Abstract
Background
Reduction in height of barium column in timed barium esophagogram (TBE) and lower esophageal sphincter (LES) pressure on manometry has been used to assess efficacy of pneumatic dilation (PD) in patients with achalasia; data comparing these two methods to assess efficacy of PD are scanty.
Methods
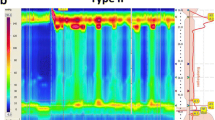
Sixty-two patients with achalasia undergoing PD were evaluated clinically (Eckardt’s score), high-resolution manometry (HRM), and TBE (films at 1 and 5 min) before and 4 weeks after PD using 30 and 35 mm Rigiflex balloon (Microvasive, Milliford, MA, USA) in female and male patients, respectively. Response was defined clinically as Eckardt’s score <3, by manometry as LES pressure <22.5 mmHg, and by TBE as adequate esophageal emptying (reduction in height of barium column by more than 50 % of pretreatment value in 5-min radiograph).
Results
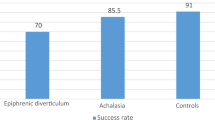
Forty-three out of sixty-two (69 %) patients [age 34 ± 12 years, 36 (58 %) male] responded, and 19 (31 %) did not respond to the first session of PD as assessed by post-PD Eckardt’s score. Thirty-eight out of 43 (88 %) responders had adequate esophageal emptying of barium in TBE, while 31/43 (72 %) had LES pressure below 22.5 mmHg on HRM (p = ns). Eight out of 19 (42 %) nonresponders showed failure in esophageal emptying (defined by lack of reduction in height of barium column by 50 %) in TBE, and 11/19 (58 %) had LES pressure >22.5 mmHg (p = ns). Kaplan–Meier analysis showed that response on TBE and HRM at 1 month predicted clinical response well during 6 months follow up.
Conclusion
TBE and esophageal HRM were comparable in assessing efficacy of PD in treatment of achalasia.




Similar content being viewed by others
References
Castell DO. Motor disorders of the esophagus. N Engl J Med. 1979;301:1124.
Ghoshal UC, Aggarwal R, Kumar S, Naik SR. Pneumatic dilation versus intrasphincteric botulinum toxin injection in the treatment of achalasia cardia in India: an economic analysis. Indian J Gastroenterol. 2002;21:193–6.
Ghoshal UC, Kumar S, Saraswat VA, Aggarwal R, Misra A, Choudhuri G. Long-term follow-up after pneumatic dilation for achalasia cardia: factors associated with treatment failure and recurrence. Am J Gastroenterol. 2004;99:2304–10.
Swanstrom LL, Kurian A, Dunst CM, Sharata A, Bhayani N, Rieder E. Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg. 2012;256:659–67.
Vaezi MF, Baker ME, Achkar E, Richter JE. Timed barium oesophagram: better predictor of long term success after pneumatic dilation in achalasia than symptom assessment. Gut. 2002;50:765–70.
Eckardt VF, Aignherr C, Bernhard G. Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology. 1992;103:1732–8.
Rohof WO, Lei A, Boeckxstaens GE. Esophageal stasis on a timed barium esophagogram predicts recurrent symptoms in patients with long-standing achalasia. Am J Gastroenterol. 2013;108:49–55.
Pandolfino JE, Ghosh SK, Zhang Q, Jarosz A, Shah N, Kahrilas PJ. Quantifying EGJ morphology and relaxation with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol. 2006;290:G1033–40.
Conklin JL. Evaluation of esophageal motor function with high-resolution manometry. J Neurogastroenterol Motil. 2013;19:281–94.
Eckardt AJ, Eckardt VF. Current clinical approach to achalasia. World J Gastroenterol. 2009;15:3969–75.
Ghoshal UC, Rangan M, Misra A. Pneumatic dilation for achalasia cardia: reduction in lower esophageal sphincter pressure in assessing response and factors associated with recurrence during long-term follow up. Dig Endosc. 2011;24:7–15.
Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology. 2008;135:1526–33.
Lin Z, Kahrilas PJ, Roman S, Boris L, Carlson D, Pandolfino JE. Refining the criterion for an abnormal integrated relaxation pressure in esophageal pressure topography based on the pattern of esophageal contractility using a classification and regression tree model. Neurogastroenterol Motil. 2012;24:e356–63.
Neyaz Z, Gupta M, Ghoshal UC. How to perform and interpret timed barium esophagogram. J Neurogastroenterol Motil. 2013;19:251–6.
Ghoshal UC, Rangan M. A review of factors predicting outcome of pneumatic dilation in patients with achalasia cardia. J Neurogastroenterol Motil. 2011;17:9–13.
Farhoomand K, Connor JT, Richter JE, Achkar E, Vaezi MF. Predictors of outcome of pneumatic dilation in achalasia. Clin Gastroenterol Hepatol. 2004;2:389–94.
Farrokhi F, Vaezi MF. Idiopathic (primary) achalasia. Orphanet J Rare Dis. 2007;2:38.
Kostic S, Kjellin A, Ruth M, et al. Pneumatic dilatation or laparoscopic cardiomyotomy in the management of newly diagnosed idiopathic achalasia. Results of a randomized controlled trial. World J Surg. 2007;31:470–8.
Lake JM, Wong RK. Review article: the management of achalasia—a comparison of different treatment modalities. Aliment Pharmacol Ther. 2006;24:909–18.
Wang L, Li YM, Li L. Meta-analysis of randomized and controlled treatment trials for achalasia. Dig Dis Sci. 2009;54:2303–11.
Vela MF, Richter JE, Khandwala F, et al. The long-term efficacy of pneumatic dilatation and Heller myotomy for the treatment of achalasia. Clin Gastroenterol Hepatol. 2006;4:580–7.
Karamanolis G, Sgouros S, Karatzias G, et al. Long-term outcome of pneumatic dilation in the treatment of achalasia. Am J Gastroenterol. 2005;100:270–4.
Lopushinsky SR, Urbach DR. Pneumatic dilatation and surgical myotomy for achalasia. JAMA. 2006;296:2227–33.
Eckardt VF, Gockel I, Bernhard G. Pneumatic dilation for achalasia: late results of a prospective follow up investigation. Gut. 2004;53:629–33.
Gelfand MD, Kozarek RA. An experience with polyethylene balloons for pneumatic dilation in achalasia. Am J Gastroenterol. 1989;84:924–7.
Vaezi MF, Baker ME, Richter JE. Assessment of esophageal emptying post-pneumatic dilation: use of the timed barium esophagram. Am J Gastroenterol. 1999;94:1802–7.
Kostic SV, Rice TW, Baker ME, et al. Timed barium esophagogram: a simple physiologic assessment for achalasia. J Thorac Cardiovasc Surg. 2000;120:935–43.
Oezcelik A, Hagen JA, Halls JM, et al. An improved method of assessing esophageal emptying using the timed barium study following surgical myotomy for achalasia. J Gastrointest Surg. 2009;13:14–8.
Mikaeli J, Islami F, Malekzadeh R. Achalasia: a review of Western and Iranian experiences. World J Gastroenterol. 2009;15:5000–9.
Pratap N, Reddy DN. Can achalasia subtyping by high-resolution manometry predict the therapeutic outcome of pneumatic balloon dilatation?: author's reply. J Neurogastroenterol Motil. 2011;17:205.
Conflict of interest
UCG, MG, AV, ZN, SM, AM, and VAS have no conflict of interest to declare.
Ethics statement
The study was performed in a manner to conform with the Helsinki Declaration of 1975, as revised in 2000 and 2008 concerning Human and Animal Rights, and the authors followed the policy concerning Informed Consent as shown on Springer.com.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ghoshal, U.C., Gupta, M., Verma, A. et al. High-resolution manometry is comparable to timed barium esophagogram for assessing response to pneumatic dilation in patients with achalasia. Indian J Gastroenterol 34, 144–151 (2015). https://doi.org/10.1007/s12664-015-0551-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-015-0551-x