Lacaille, J., Sadikaj, G., Nishioka, M., Carriere, K., Flanders, J., & Knaeuper, B. (2018). Daily mindful responding mediates the effect of meditation practice on stress and mood: the role of practice duration and adherence. Journal of Clinical Psychology, 74(1), 109–122. https://doi.org/10.1002/jclp.22489.
Lamothe, M., Rondeau, E., Malboeuf-Hurtubise, C., Duval, M., & Sultan, S. (2016). Outcomes of MBSR or MBSR-based interventions in health care providers: a systematic review with a focus on empathy and emotional competencies. Complementary Therapies in Medicine, 24, 19–28. https://doi.org/10.1016/j.ctim.2015.11.001.
Langer, E. (2014). Mindfulness (25th Anniversary ed.). Da Calp Press.
Leyland, A., Rowse, G., & Emmerson, L. M. (2019). Experimental effects of mindfulness inductions on self-regulation: systematic review and meta-analysis. Emotion, 19(1), 108–122. https://doi.org/10.1037/emo0000425.
Lomas, T., Cartwright, T., Edginton, T., & Ridge, D. (2015). A qualitative analysis of experiential challenges associated with meditation practice. Mindfulness, 6(4), 848–860. https://doi.org/10.1007/s12671-014-0329-8.
Lu, S. (2015). Mindfulness holds promise for treating depression: new research suggests that practicing mindfulness may help prevent a relapse. American Psychological Association, 46(3), 50.
Ma, S. H., & Teasdale, J. D. (2004). Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. Journal of Consulting and Clinical Psychology, 72(1), 31–40. https://doi.org/10.1037/0022-006X.72.1.31.
McHugh, M. L. (2012). Interrater reliability: the kappa statistic. Biochemia Medica, 22(3), 276–282.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & The PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed1000097.
Nakagawa, S. (2004). A farewell to Bonferroni: the problems of low statistical power and publication bias. Behavioural Ecology, 15(6), 1044–1045. https://doi.org/10.1093/beheco/arh107.
Niklicek, I., & Kuijpers, K. F. (2008). Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: is increased mindfulness indeed the mechanism? Annals of Behavioral Medicine, 35, 331–340. https://doi.org/10.1007/s12160-008-9030-2.
Parsons, C. E., Crane, C., Parsons, L. J., Fjorback, L. O., & Kuyken, W. (2017). Home practice in mindfulness-based cognitive therapy and mindfulness-based stress reduction: a systematic review and meta-analysis of participants' mindfulness practice and its association with outcomes. Behaviour Research and Therapy, 95, 29–41. https://doi.org/10.1016/j.brat.2017.05.004.
Ribeiro, L., Atchley, R. M., & Oken, B. S. (2018). Adherence to practice of mindfulness in novice meditators: practices chosen, amount of time practiced, and long-term effects following a mindfulness-based intervention. Mindfulness, 9(2), 401–411. https://doi.org/10.1007/s12671-017-0781-3.
Rosenzweig, S., Greeson, J. M., Reibel, D. K., Green, J. S., Jasser, S. A., & Beasley, D. (2010). Mindfulness-based stress reduction for chronic pain conditions: variation in treatment outcomes and role of home meditation practice. Journal of Psychosomatic Research, 68, 29–36. https://doi.org/10.1016/j.jpsychores.2009.03.010.
Schellekens, M. P. J., van den Hurk, D. G. M., Prins, J. B., Donders, A. R. T., Molema, J., Dekhuijzen, R., van der Drift, M. A., & Speckens, A. E. M. (2017). Mindfulness-based stress reduction added to care as usual for lung cancer patients and/or their partners: a multicentre randomized controlled trial. Psycho-Oncology, 26, 2118–2126. https://doi.org/10.1002/pon.4430.
Schumer, M. C., Lindsay, E. K., & Creswell, J. D. (2018). Brief mindfulness training for negative affectivity: a systematic review and meta-analysis. Journal of Consulting and Clinical Psychology, 86(7), 569–583. https://doi.org/10.1037/ccp0000324.
Schwarzer, G. (2007). Meta: an R package for meta-analysis. R News, 7(3), 40–45.
Segal, Z. V., Williams, M. G., & Teasdale, J. D. (2002). Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. Guildford Press.
Shapiro, S. L., Astin, J. A., Bishop, S. R., & Cordova, M. (2005). Mindfulness-based stress reduction for health care professionals: results from a randomized trial. International Journal of Stress Management, 12(2), 164–176. https://doi.org/10.1037/1072-5245.12.2.164.
Spijkerman, M. P. J., Pots, W. T. M., & Bohlmeijer, E. T. (2016). Effectiveness of online mindfulness-based interventions in improving mental health: a review and meta-analysis of randomized controlled trials. Clinical Psychology Review, 45, 102–114. https://doi.org/10.1016/j.cpr.2016.03.009.
Strauss, C., Cavanagh, K., Oliver, A., & Pettman, D. (2014). Mindfulness-based interventions for people diagnosed with a current episode of an anxiety or depressive disorder: a meta-analysis of randomized controlled trials. PLoS One, 9(4), e96110. https://doi.org/10.1371/journal.pone.0096110.
Teasdale, J. D., Segal, Z. V., Williams, J. M. G., Ridgeway, V. A., Soulsby, J. M., & Lau, M. A. (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology, 68(4), 615–623. https://doi.org/10.1037//0022-006X.68.4.615.
The Cochrane Collaboration. (2012). Review manager (RevMan) (version 5.2) [computer program]. Copenhagen: The Nordic Cochrane Centre.
The R Foundation for Statistical Computing. (2017). [Computer program]. https://www.r-project.org/foundation/.
Thomas, J. (2017). Brief mindfulness training in the social work practice classroom. Social Work Education, 36(1), 102–118. https://doi.org/10.1080/02615479.2016.1250878.
van Dam, N. T., van Vugt, M. K., Vago, D. R., Schmalzl, L., Saron, C. D., Olendzki, A., Meissner, T., Lazar, S. W., Kerr, C. E., Gorchov, J., Fox, K. C. R., Field, B. A., Britton, W. B., Brefczynski-Lewis, J. A., & Meyer, D. E. (2018). Mind the hype: a critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspectives on Psychological Science, 13(1), 36–61. https://doi.org/10.1177/1745691617709589.
Vettese, L. C., Toneatto, T., Stea, J. N., Nguyen, L., & Wang, J. J. (2009). Do mindfulness meditation participants do their homework? And does it make a difference? A review of the empirical evidence. Journal of Cognitive Psychotherapy: An International Quarterly, 23(3), 198–225. https://doi.org/10.1891/0889-8391.23.3.198.
Viechtbauer, W. (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36(3), 1–48. http://www.jstatsoft.org/v36/i03/.
Virgili, M. (2015). Mindfulness-based interventions reduce psychological distress in working adults: a meta-analysis of intervention studies. Mindfulness, 6(2), 326–337. https://doi.org/10.1007/s12671-013-0264-0.
Wickham, H. (2009). ggplot2: elegant graphics for data analysis. Springer-Verlag.
Williams, J. M. G. (2008). Mindfulness, depression and modes of mind. Cognitive Therapy and Research, 32, 721. https://doi.org/10.1007/s10608-008-9204-z.
Williams, J. M. G., Alatiq, Y., Crane, C., Barnhofer, T., Fennell, M. J. V., Duggan, D. S., Hepburn, A., & Goodwin, G. M. (2008). Mindfulness-based cognitive therapy (MBCT) in bipolar disorder: preliminary evaluation of immediate effects on between-episode functioning. Journal of Affective Disorders, 107, 275–279. https://doi.org/10.1016/j.jad.2007.08.022.
Yalom, I. D. (1983). Inpatient group psychotherapy. Basic Books.
Zautra, A. J., Davis, M. C., Reich, J. W., Nicassio, P., Tennen, H., Finan, P., Kratz, A., Parrish, B., & Irwin, M. R. (2008). Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. Journal of Consulting and Clinical Psychology, 76(3), 408–421. https://doi.org/10.1037/0022-006X.76.3.408.
Acknowledgments
This work was carried out as part of a PhD in Psychology. The author would like to thank Fergal Jones (FJ), Clara Strauss (CS) and Kate Cavanagh (KC) for their supervision and consultation and for their scientific contributions. In particular, the author would like to thank Fergal Jones for his valuable help in the final preparation of the manuscript and Sabina Hulbert for statistical consultation. The author would also like to thank the authors of included studies who supplied the additional data and information needed for the meta-regression.
Review Registration
PROSPERO International prospective register of systematic reviews registration number: CRD42017056864.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares that she has no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(PDF 1825 kb)
Rights and permissions
About this article
Cite this article
Strohmaier, S. The Relationship Between Doses of Mindfulness-Based Programs and Depression, Anxiety, Stress, and Mindfulness: a Dose-Response Meta-Regression of Randomized Controlled Trials. Mindfulness 11, 1315–1335 (2020). https://doi.org/10.1007/s12671-020-01319-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-020-01319-4