Abstract
Background
Sepsis remains a global health burden associated with significant morbidity and mortality. Bacteria are known to be the predominant pathogens in sepsis; however, viral etiologies in sepsis are still under diagnosed. Respiratory viral pathogens have been previously linked to sepsis, but the knowledge of incidence, disease burden and mortality of viral-induced sepsis remains limited. This study aimed at understanding the role of respiratory viral infections in the causation of sepsis in liver disease patients.
Methods
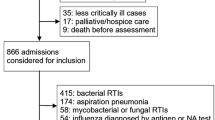
In this retrospective study, the clinical records of liver disease patients with influenza-like illness, whose requests for respiratory viral testing were received from January 2019 to December 2022, were reviewed. Respiratory viruses were identified using FilmArray 2.0 respiratory panel (BioFire Diagnostics, Utah, USA).
Results
Of 1391 patients tested, a respiratory viral etiology was detected in 23%. The occurrence of sepsis was seen in 35%. Among these, isolated viral etiology with no other bacterial/fungal coinfection was found in 55% of patients. Rhinovirus/Enterovirus was found as the most common underlying viral etiology (23.4%). The sepsis prevalence was higher among patients with associated comorbidities (45%) and decompensated cirrhosis (84%). On multi-variable analysis, no factor was found independently associated with sepsis-related mortality.
Conclusion
This study underlines the importance of isolated viral etiology in causation of sepsis among liver disease patients. Patients with comorbidities, older age and decompensated cirrhosis are at an increased risk of developing sepsis and are associated with poorer outcomes. Accurate and timely identification of the viral etiology in sepsis would prevent the misuse of antibiotics and improve overall patient care.
Graphical abstract



Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801–10. https://doi.org/10.1001/jama.2016.0287.
Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395:200–11. https://doi.org/10.1016/S0140-6736(19)32989-7.
Phua J, Ngerng W, See K, et al. Characteristics and outcomes of culture-negative versus culture-positive severe sepsis. Crit Care. 2013;17:R202. https://doi.org/10.1186/cc12896.
Vincent JL, Sakr Y, Sprung CL, et al. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med. 2006;34:344–53. https://doi.org/10.1097/01.ccm.0000194725.48928.3a.
Southeast Asia Infectious Disease Clinical Research Network. Causes and outcomes of sepsis in southeast Asia: a multinational multicentre cross-sectional study. Lancet Glob Health. 2017;5:e157-67. https://doi.org/10.1016/S2214-109X(17)30007-4.
Gu X, Zhou F, Wang Y, Fan G, Cao B. Respiratory viral sepsis: epidemiology, pathophysiology, diagnosis and treatment. Eur Respir Rev. 2020;29:200038. https://doi.org/10.1183/16000617.0038-2020.
Cillóniz C, Dominedò C, Magdaleno D, Ferrer M, Gabarrús A, Torres A. Pure viral sepsis secondary to community-acquired pneumonia in adults: Risk and prognostic factors. J Infect Dis. 2019;220:1166–71. https://doi.org/10.1093/infdis/jiz257.
Zhao H, Liu Y, Feng Z, et al. A fatal case of viral sepsis and encephalitis in a child caused by human adenovirus type 7 infection. Virol J. 2022;19:154. https://doi.org/10.1186/s12985-022-01886-z.
Li H, Liu L, Zhang D, et al. SARS-CoV-2 and viral sepsis: observations and hypotheses. Lancet. 2020;395:1517–20. https://doi.org/10.1016/S0140-6736(20)30920-X.
Metz M, Gualdoni GA, Winkler HM, et al. MxA for differentiating viral and bacterial infections in adults: a prospective, exploratory study. Infection. 2023;51:1329–37. https://doi.org/10.1007/s15010-023-01986-0.
Poritz MA, Blaschke AJ, Byington CL, et al. Film Array, an automated nested multiplex PCR system for multi-pathogen detection: development and application to respiratory tract infection. PLoS One. 2011;6:e26047. [Erratum in: PLoS One. 2011;6. doi: 10.1371/annotation/468cfdcd-184c-42f7-a1d0-3b72a2f6a558] https://doi.org/10.1371/journal.pone.0026047.
WHO. Global Epidemiological Surveillance Standards for Influenza. (Available from: http://www.who.int/influenza/resources/documents/WHO_Epidemiological_Influenza_Surveillance_Standards_2014.pdf). Accessed on 5th July, 2023.
Fang W, Wu J, Cheng M, et al. Diagnosis of invasive fungal infections: challenges and recent developments. J Biomed Sci. 2023;30:42. https://doi.org/10.1186/s12929-023-00926-2.
Abumayyaleh M, Nuñez-Gil IJ, El-Battrawy I, et al. Sepsis of Patients Infected by SARS-CoV-2: Real-World Experience From the International HOPE-COVID-19-Registry and Validation of HOPE Sepsis Score. Front Med (Lausanne). 2021;8:728102. https://doi.org/10.3389/fmed.2021.728102.
Lin GL, McGinley JP, Drysdale SB, Pollard AJ. Epidemiology and Immune Pathogenesis of Viral Sepsis. Front Immunol. 2018;9:2147. https://doi.org/10.3389/fimmu.2018.02147.
Premkumar M, Devurgowda D, Dudha S, et al. A/H1N1/09 Influenza is associated with high mortality in liver cirrhosis. J Clin Exp Hepatol. 2019;9:162–70. https://doi.org/10.1016/j.jceh.2018.04.006.
Samal J, Agarwal R, Soni A, Pandey A, Thapar S, Gupta E. Coinfection of SARS-CoV-2 with other respiratory pathogens in patients with liver disease. Access Microbiol. 2022;4:acmi000456. https://doi.org/10.1099/acmi.0.000456.
Sarin SK, Choudhury A, Lau GK, et al. Pre-existing liver disease is associated with poor outcome in patients with SARS CoV2 infection; The APCOLIS Study (APASL COVID-19 Liver Injury Spectrum Study). Hepatol Int. 2020;14:690–700. https://doi.org/10.1007/s12072-020-10072-8.
Nam HH, Ison MG. Respiratory syncytial virus infection in adults. BMJ 2019;366:l5021. https://doi.org/10.1136/bmj.l5021.
Liu J, Zhao H, Feng Z, et al. A severe case of human rhinovirus A45 with central nervous system involvement and viral sepsis. Virol J. 2022;19:72. https://doi.org/10.1186/s12985-022-01799-x.
Bajpai V, Gupta E, Mitra LG, et al. Spectrum of respiratory viral infections in liver disease patients with cirrhosis admitted in critical care unit. J Lab Physicians. 2019;11:356–60. https://doi.org/10.4103/JLP.JLP_6_19.
Tsao YT, Tsai YH, Liao WT, Shen CJ, Shen CF, Cheng CM. Differential markers of bacterial and viral infections in children for point-of-care testing. Trends Mol Med. 2020;26:1118–32. https://doi.org/10.1016/j.molmed.2020.09.004.
Maras JS, Sharma S, Bhat A, et al. Multi-omics analysis of respiratory specimen characterizes baseline molecular determinants associated with SARS-CoV-2 outcome. iScience. 2021;24:102823. https://doi.org/10.1016/j.isci.2021.102823.
Piri R, Yahya M, Ivaska L, et al. Myxovirus Resistance Protein A as a Marker of Viral Cause of Illness in Children Hospitalized with an Acute Infection. Microbiol Spectr. 2022;10:e0203121. https://doi.org/10.1128/spectrum.02031-21.
Rhedin S, Eklundh A, Ryd-Rinder M, et al. Myxovirus resistance protein A for discriminating between viral and bacterial lower respiratory tract infections in children - The TREND study. Clin Microbiol Infect. 2022;28:1251–7. https://doi.org/10.1016/j.cmi.2022.05.008.
Lehtinen O, Broman N, Waris M, et al. Association of human myxovirus resistance protein A with severity of COVID-19. BMC Infect Dis. 2022;22:755. https://doi.org/10.1186/s12879-022-07753-0.
Self WH, Rosen J, Sharp SC, et al. Diagnostic accuracy of FebriDx: A rapid test to detect immune responses to viral and bacterial upper respiratory infections. J Clin Med. 2017;6:94. https://doi.org/10.3390/jcm6100094.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
EG: Conceptualization, final manuscript editing, supervision and project administration, JS: Manuscript writing and study design; RM and HT: Manuscript editing and clinical data evaluation, MG: manuscript editing, NR: Data compilation, TP: Statistical analysis, MP: Data analysis and manuscript editing, AT: Clinical data evaluation, RA: Data interpretation and manuscript editing and PK, VK and SA: Clinical data evaluation.
Corresponding author
Ethics declarations
Conflict of interest
EG, JS, RM, HT, MG, NR, TP, MP, AT, RA, PK, VK and SA declare that they have no conflict of interest pertaining to this article.
Institutional review board
The Institutional Review Board (Institutional Ethics Committee, ILBS) reviewed and approved the study (Ethical Approval Number—IEC/2021/84/MA10). The study was conducted as per the policy of the Declaration of Helsinki. The Institutional Review Board (Institutional Ethics Committee, ILBS) waived informed consent because the study was based on the retrospective analysis of existing clinical data. Patient records or information were anonymized and de-identified before analysis.
Informed consent
This was a retrospective study, so patient informed consent was waived.
Disclaimer
The authors are solely responsible for the data and the content of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, the Indian Society of Gastroenterology or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gupta, E., Samal, J., Maiwall, R. et al. Respiratory tract viral infections associated sepsis in patients with underlying liver disease: Viral sepsis an entity to look forward!. Indian J Gastroenterol (2024). https://doi.org/10.1007/s12664-024-01536-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12664-024-01536-y