Abstract
Purpose
Interventional pulmonology is a growing subspecialty of pulmonary medicine with flexible and rigid bronchoscopies increasingly used by interventional pulmonologists for advanced diagnostic and therapeutic purposes. This review discusses different technical aspects of anesthesia for interventional pulmonary procedures with an emphasis placed on pharmacologic combinations, airway management, ventilation techniques, and common complications.
Source
Relevant medical literature was identified by searching the PubMed and Google Scholar databases for publications on different anesthesia topics applicable to interventional pulmonary procedures. Cited literature included case reports, original research articles, review articles, meta-analyses, guidelines, and official society statements.
Principal findings
Interventional pulmonology is a rapidly growing area of medicine. Anesthesiologists need to be familiar with different considerations required for every procedure, particularly as airway access is a shared responsibility with pulmonologists. Depending on the individual case characteristics, a different selection of airway method, ventilation mode, and pharmacologic combination may be required. Most commonly, airways are managed with supraglottic devices or endotracheal tubes. Nevertheless, patients with central airway obstruction or tracheal stenosis may require rigid bronchoscopy and jet ventilation. Although anesthetic approaches may vary depending on factors such as the length, complexity, and acuity of the procedure, the majority of patients are anesthetized using a total intravenous anesthetic technique.
Conclusions
It is fundamental for the anesthesia provider to be updated on interventional pulmonology procedures in this rapidly growing area of medicine.
Résumé
Objectif
La pneumologie interventionnelle est une sous-spécialité de la pneumologie en progression grâce à l’utilisation croissante des bronchoscopes souples et rigides par les pneumologues interventionnels à des fins diagnostiques et thérapeutiques avancées. Cette analyse aborde les différents aspects techniques de l’anesthésie pour les procédures interventionnelles en pneumologie en insistant sur les combinaisons pharmacologiques, la gestion des voies respiratoires, les techniques de ventilation et les complications fréquentes.
Source
La littérature médicale pertinente a été identifiée par une recherche des publications sur différents sujets d’anesthésie applicables aux procédures interventionnelles en pneumologie dans les bases de données PubMed et Google Scholar. Les publications citées ont inclus des rapports de cas, des articles de recherche originale, des articles de synthèse, des méta-analyses, des lignes directrices et les déclarations officielles de sociétés savantes.
Constatations principales
La pneumologie interventionnelle est une branche de la médecine qui se développe rapidement. Les anesthésiologistes ont besoin de se familiariser avec les différents problèmes soulevés par chaque procédure, en particulier dans la mesure où la responsabilité de l’accès aux voies respiratoires est partagée avec les pneumologues. La méthode de gestion des voies aériennes, le mode de ventilation et la combinaison pharmacologique pourront être choisis en fonction des caractéristiques de chaque cas particulier. Le plus souvent, les voies respiratoires sont gérées avec des dispositifs supraglottiques ou des tubes endotrachéaux. Néanmoins, les patients présentant une obstruction centrale des voies respiratoires ou une sténose de la trachée peuvent nécessiter le recours à un bronchoscope rigide et à une jet-ventilation. Bien que la démarche anesthésique puisse varier en fonction de facteurs tels que la durée, la complexité et la gravité de la procédure, la majorité des patients sont anesthésiés en employant une technique intraveineuse totale.
Conclusions
Il est essentiel que le professionnel assurant l’anesthésie connaisse les plus récentes procédures interventionnelles en pneumologie dans ce domaine rapidement croissant de la médecine.
Similar content being viewed by others
Interventional pulmonology is a growing subspecialty in pulmonary medicine with remarkable advancements in recent years having been made in diagnostic and therapeutic innovations.1,2 A growing number of procedures are performed by interventional pulmonologists. Different procedures require different anesthetic considerations based on the complexity of the procedure performed and underlying patient conditions; these range from conscious sedation to general anesthesia, including the use of either conventional or jet ventilation.3,4 Hence, it is fundamental for anesthesiologists to be familiar with the nuances of the different techniques commonly performed by interventional pulmonologists.
Rigid bronchoscope, manual jet ventilator, and automatic jet ventilator. a. Volume ventilation adaptor. b. Jet ventilation adaptor (arrow points at ventilator port). c. Rigid bronchoscope with lateral fenestrations and beveled tip. d. Rigid tracheoscope. e. Manual jet ventilator with barometer (Sanders jet ventilator). f. Automatic mechanical jet ventilator (Monsoon®, Acutronic medical systems). Note the * and the † at the end of the jet ventilators are connected to the port (arrow) on the adaptor (b)
This narrative review addresses the various methods used for securing the airway as well as the pharmacologic considerations, ventilation modes, and potential complications relevant to the different interventional bronchoscopic procedures.
Pre-procedure assessment
Over 500,000 bronchoscopies are performed annually in the United States5 to address many conditions including malignancy (i.e., for diagnostic, staging, and palliative purposes), interstitial lung disease, asthma, and central airway obstruction.6 Current American Thoracic Society recommendations state that, based on the patient’s underlying condition and physician’s criteria, a full preoperative evaluation (including a full physical examination, laboratory tests, and relevant imaging) should be done prior to bronchoscopy.7 Emphasis should be placed on airway assessment and identification of challenging airway predictors.3,8 Interventional pulmonologists and anesthesiologists should plan each case collaboratively to minimize complications.
Generally, bronchoscopic procedures may be classified as basic diagnostic, advanced diagnostic, and/or therapeutic procedures. These are summarized in Table 1.
Flexible bronchoscopy
Procedure description
The flexible bronchoscope has become an increasingly popular tool over the past years following its introduction in 1968 by Ikeda et al.9 It involves an endoscopic minimally invasive approach to the tracheobronchial tree allowing airway visualization from the nares to the subsegmental bronchi.5 The development of various devices, including brushes, forceps, needles, laser probes, cryoprobes, argon plasma coagulation, electrocautery devices, ultrasound probes (linear and radial), inflatable balloons, and others compatible with the flexible bronchoscope, has increased the diagnostic and therapeutic applications for this technique (Table 2).10,11
Tissue biopsies can be adequately obtained from mediastinal and hilar lymph nodes using transbronchial needle aspiration (TBNA) and from airway or parenchymal lesions with endobronchial and transbronchial forceps biopsies.12,13,14,15 Endobronchial lesions such as tumours and strictures can be debrided, resected/excised, cauterized, dilated, and/or ablated using flexible bronchoscopy.16 Other procedures performed using flexible bronchoscopy include foreign body removal, bronchioalveolar lavage (BAL), airway stenting (self-expanding metallic airways stents, both covered and uncovered), bronchial thermoplasty, intrabronchial valve placement, and photodynamic therapy.17,18,19,20,21,22 Anesthesiologists should be familiar with these and their potential complications.23
Endobronchial ultrasound (EBUS)-TBNA is the preferred method for mediastinal and hilar lymph node sampling. Using real-time ultrasound imaging, this technique achieves a sensitivity and negative predictive value close to 90% with a very low complication rate (< 0.5%).11,24,25 Radial probe EBUS uses a 360°-view small-sized ultrasound probe that fits through the working channel of a flexible bronchoscope. It is typically used in conjunction with standard bronchoscopy using a guide sheath or navigational techniques, such as electromagnetic navigation bronchoscopy (ENB) or virtual bronchoscopy (VB). Radial EBUS provides a real-time confirmation of the location of a peripheral lung lesion reached by a navigation method.26,27,28
Electromagnetic navigation bronchoscopy is a minimally invasive approach to reach peripheral lesions. A locator guide is tracked in the electromagnetic field and blended with the existing chest computed tomography data. The locator guide and a sheath, which are steerable, are advanced together in real time based on the virtual imaging and system guidance of direction and distance. Once the lesion is reached, the locatable guide is removed and the working sheath is left in place at the target through which instruments such as a radial EBUS, brush, and forceps can be passed.29
Bronchoscopy-guided technologies such as ENB,26,29 VB,30 radial probe endobronchial ultrasound,27,28 and ultrathin bronchoscopes with guided sheaths have been developed to improve the diagnostic yield of transbronchial biopsy for solitary pulmonary nodule diagnosis.31 A recent meta-analysis showed that the pooled diagnostic yield of guided bronchoscopy using one or a combination of the above modalities was 70%.30
Anesthetic depth and pharmacologic considerations
Pharmacologic approaches vary depending on the indication for bronchoscopy and complexity of the case being undertaken. Basic bronchoscopy procedures are performed under minimal to moderate procedural sedation (i.e., monitored anesthesia care). On the contrary, advanced diagnostic and therapeutic bronchoscopy procedures often require more complex techniques with deep sedation (or even general anesthesia) as defined by the American Society of Anesthesiologists.32
According to American College of Chest Physicians (ACCP) recommendations, all patients undergoing bronchoscopy should receive some degree of sedation (unless contraindicated), as this improves patient satisfaction and procedure tolerability. For this, the ACCP supports the use of propofol alone as a safe and efficient method for bronchoscopy sedation. Nevertheless, it acknowledges the possibility of using regimens of short-acting benzodiazepines, such as midazolam, in combination with an opioid (which itself may be beneficial for its antitussive properties).33
A recently published survey conducted in Switzerland evaluated the practice of 299 pulmonologists and included 27,149 bronchoscopies. It revealed that most basic bronchoscopy cases are performed using propofol, with or without midazolam and/or fentanyl. Interestingly, in this cohort, propofol was administered by the proceduralist in 84% of cases without the presence of an anesthesiologist, with extremely low (0.02%) complication rates (mainly apnea and hypotension).34 A recent retrospective study conducted in Germany assessed nearly 1,600 basic diagnostic bronchoscopy procedures to compare different moderate sedation combinations. Its results support the administration of moderate sedation with triple-sedative combinations (propofol, midazolam, and fentanyl) because it reduces the total dosage of each medication administered without increasing the incidence of adverse events.35 Nevertheless, the addition of short-acting opioid infusions to propofol infusions during bronchoscopy must be closely monitored as they have been associated with lower oxygen saturation levels (SaO2) compared with propofol infusions alone.36 Patient premedication with hydrocodone (4-5 mg iv) prior to propofol-based sedation for bronchoscopy effectively reduces cough during the procedure, increases patient and proceduralist satisfaction, and decreases the total propofol dose required to achieve adequate sedation levels. This measure is most effective for complex procedures such as BAL or TBNA.37
Infusion regimens using total intravenous anesthesia (TIVA) for either moderate to deep sedation or general anesthesia have been described for certain bronchoscopic procedures. Propofol infusions are seen in everyday practice with different pharmacologic combinations depending on each patient and the procedure performed. Effective dosing schemes have been described with an initial bolus of 0.5-1.0 mg·kg−1 followed by an infusion that can be titrated from 75 µg·kg−1·min−1 to 250 µg·kg−1·min−1, depending on the anesthetic depth desired.17,23,38 The administration of propofol can be guided safely based on electroencephalographic methods and its routine use has been be encouraged by some.39 For short-duration bronchoscopic procedures that require moderate sedation, propofol boluses should be preferred over midazolam boluses as these are associated with shorter recovery times and lower levels of reported pain, nausea, and breathlessness postoperatively.39 Depending on local regulations, propofol should only be administered in the presence of a certified anesthesia provider because it has a narrow therapeutic window that can quickly result in general anesthesia and respiratory depression.17 Other studies have validated the addition of other sedative agents to propofol infusions, such as ketamine, that also favor hemodynamic stability.40 Recently published literature shows that the addition of ketamine to midazolam and propofol infusions is as effective (to achieve sedation and analgesia) and as safe (in terms of hemodynamic and respiratory stability) as the addition of fentanyl to midazolam and propofol combinations.41 Hypotension induced by propofol infusion can almost always be adequately managed with boluses of phenylephrine or ephedrine.23
The use of topical anesthetics is recommended by the ACCP for both basic and advanced bronchoscopy as it reduces the dose of sedative agents needed and effectively decreases cough.42 Successful suppression of the gag reflex can be achieved by spraying lidocaine 1% directly over the oropharynx, vocal cords, and aryepiglottic folds.43 Lidocaine 1% is generally a preferred concentration (over 2%) for topical anesthesia during bronchoscopy, as it has been shown to achieve equal patient and operator satisfaction levels while delivering a significantly lower total drug dose.44
Lastly, volatile agents are highly discouraged because bronchoscopic procedures require constant suctioning of the airways, making it impossible to determine the concentration of the agent delivered to the patient (risking inadequate depth of anesthesia in the patient and significant contamination of the procedural room).23,38
Specific advanced bronchoscopic procedures such as EBUS-TBNA may be performed with moderate to deep sedation or general anesthesia as shown by recently published literature. Nevertheless, conflicting evidence exists regarding the impact that sedation level has on the diagnostic yield, complication rate, and procedure tolerability.45,46 Hence, the sedation method selection for EBUS-TBNA should be made individually, considering the operator’s experience, patient preference, local resources (i.e., access to an anesthesiologist), and procedure duration.47 A common practice for this purpose includes an infusion using propofol (75-250 µg·kg−1·min−1) along with small boluses of opioids (fentanyl or remifentanil).38
Dynamic flexible bronchoscopy, a protocol used to diagnose tracheobronchomalacia, requires dynamic airway maneuvers. This procedure is often performed under minimal sedation and abundant topical anesthesia that allows forced inspiratory and expiratory maneuvers while diminishing cough and patient anxiety. Minimal sedation for this situation can be adequately achieved using fentanyl and midazolam boluses as needed during the procedure [mean (standard deviation) total dose per procedure has been reported as fentanyl 37.5 (12.5) µg, midazolam 1.5 (0.5) mg].43
Patients undergoing bronchial thermoplasty (for severe asthma) or Chartis assessment (of collateral ventilation in patients who are candidates for endoscopic lung volume reduction with endobronchial valves) may benefit from small doses of anticholinergics (i.e., 10 µg·kg−1 atropine iv or im or glycopyrrolate 5 µg·kg−1 iv) as premedication to reduce bronchial secretions.48 Nevertheless, the ACCP discourages the routine use of anticholinergics as current evidence fails to show a general clinical benefit.42
Airway and ventilation modes
Depending on the procedure performed, as well as patient medical comorbidities, different modalities of airway-securing devices can be used. Selected short-duration procedures can be safely performed under minimal to moderate sedation with spontaneous ventilation and no airway-securing device. A bite block should be placed to protect the bronchoscope and the patient’s teeth. In patients able to maintain spontaneous ventilation while undergoing endoscopic airway surgery, the use of humidified high-flow nasal oxygen (HFNO) (40-60 L·min−1) is an effective option to prevent hypoxia or hypercapnia.49,50 For patients with respiratory failure who are undergoing bronchoscopy, the application of non-invasive positive pressure ventilation via resuscitation face mask has been proven superior to HFNO in maintaining adequate oxygenation.51 The Janus mask (Biomedical Srl, Florence, Italy) is another option for these cases as it allows delivery of continuous positive airway pressure while bronchoscopy is performed.52
When deep sedation or general anesthesia is desired and an airway-securing device is required, patients should be pre-oxygenated with a non-rebreathe face mask at 10-12 L·min−1.38 Once sedation or anesthesia has been induced, the airway can be supported using a supraglottic airway (SGA) over a regular endotracheal tube (ETT). A laryngeal mask airway (LMA®; Teleflex Medical Inc; Wayne, PA, USA) is a common option as it allows adequate examination of the larynx and facilitates sampling of high-level (e.g., station 2) mediastinal lymph nodes. Other SGAs have similarly been used.53 Because they produce less stimulation at placement, SGAs require lower doses of sedating agents compared with an ETT and are a relatively non-traumatic method when a tracheal lesion (i.e., mass or stenosis) is present.17,54 An SGA also allows proper evaluation and treatment of subglottic/high-tracheal lesions54,55 and provides airway support, improving oxygen saturation and facilitating insertion of the bronchoscope into the larynx.56,57
As no studies have compared the use of different SGA designs in the context of flexible bronchoscopy, the size and type of the SGA chosen will depend on each patient’s size and product availability. Different alternatives, such as the ProSeal™ (Teleflex Medical Inc; Wayne, PA, USA) or i-gel® SGA (Intersurgical, Wokingham, UK), may be used. An SGA with its own bite block, such as the i-gel, can be used to prevent injury to the patient as well as damage to the bronchoscope. Sizes 4 and 5 are the main options described in the literature for use in the adult population.58 The size 4 i-gel has a 12.3-mm internal diameter and fits a therapeutic bronchoscope (5.9-mm external diameter) or EBUS scope (6.9-mm external diameter) without significantly compromising ventilation.38 This device will also allow the introduction of a 7.0-mm external diameter ETT in case intubation is needed.59 Recent literature suggests that the i-gel SGA is a reliable and safe alternative in patients with severe chronic obstructive pulmonary disease undergoing bronchoscopy procedures in whom excessive tracheal stimulation from laryngoscopy and ETT insertion should be avoided.60
Because the bronchoscope is constantly inserted and withdrawn, the SGA can be dislodged, leading to an air leak.23 Proper ventilation should be assessed with end-tidal capnography, auscultation, and inspection of the mask position using the bronchoscope. In cases of difficult SGA placement, obesity, or severe gastroesophageal reflux, an ETT is a reasonable option. Typically, a larger sized ETT (i.e., 8-9 mm) is recommended, particularly if a wide-diameter therapeutic bronchoscope (5.7-mm external diameter) or an EBUS scope (6.9-mm external diameter) is being used.38
Ventilator settings should be adjusted according to a patient’s physiologic parameters. Pressure-controlled ventilation with a standard continuous positive end-expiratory pressure (PEEP) between 5 and 10 cmH2O as well as positive pressure support ventilation between 15 and 20 cmH2O is a reasonable approach.51,61 Other parameters suggested include a tidal volume close to 10 mL·kg−1 body weight, F i O2 of 100%, a 1:2 inspiratory to expiratory ratio, and a respiratory rate of 12 cycles·min−1. When performing electrosurgical procedures, different settings (including low F i O2) are recommended to prevent airway fire (see common complications and special considerations as discussed further it the text). For endoscopic lung volume reduction procedures (valves or coils), a 1:3 to 1:4 inspiration-to-expiration ratio is recommended to avoid auto-PEEP.62
When using an SGA, a maximum peak pressure of 20-30 cmH2O is preferred to minimize air leaks and gastric distention.63 Patients who despite these measures have unreasonably high end-tidal carbon dioxide (CO2) or persistent low SaO2 should undergo endotracheal intubation with volume-controlled ventilation. When performing balloon dilation, mechanical ventilation is recommended since apnea during the balloon inflation is needed.64
Common complications and special considerations
Flexible bronchoscopy is generally a very safe procedure. In 2003, the ACCP reported a major complication rate of < 1% with a mortality rate of < 0.04% after evaluating nearly 68,000 cases.5 A retrospective study that evaluated over 23,000 procedures in China reported a major complication rate of 0.64% with a mortality rate of 0.013%.65 The most common complications included airway (larynx, trachea, or bronchi) spasm (0.28%), bleeding (0.16%), arrhythmias (0.10%), and pneumothorax/airway perforation (0.03%).5,65,66
Most cases of endobronchial bleeding that occur during bronchoscopy are minimal (estimated < 20 mL) and do not represent a major threat to the patient´s clinical condition.67,68 Massive endobronchial hemorrhage occurs in < 0.1% of cases but may have a fatality rate as high as 10%.69 For these events, conversion to rigid bronchoscopy may be required to protect and selectively ventilate the non-bleeding lung.
Procedures such as EBUS-TBNA carry an extremely low risk of endobronchial bleeding (0.2%), as shown in the over 1,300 cases evaluated by the ACCP Quality Improvement Registry, Evaluation, and Education (AQuIRE) registry.70 Nevertheless, it is important to highlight the close anatomical relation that exists between major vascular structures and mediastinal lymph nodes—i.e., stations in the left lower paratracheal region (4 L, 5, and 6) with the aortic arch and the pulmonary artery; stations in the right lower paratracheal region (4R) with the superior vena cava; and upper paratracheal stations (2R and 2L) with the innominate artery, left common carotid artery, and bilateral innominate veins.71 The use of colour Doppler ultrasound during EBUS procedures allows for proper identification of vascular structures.72
Aspirin use does not increase the bleeding risk during biopsies and should not preclude bronchoscopy from taking place.73 Nevertheless, clopidogrel does significantly increase the risk of hemorrhage and has an additive effect when combined with aspirin. Current recommendations state that clopidogrel should be discontinued seven days prior to bronchoscopic biopsies.66,74
Anticoagulant agents increase the risk of hemorrhage and should not be taken prior to endobronchial biopsies. Low-molecular-weight heparin should be discontinued 12-24 hr before procedure (depending on therapeutic doses), while intravenous heparin should be discontinued four to six hours prior to procedure.16,75 Warfarin also increases bleeding risk and should be discontinued five days ahead of procedure.66 Oral anticoagulants are highly dependent on patient renal function; apixaban and rivaroxaban should be discontinued at least 24-48 hr before procedure, whereas dabigatran should be stopped for 36-72 hr in advance. In patients with impaired renal function (i.e., creatinine clearance 30-50 mL·min−1) apixaban and rivaroxaban should be discontinued 36-72 hr prior to procedure. Because dabigatran has a significantly higher renal elimination, it should be withdrawn 48-96 hr ahead of the procedure in patients with renal impairment.76 Despite recommendations, antiplatelet/anticoagulation regimes should be managed considering each patient’s condition, carefully evaluating the risk-benefit relation for each case.
Pre-procedure coagulation tests (activated partial thromboplastin time, prothrombin time, and international normalized ratio) are poor predictors of bleeding risk and should not be routinely performed.77,78 These should be reserved for cases with known bleeding risk factors, including immunosuppression (HIV), thrombocytopenia, uremia, mechanical ventilation, and history of coagulopathy.79 Platelet counts as low as 20,000-30,000 mm−3 may be sufficient to avoid endobronchial bleeding when doing airway inspection or BAL, but platelet counts above 50,000 mm−3 are recommended for advanced diagnostic or therapeutic bronchoscopy.67,80
Even though most procedures done via flexible bronchoscopy are relatively safe, there is always a risk of airway perforation when dilating a narrowed airway or performing a transbronchial biopsy, for example. This can present as subcutaneous emphysema, pneumothorax, pneumomediastinum, or even air embolism.23 On the other hand, the pneumothorax risk associated with transbronchial biopsies is < 3%.81,82 with a recent meta-analysis reporting a pneumothorax rate of only 1.5% during guided transbronchial biopsies.30 This risk is increased up to 14% in mechanically ventilated patients. Because the risk depends on a variety of factors such as the anatomical location of the biopsies and the technique used, some authors suggest doing a routine chest x-ray 30-60 min after high-risk procedures, particularly if the patient exhibits signs of respiratory distress.83
Cardiovascular comorbidities may represent a challenge when performing bronchoscopy. Invasive airway procedures increase myocardial work load by increasing the heart rate and systolic and diastolic blood pressure as well as decreasing SaO2.84,85 High-risk patients should be fully monitored and receive adequate O2 supplementation. Some authors suggest that patients with an acute coronary event or recent heart failure exacerbation should have their procedure deferred for four to six weeks.16 Nevertheless, if there is an strong need for bronchoscopy, this may be performed safely as long as the patient is not having an active ischemic episode.86 Although the magnetic field generated over the patient during ENB is a potential source of interference over implantable pacemakers and cardioverter defibrillators,87 current evidence suggests that ENB can be safely performed in patients with such devices.88
Lung edema secondary to negative airway pressure is an uncommon complication, but can occur if the patient coughs or inhales against a closed glottis or an obstructed airway (by balloon or bronchoscope). This situation is best prevented by maintaining an adequate anesthetic depth and proper muscle relaxation and generously irrigating the glottis with topical lidocaine.38
Rigid bronchoscopy
Procedure description
Rigid bronchoscopy is an invasive procedure that allows simultaneous ventilation, oxygenation, and airway inspection/intervention. It was first described in the late 1800s by the German physician Gustav Killian as a tool to remove foreign bodies from the tracheobronchial tree.10 Rigid bronchoscopy procedures represent a challenge for the anesthesiologist because it requires allowing the interventionist easy access to the airway, with an adequate degree of muscle paralysis, all the while maintaining proper ventilation and oxygenation.17
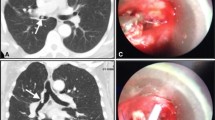
The rigid bronchoscope is composed of a hollow metal tube with a beveled distal end. On the proximal end, the scope’s “head” has three ports: one for an optical device (fibrescope or eyepiece), one for a working instrument, and one for ventilation (lateral port). Lengths usually range from 33 cm (tracheoscope) to 43 cm (bronchoscope), while diameters may be as small as 3 mm and as large as 14 mm. The rigid bronchoscopes have fenestrations on the distal segment that allow lateral ventilation when selective intubation is performed (see Figure).8,89
It is typically used to perform airway procedures that involve bypassing an obstruction or those that require a large working channel. In contrast to the flexible bronchoscope, the rigid bronchoscope offers fewer limitations in terms of the working channel size and field exploration. Endobronchial tumour destruction and removal are commonly performed using rigid bronchoscopy. Other frequently used indications include mechanical dilation (for central airway obstruction) and endobronchial ablation (laser, argon plasma coagulation, electrocautery, and cryodebridement).24,90,91,92
Rigid bronchoscopy is particularly suitable for foreign object removal because it allows securing the airway while facilitating its inspection. This helps prevent accidental object dislodgement into the distal airways.93 Rigid bronchoscopy is also useful for airway stent placement (silicone and metallic) or treating both benign and malignant obstructions, tracheoesophageal fistulae, and tracheobronchomalacia.91 Flexible bronchoscopy through the rigid scope that is used as a conduit frequently complements rigid bronchoscopy because it reaches more distal airways (i.e., the rigid bronchoscope only reaches the mainstem bronchi) facilitating suction and tool guidance.5,8
Anesthetic depth and pharmacologic considerations
Because rigid bronchoscopy is a much more stimulating procedure than flexible bronchoscopy, it almost always requires general anesthesia.94 As with flexible bronchoscopy, the use of volatile anesthetics for induction and maintenance of anesthesia is discouraged. The ventilation methods used and constant airway leaks during rigid bronchoscopy make inhaled anesthetics highly unreliable and can lead to considerable operating room contamination.23,38,95
Premedication with midazolam (2-4 mg iv) helps reduce anxiety and produces anterograde amnesia.96,97 Although it is not a routine practice, some authors suggest premedication with oral clonidine (300 µg) to blunt the cardiovascular response produced by rigid bronchoscope insertion. This protects against potential arrhythmias and myocardial ischemia.98 Spraying topical lidocaine 1% (3-5 mg·kg−1) over the supraglottic and glottic areas is another strategy proposed to blunt the cardiovascular response associated with bronchoscope insertion.99 Anticholinergics, particularly glycopyrrolate, are options because of their antisialagogue properties and reduction in overall airway secretions.48 Premedication with small intramuscular doses of glycopyrrolate (0.005 mg·kg−1) 30 min prior to procedure is commonly seen in clinical practice.100,101 Atropine use is discouraged as it has been associated with greater hemodynamic fluctuations and increased procedure time,48 though available data on this subject are limited.
Anesthesia induction and maintenance are best performed with propofol-based TIVA infusions, titrating doses of 100-200 µg·kg−1·min−1.23,102 Additional 30-50-mg boluses may be used to suppress hemodynamic responses and laryngospasm when changing or re-introducing the rigid scope.64 Propofol is also thought to attenuate some of the postoperative coughing that often occurs.103 Because awareness during anesthesia is a major concern when performing rigid bronchoscopy, some authors suggest that propofol infusions should be guided by bispectral index (BIS) monitoring, with the target between 40 and 60.104,105
In addition to propofol, short-acting opioids (remifentanil) are a safe option and should be used particularly when low levels of postoperative pain are expected.106 Remifentanil bolus (1 µg·kg−1) followed by infusion (0.3 µg·kg−1·min−1) can effectively attenuate the cardiovascular response to bronchoscopy better than fentanyl (2 µg·kg−1).107 Similarly, a remifentanil bolus of 2 µg·kg−1 (in addition to a target-controlled infusion of propofol) attenuates the cardiovascular response during rigid bronchoscopy better than remifentanil at 1 µg·kg−1.108 Recent literature supports the use of higher doses of remifentanil infusions (0.25-0.5 µg·kg−1·min−1) over lower doses, as these are associated with lower risk of coughing and laryngospasm and increased proceduralist satisfaction.109
Other pharmacologic strategies for rigid bronchoscopy including dexmedetomidine and ketamine have been described.64 Dexmedetomidine has been used for foreign object extraction in elderly patients receiving an initial bolus of 1-2 µg·kg−1 followed by a 0.2-0.7 µg·kg−1·hr−1 maintenance infusion.110 In children, dexmedetomidine (4 µg·kg−1 bolus followed by 1-2 µg·kg−1·hr−1 infusion) plus propofol (200 µg·kg−1·min−1) has been described for cases that require spontaneous ventilation.111 The addition of ketamine to remifentanil-based TIVA does not provide an advantage in terms of hemodynamic stability compared with remifentanil and propofol-based TIVA.94
For pediatric patients, the use of volatile anesthetics during induction is accepted, especially in scenarios when spontaneous ventilation is desired (i.e., foreign object removal). For these situations, sevoflurane is used as the induction agent because of its less pungent nature as well as providing better hemodynamic stability, less respiratory depression, and faster induction and recovery times compared with other TIVA alternatives.112 Nevertheless, propofol with remifentanil TIVA (under BIS guidance) is a safe induction alternative for children undergoing rigid bronchoscopy.113 Infusions using propofol (200 µg·kg−1·min−1) and remifentanil (0.05-0.15 µg·kg−1·min−1) have been described for anesthesia maintenance in this population.102
Muscle relaxation is desired during most scenarios to facilitate proper intubation and minimize airway injury. Proposed pharmacologic schemes include depolarizing and non-depolarizing agents. Indeed, short-acting neuromuscular blocking agents (e.g., succinylcholine) are suitable for intubation in cases that require subsequent maintenance of spontaneous ventilation to evaluate dynamic airway obstruction.17,106 Low-dose succinylcholine (0.5 mg·kg−1) is associated with better intubating conditions and lower costs compared with low-dose rocuronium (0.25 mg·kg−1) with sugammadex reversal (0.5 mg·kg−1).114 For cases requiring more prolonged paralysis, additional rocuronium boluses of 0.3 mg·kg−1 may be administered.23 Postoperative myalgia associated with depolarizing agents may be reduced using low precurarization doses of rocuronium (5 mg) or vecuronium (0.5 mg).17
Complete reversal of the neuromuscular blockade at the end of the procedure is fundamental as most patients who undergo rigid bronchoscopy have a significantly decreased pulmonary reserve and do not tolerate residual paralysis.115 An SGA can be placed as a transitory airway to provide partial ventilation support after rigid scope removal.17 The SGA allows inspection of the larynx, which can be facilitated by spraying with lidocaine 1%. This common practice effectively decreases the incidence of laryngospasm.116 In the post-anesthesia care unit, simple maneuvers such as raising the head of the bed and administering high F i O2 with humidified oxygen can reduce coughing and respiratory distress; nebulized lidocaine can also be beneficial.96
Airway and ventilation modes
Different ventilation methods have been historically employed with rigid bronchoscopy. The most common are apneic oxygenation, spontaneous-assisted ventilation, controlled mechanical ventilation, and jet ventilation (manual or automatic, high or low frequency).3 Apneic ventilation was the first approach described for ventilation during rigid bronchoscopy. Patients are pre-oxygenated and ventilated initially with a 100% F i O2. Ventilation is then suspended while the pulmonologist works through the bronchoscope. When the SaO2 threshold has been reached (e.g., 92%), the procedure is paused, bronchoscopy instruments are removed, and the patient is ventilated, usually with a self-inflating bag system and an F i O2 of 100%. Once oxygenation has improved, apnea is reinstituted allowing the procedure to continue.3 In more modern-day practice, apneic ventilation is discouraged, as it can lead to significant acid-base disturbances, blood pressure instability, and a higher probability of awareness episodes during bronchoscopy.103,104
Spontaneous-assisted ventilation is another technique used to support rigid bronchoscopy. It is performed concomitantly with TIVA by titrating the anesthetic dose such that patients maintain spontaneous ventilation. The bronchoscope is connected to the anesthetic circuit and respiratory support is provided as needed. The anesthesiologist will attempt to maintain a respiratory rate between 10 and 20 breaths·min−1, in synchronization with the patient and the bronchoscopist’s maneuvers. Oxygen supplementation using high F i O2 is given constantly through the rigid bronchoscope.117 Spontaneous assisted ventilation was the method performed traditionally for foreign object removal, particularly in children. Nevertheless, a recent meta-analysis concluded that it is associated with a higher incidence of laryngospasm and coughing compared with controlled ventilation.118 Although this meta-analysis suggests that these ventilation modes do not differ in terms of desaturation events, other authors have reported a higher incidence associated with spontaneous ventilation.118,119
Ventilation support for rigid bronchoscopy may be delivered in the form of mechanical positive pressure controlled ventilation. As with spontaneous assisted ventilation, the bronchoscope is connected to the anesthesia circuit, thus serving as an endotracheal tube. Air leaks can be minimized by sealing the bronchoscope ports with caps and packing the nasal and oral pharynx with gauze. This ventilation modality is less often used for rigid bronchoscopy because constant airway leaks interfere with the ventilator’s ability to deliver pre-set gas volumes.3 Similarly, conventional ventilators deliver large tidal volumes that cause constant displacement of diaphragm and thoracic structures, which can complicate the interventional procedure.
Jet ventilation is commonly used during rigid bronchoscopy. Based on the Venturi principle and other physical properties, the system achieves a high F i O2 by administering high-pressure gas through an open system. Jet ventilation is convenient because it provides adequate ventilation and allows proper technical access during rigid bronchoscopy procedures.120,121 It can be delivered manually (i.e., with a Sanders adapter)122 or mechanically, as high frequency jet ventilation (HFJV) (120-600 respirations·min−1) and/or low frequency jet ventilation (LFJV) (10-30 respirations·min−1).89,120 Several hybrid jet ventilation techniques are now available thanks to modern ventilators such as the TwinStream Respirator™ (Carl Reiner, Vienna, Austria). Superimposed high-frequency jet ventilation (SHFJV) is a modality that combines both HFJV and LFJV and is commonly used for patients with laryngotracheal stenosis as it helps avoid excessively high airway pressures.123 Delivered tidal volumes usually range between 1 and 3 mL·kg−1 and may be less than the anatomical dead space, hence the need for very high frequency.89 Technical settings (e.g., driving pressure and duration) of the jet ventilator can be adjusted according to intraoperative blood-gas analysis or based on the quantity of conventional ventilation periods required to achieve adequate SaO2. The end-tidal CO2 after brief periods of HFJV interruption can be used to estimate partial pressure of CO2 along with transcutaneous CO2 monitoring to guide ventilator parameters.124 Although some patients will require an arterial cannula to monitor arterial gases, the adequate use of capnography may reduce unnecessary arterial blood gas sampling.125
Recommendations to prevent barotrauma include maintaining a driving pressure around 1.5 bar (approximately 20 PSI) and limiting inspiration duration to 30-40% of the respiratory cycle.89 Pressure parameters may be adjusted by targeting a maximum PEEP of 10 cmH2O, especially when treating patients with severe central airway obstruction, as high auto-PEEP might develop, causing barotrauma.126 Different airway pressures are displayed in real time by modern mechanical ventilators (e.g., Monsoon High Frequency Jet Ventilator®; Acutronic Medical Systems AG, Hirzel, Switzerland). Importantly, to prevent barotrauma, the expiratory pathway on the rigid bronchoscope must remain unobstructed.89
Following the procedure, the rigid bronchoscope is withdrawn and respiratory support is provided until residual sedation resolves. An SGA, particularly an LMA, is preferred over a face mask for this purpose, as its use favours hemodynamic and respiratory stability.127 In addition, an LMA allows spraying vocal cords with topical anesthetic and a prompt airway inspection with a flexible bronchoscope in case of an emergent situation.91
Common complications and special considerations
Complication rates associated with rigid bronchoscopy vary significantly depending on the patient health status and procedure performed. A recent retrospective study evaluated complication rates in over 3,000 children undergoing foreign body extraction and reported a 9% complication rate. Frequent complications include hypoxemia (3.2%), laryngospasm (1.3%), laryngeal edema (0.9%), atelectasis (0.3%), and pneumothorax (0.3%). The mortality rate was 0.3%128 but other series have reported complication rates as high as 19.8% and a 30-day mortality of 7.8%, particularly when bronchoscopy is performed urgently in patients with severe underlying disease and high American Society of Anesthesiologists (ASA) physical status scores.129
The ACCP recently published complication rates for malignant central airway obstruction based on results from the AQuIRE Registry. Over 1,000 procedures conducted in 947 patients revealed a complication rate of 3.9% with a 14.8% 30-day mortality rate. Variables identified as increased complication rate predictors for therapeutic bronchoscopy (including both rigid and flexible) included: emergent procedures, ASA physical status scores > III, re-do therapeutic bronchoscopy, and the need for moderate sedation.128 Hence, careful patient selection and weighting the risk-benefit relation of the procedure contribute to its success. In patients with a high risk of central airway obstruction, availability of extracorporeal circulation devices or ability to perform emergency tracheotomy is advisable.24
Appropriate ventilation method selection is fundamental, as this may be the source for complications. Spontaneous ventilation is associated with an 18% risk of hypoxemia and a 1% risk of bronchospasm and laryngospasm. These events can be reversed with simple pharmacologic measures without severe consequences.89 Jet ventilation is an option to maintain normocapnic oxygenation, but may cause barotrauma; cases of pneumothorax, pneumomediastinum, subcutaneous emphysema, and even tension pneumothorax have been described.121,130 Since this is a high-pressure open system with no expiration valve, the air outlet should not be obstructed to prevent excessive airway pressure buildup. For this purpose, some automated jet ventilators have built-in alarm systems.17,55
Other devices, such as the Ventrain® system (Ventinova Medical B.V., Eindhovven, Netherlands), have an active expiration mechanism that facilitates ventilation through a small-bore cricothyroidotomy cannula and may be useful in acute upper airway obstruction scenarios.131,132 Although this technique is not currently used to support interventional pulmonary procedures, it may be considered as an alternative to ventilate patients under cannot-ventilate-cannot-oxygenate scenarios. Two recently published case reports describe its elective use in patients with severe upper airway obstruction undergoing endoscopic debridement of supraglottic lesions.132,133
Jet ventilation in proximity to stenotic lesions may significantly increase the pressure in airways distal to the lesion.134 Excessive pressure buildup can be prevented by placing the jet injector as far as possible from the lesion or by placing a jet ventilation catheter either on the mainstem bronchus contralateral to the lesion (while selectively intubated with a rigid bronchoscope) or distal to the lesion treated.134 Other complications involving jet ventilation include injury to the mucociliary epithelium (due to extremely high respiratory frequency) and are best prevented by ventilators that allow air humidification and warming.17,55 Patients with pneumonia, an acute asthma attack, severe obesity, or poor baseline oxygenation are poor candidates for jet ventilation because this may lead to severe heterogeneity in ventilation.90
Different risks are associated with specific surgical techniques. Airway fire is a rare but catastrophic event, caused by the combination of an ignitor (a heat-based surgical device such as a laser or electrocautery), an oxidizer (oxygen or nitrous oxide), and fuel (tissue, mesh, or plastic devices).135 Hence, the main approach to prevent these events is to reduce the use of each of the three elements described previously. In that sense, it is recommended that F i O2 and end-tidal O2 be below 40% prior to activation of the laser, electrocautery, or argon plasma coagulation (APC) systems.136 Patients who cannot tolerate F i O2 < 40% should not undergo these procedures and a different therapeutic alternative should be considered.
Other safety measures that have been described include correcting air leaks, avoiding nitrous oxide, and using a shorter circuit with high fresh gas flow (i.e., > 5 L·min−1) that allows for the more rapid achievement of low F i O2 concentrations.136,137 To decrease exposure to potential fuels, a distance > 1 cm between the tip of the probe (laser, electrocautery, or APC) and the tip of the bronchoscope and a distance > 4 cm between the tip of the probe and the tip of the distal end of the ETT should be maintained. Similarly, gauzes sponges, mesh, drapes, or any other products used to pack the oropharynx should not be used as these may act as combustible material.135
Spray cryotherapy, used to recanalize the airway in benign and malignant conditions, may lead to tension pneumothorax, pneumothorax, or severe hypoxia due to rapid conversion of nitrous oxide from the liquid to gaseous form. Complications in this scenario are best prevented by generous preoxygenation, holding ventilation, and allowing free airway outflow.138 The use of APC has a low yet life-threatening risk of argon gas embolism. Unfortunately, other than using a low flow of argon gas and avoiding direct contact with vessels, there are no other effective measures to prevent these events.139 Although the risk of airway fire with APC is low (at least in theory) because argon gas displaces oxygen and thus reduces the combustion risk, the F i O2 should nonetheless still be kept < 40%.93 Rigid bronchoscope insertion may cause a rise in intracranial pressure secondary to laryngeal stimulation; however, this effect is not clinically significant.140
Lastly, in patients who present with critical airway stenosis, positive pressure ventilation above the stenosis might not achieve adequate ventilation once the patient is under general anesthesia.141 Balloon dilation using topical anesthesia and minimal sedation can be achieved in spontaneously breathing awake patients.142 Such a technique can allow a safer tracheal luminal diameter to proceed with more conventional anesthesia and therapeutic intervention. Furthermore, in patients requiring stent placement, silicone (but not metallic) stents require the use of the rigid bronchoscope. In patients requiring further ventilatory support following tracheal stent placement, proper placement of an appropriately sized ETT directed visually under bronchoscopic guidance is necessary to avoid airway stent dislodgement.143 Thus, coordination between the anesthesia team and interventional pulmonologist is required.
Conclusions
Interventional pulmonology is a rapidly growing area of medicine. Advanced diagnostic and therapeutic bronchoscopy is widely applied in different pathologies of the airways, lungs, and mediastinum. Therefore, it is fundamental for the anesthesia provider to be updated on this area.
Evidence-based recommendations regarding airway management, pharmacologic strategies, and complications should help guide anesthesiologists when approaching common bronchoscopic procedures. In daily practice, each case should be approached individually. A thorough evaluation of individual comorbidities, risk factors, and technical aspects associated with each procedure is necessary. Given that interventional pulmonologists and the anesthesia team share the working field, constant communication between specialists is fundamental.
References
Arias S, Lee HJ. The future of interventional pulmonology. Semin Respir Crit Care Med 2014; 35: 763-8.
Beaudoin EL, Chee A, Stather DR. Interventional pulmonology: an update for internal medicine physicians. Minerva Med 2014; 105: 197-209.
Pathak V, Welsby I, Mahmood K, Wahidi M, MacIntyre N, Shofer S. Ventilation and anesthetic approaches for rigid bronchoscopy. Ann Am Thorac Soc 2014; 11: 628-34.
José RJ, Shaefi S, Navani N. Sedation for flexible bronchoscopy: current and emerging evidence. Eur Respir Rev Off J Eur Respir Soc 2013; 22: 106-16.
Ernst A, Silvestri GA, Johnstone D, American College of Chest Physicians. Interventional pulmonary procedures: guidelines from the American College of Chest Physicians. Chest 2003; 123: 1693-717.
Maldonado F, Edell ES, Barron PJ, Yung RC. Update in interventional pulmonology: a prologue to a new review series. Respirol Carlton Vic 2014; 19: 471.
Bolliger CT, Mathur PN, Beamis JF, et al. ERS/ATS statement on interventional pulmonology. European Respiratory Society/American Thoracic Society. Eur Respir J 2002; 19: 356-73.
Alraiyes AH, Machuzak MS. Rigid bronchoscopy. Semin Respir Crit Care Med 2014; 35: 671-80.
Ikeda S, Yanai N, Ishikawa S. Flexible bronchofiberscope. Keio J Med 1968; 17: 1-16.
Panchabhai TS, Mehta AC. Historical perspectives of bronchoscopy. Connecting the dots. Ann Am Thorac Soc 2015; 12: 631-41.
Haas AR, Vachani A, Sterman DH. Advances in diagnostic bronchoscopy. Am J Respir Crit Care Med 2010; 182: 589-97.
Parmaksız ET, Caglayan B, Salepci B, et al. The utility of endobronchial ultrasound-guided transbronchial needle aspiration in mediastinal or hilar lymph node evaluation in extrathoracic malignancy: Benign or malignant? Ann Thorac Med 2012; 7: 210-4.
Navani N, Nankivell M, Lawrence DR, et al. Lung cancer diagnosis and staging with endobronchial ultrasound-guided transbronchial needle aspiration compared with conventional approaches: an open-label, pragmatic, randomised controlled trial. Lancet Respir Med 2015; 3: 282-9.
Chrissian A, Misselhorn D, Chen A. Endobronchial-ultrasound guided miniforceps biopsy of mediastinal and hilar lesions. Ann Thorac Surg 2011; 92: 284-8.
Herth FJF, Schuler H, Gompelmann D, et al. Endobronchial ultrasound-guided lymph node biopsy with transbronchial needle forceps: a pilot study. Eur Respir J 2012; 39: 373-7.
Casal RF, Ost DE, Eapen GA. Flexible bronchoscopy. Clin Chest Med 2013; 34: 341-52.
José RJ, Shaefi S, Navani N. Anesthesia for bronchoscopy. Curr Opin Anaesthesiol 2014; 27: 453-7.
Goyal R, Nayar S, Gogia P, Garg M. Extraction of tracheobronchial foreign bodies in children and adults with rigid and flexible bronchoscopy. J Bronchol Interv Pulmonol 2012; 19):35-43.
Menon PR, Lodha R, Singh U, Kabra SK. A prospective assessment of the role of bronchoscopy and bronchoalveolar lavage in evaluation of children with pulmonary tuberculosis. J Trop Pediatr 2011; 57: 363-7.
Castro M, Rubin AS, Laviolette M, et al. Effectiveness and safety of bronchial thermoplasty in the treatment of severe asthma: a multicenter, randomized, double-blind, sham-controlled clinical trial. Am J Respir Crit Care Med 2010; 181: 116-24.
Sciurba FC, Ernst A, Herth FJ, et al. A randomized study of endobronchial valves for advanced emphysema. N Engl J Med 2010; 363: 1233-44.
Cortese DA, Edell ES, Kinsey JH. Photodynamic therapy for early stage squamous cell carcinoma of the lung. Mayo Clin Proc 1997; 72: 595-602.
Pawlowski J. Anesthetic considerations for interventional pulmonary procedures. Curr Opin Anaesthesiol 2013; 26: 6-12.
Selzer AR, Murrell M, Shostak E. New trends in interventional pulmonology. Curr Opin Anaesthesiol 2017; 30: 17-22.
Silvestri GA, Gonzalez AV, Jantz MA, et al. Methods for staging non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013; 143(5 Suppl): e211S-50S.
Ozgul G, Cetinkaya E, Ozgul MA, et al. Efficacy and safety of electromagnetic navigation bronchoscopy with or without radial endobronchial ultrasound for peripheral lung lesions. Endosc Ultrasound 2016; 5: 189-95.
Ali MS, Trick W, Mba BI, Mohananey D, Sethi J, Musani AI. Radial endobronchial ultrasound for the diagnosis of peripheral pulmonary lesions: a systematic review and meta-analysis. Respirol Carlton Vic 2017; 22: 443-53.
Vincent BD, El-Bayoumi E, Hoffman B, et al. Real-time endobronchial ultrasound-guided transbronchial lymph node aspiration. Ann Thorac Surg 2008; 85: 224-30.
Muñoz-Largacha JA, Litle VR, Fernando HC. Navigation bronchoscopy for diagnosis and small nodule location. J Thorac Dis 2017; 9(Suppl 2): S98-103.
Wang Memoli JS, Nietert PJ, Silvestri GA. Meta-analysis of guided bronchoscopy for the evaluation of the pulmonary nodule. Chest 2012; 142: 385-93.
Dhillon SS, Harris K. Bronchoscopy for the diagnosis of peripheral lung lesions. J Thorac Dis 2017; 9(Suppl 10): S1047-58.
Continuum of Depth of Sedation: Definition of General Anesthesia and Levels of Sedation/Analgesia. Available from URL: http://www.asahq.org/~/media/Sites/ASAHQ/Files/Public/Resources/standardsguidelines/continuum-of-depth-of-sedation-definition-of-general-anesthesia-and-levels-of-sedationanalgesia.pdf (accessed January 2018).
Stolz D, Chhajed PN, Leuppi JD, Brutsche M, Pflimlin E, Tamm M. Cough suppression during flexible bronchoscopy using combined sedation with midazolam and hydrocodone: a randomised, double blind, placebo controlled trial. Thorax 2004; 599: 773-6.
Gaisl T, Bratton DJ, Heuss LT, et al. Sedation during bronchoscopy: data from a nationwide sedation and monitoring survey. BMC Pulm Med 2016; 16: 113.
Müller T, Thümmel K, Cornelissen CG, Krüger S, Dreher M. Analogosedation during flexible bronchoscopy using a combination of midazolam, propofol and fentanyl - a retrospective analysis. PloS One 2017; 12: e0175394.
Yoon HI, Kim JH, Lee JH, et al. Comparison of propofol and the combination of propofol and alfentanil during bronchoscopy: a randomized study. Acta Anaesthesiol Scand 2011; 55: 104-9.
Schlatter L, Pflimlin E, Fehrke B, Meyer A, Tamm M, Stolz D. Propofol versus propofol plus hydrocodone for flexible bronchoscopy: a randomised study. Eur Respir J 2011; 38: 529-37.
Sarkiss M, Kennedy M, Riedel B, et al. Anesthesia technique for endobronchial ultrasound-guided fine needle aspiration of mediastinal lymph node. J Cardiothorac Vasc Anesth 2007; 21: 892-6.
Clark G, Licker M, Younossian AB, et al. Titrated sedation with propofol or midazolam for flexible bronchoscopy: a randomised trial. Eur Respir J 2009; 34: 1277-83.
Hwang J, Jeon Y, Park HP, Lim YJ, Oh YS. Comparison of alfetanil and ketamine in combination with propofol for patient-controlled sedation during fiberoptic bronchoscopy. Acta Anaesthesiol Scand 2005; 49: 1334-8.
Fruchter O, Manevich Y, Carmi U, Rozengarten D, Kramer MR. Prospective Randomized Trial Evaluating Ketamine for Adult Bronchoscopy. J Bronchol Interv Pulmonol 2017; 24: 279-84.
Wahidi MM, Jain P, Jantz M, et al. American College of Chest Physicians consensus statement on the use of topical anesthesia, analgesia, and sedation during flexible bronchoscopy in adult patients. Chest 2011; 140: 1342-50.
Majid A, Gaurav K, Sanchez JM, et al. Evaluation of tracheobronchomalacia by dynamic flexible bronchoscopy. A pilot study. Ann Am Thorac Soc 2014; 11: 951-5.
Kaur H, Dhooria S, Aggarwal AN, Gupta D, Behera D, Agarwal R. A randomized trial of 1% vs 2% lignocaine by the spray-as-you-go technique for topical anesthesia during flexible bronchoscopy. Chest 2015; 148: 739-45.
Casal RF, Lazarus DR, Kuhl K, et al. Randomized trial of endobronchial ultrasound-guided transbronchial needle aspiration under general anesthesia versus moderate sedation. Am J Respir Crit Care Med 2015; 191: 796-803.
Yarmus LB, Akulian JA, Gilbert C, et al. Comparison of moderate versus deep sedation for endobronchial ultrasound transbronchial needle aspiration. Ann Am Thorac Soc 2013; 10: 121-6.
Aswanetmanee P, Limsuwat C, Kabach M, Alraiyes AH, Kheir F. The role of sedation in endobronchial ultrasound-guided transbronchial needle aspiration: systematic review. Endosc Ultrasound 2016; 5: 300-6.
Malik JA, Gupta D, Agarwal AN, Jindal SK. Anticholinergic premedication for flexible bronchoscopy: a randomized, double-blind, placebo-controlled study of atropine and glycopyrrolate. Chest 2009; 136: 347-54.
Booth AW, Vidhani K, Lee PK, Thomsett CM. SponTaneous Respiration using IntraVEnous anaesthesia and Hi-flow nasal oxygen (STRIVE Hi) maintains oxygenation and airway patency during management of the obstructed airway: an observational study. BJA Br J Anaesth 2017; 118: 444-51.
Drake MG. High flow nasal cannula oxygen in adults: an evidence-based assessment. Ann Am Thorac Soc 2017 ==;
Simon M, Braune S, Frings D, Wiontzek AK, Klose H, Kluge S. High-flow nasal cannula oxygen versus non-invasive ventilation in patients with acute hypoxaemic respiratory failure undergoing flexible bronchoscopy–a prospective randomised trial. Crit Care Lond Engl 2014; 18: 712.
Cabrini L, Landoni G. A novel non-invasive ventilation mask to prevent and manage respiratory failure during fiberoptic bronchoscopy, gastroscopy and transesophageal echocardiography. Heart Lung Vessels 2015; 7: 297-303.
Sastre JA, Cordovilla R, Jiménez MF, López T. Management of a transbronchial cryobiopsy using the i-gel® airway and the Arndt endobronchial blocker. Can J Anesth 2014; 61: 886-8.
Vorasubin N, Vira D, Jamal N, Chhetri DK. Airway management and endoscopic treatment of subglottic and tracheal stenosis: the laryngeal mask airway technique. Ann Otol Rhinol Laryngol 2014; 123: 293-8.
Sarkiss M. Anesthesia for bronchoscopy and interventional pulmonology: from moderate sedation to jet ventilation. Curr Opin Pulm Med 2011; 17: 274-8.
Alon D, Pertzov B, Gershman E, et al. The Safety of laryngeal mask airway-assisted bronchoscopy versus standard nasal bronchoscopy. Respir Int Rev Thorac Dis 2017; 93: 279-84.
Fadaizadeh L, Hoseini MS, Bagheri M. Anaesthesia management during interventional bronchoscopic procedures: laryngeal mask airway or rigid bronchoscope. Turk J Anaesthesiol Reanim 2014; 42: 302-7.
Landsdalen HE, Berge M, Kristensen F, Guttormsen AB, Søfteland E. Continuous ventilation during intubation through a supraglottic airway device guided by fiberoptic bronchoscopy: a observational assessment. Acta Anaesthesiol Scand 2017; 61: 23-30.
Sharma S, Rogers R, Popat M. The i-gel™ airway for ventilation and rescue intubation. Anaesthesia 2007; 62: 419-20.
Arevalo-Ludeña J, Arcas-Bellas JJ, Alvarez-Rementería R, Flandes J, Morís L, Muñoz Alameda LE. A comparison of the I-Gel supraglottic device with endotracheal intubation for bronchoscopic lung volume reduction coil treatment. J Clin Anesth 2016; 31: 137-41.
Murgu SD, Pecson J, Colt HG. Flexible bronchoscopy assisted by noninvasive positive pressure ventilation. Crit Care Nurse 2011; 31: 70-6.
Slebos D-J, Shah PL, Herth FJF, Valipour A. Endobronchial valves for endoscopic lung volume reduction: best practice recommendations from expert panel on endoscopic lung volume reduction. Respir Int Rev Thorac Dis 2017; 93: 138-50.
Aoyama K, Yasunaga E, Takenaka I, Kadoya T, Sata T, Shigematsu A. Positive pressure ventilation during fibreoptic intubation: comparison of the laryngeal mask airway, intubating laryngeal mask and endoscopy mask techniques. Br J Anaesth 2002; 88: 246-54.
Goudra BG, Singh PM, Borle A, Farid N, Harris K. Anesthesia for advanced bronchoscopic procedures: state-of-the-art review. Lung 2015; 193: 453-65.
Jin F, Mu D, Chu D, Fu E, Xie Y, Liu T. Severe complications of bronchoscopy. Respir Int Rev Thorac Dis 2008; 76: 429-33.
Du Rand IA, Blaikley J, Booton R, et al. British Thoracic Society guideline for diagnostic flexible bronchoscopy in adults: accredited by NICE. Thorax 2013; 68(Suppl 1): i1-44.
Carr IM, Koegelenberg CF, von Groote-Bidlingmaier F, et al. Blood loss during flexible bronchoscopy: a prospective observational study. Respir Int Rev Thorac Dis 2012; 84: 312-8.
Cordasco EM, Mehta AC, Ahmad M. Bronchoscopically induced bleeding. A summary of nine years’ Cleveland clinic experience and review of the literature. Chest 1991; 100: 1141-7.
Zhou GW, Zhang W, Dong YC, et al. Flexible bronchoscopy-induced massive bleeding: a 12-year multicentre retrospective cohort study. Respirol Carlton Vic 2016; 21: 927-31.
Ost DE, Ernst A, Grosu HB, et al. Complications following therapeutic bronchoscopy for malignant central airway obstruction: results of the AQuIRE Registry. Chest 2015; 148: 450-71.
Arias S, Liu QH, Frimpong B, et al. Role of the endobronchial landmarks guiding TBNA and EBUS-TBNA in lung cancer staging. Can Respir J 2016; 2016: 1652178.
Yasufuku K, Chiyo M, Sekine Y, et al. Real-time endobronchial ultrasound-guided transbronchial needle aspiration of mediastinal and hilar lymph nodes. Chest 2004; 126: 122-8.
Herth FJ, Becker HD, Ernst A. Aspirin does not increase bleeding complications after transbronchial biopsy. Chest 2002; 122: 1461-4.
Ernst A, Eberhardt R, Wahidi M, Becker HD, Herth FJ. Effect of routine clopidogrel use on bleeding complications after transbronchial biopsy in humans. Chest 2006; 129: 734-7.
Wahidi MM, Rocha AT, Hollingsworth JW, Govert JA, Feller-Kopman D, Ernst A. Contraindications and safety of transbronchial lung biopsy via flexible bronchoscopy. A survey of pulmonologists and review of the literature. Respir Int Rev Thorac Dis 2005; 72: 285-95.
Fenger-Eriksen C, Münster AM, Grove EL. New oral anticoagulants: clinical indications, monitoring and treatment of acute bleeding complications. Acta Anaesthesiol Scand 2014; 58: 651-9.
Segal JB, Dzik WH; Transfusion Medicine/Hemostasis Clinical Trials Network. Paucity of studies to support that abnormal coagulation test results predict bleeding in the setting of invasive procedures: an evidence-based review. Transfusion (Paris) 2005; 45: 1413-25.
Brickey DA, Lawlor DP. Transbronchial biopsy in the presence of profound elevation of the international normalized ratio. Chest 1999; 115: 1667-71.
Kozak EA, Brath LK. Do “screening” coagulation tests predict bleeding in patients undergoing fiberoptic bronchoscopy with biopsy? Chest 1994; 106: 703-5.
Nandagopal L, Veeraputhiran M, Jain T, Soubani AO, Schiffer CA. Bronchoscopy can be done safely in patients with thrombocytopenia. Transfusion (Paris) 2016; 56: 344-8.
Harzheim D, Sterman D, Shah PL, Eberhardt R, Herth FJ. Bronchoscopic transparenchymal nodule access: feasibility and safety in an endoscopic unit. Respir Int Rev Thorac Dis 2016; 91: 302-6.
Durakovic A, Andersen H, Christiansen A, Hammen I. Retrospective analysis of radial EBUS outcome for the diagnosis of peripheral pulmonary lesion: sensitivity and complications. Eur Clin Respir J 2015; 2: 28947.
Boskovic T, Stojanovic M, Stanic J, et al. Pneumothorax after transbronchial needle biopsy. J Thorac Dis 2014; 6(Suppl 4): S427-34.
Ali AH, Toba H, Sakiyama S, et al. Holter ECG monitoring of sympathovagal fluctuation during bronchoscopy. Clin Respir J 2016; 10: 204-10.
Davies L, Mister R, Spence DP, Calverley PM, Earis JE, Pearson MG. Cardiovascular consequences of fibreoptic bronchoscopy. Eur Respir J 1997; 10: 695-8.
Dweik RA, Mehta AC, Meeker DP, Arroliga AC. Analysis of the safety of bronchoscopy after recent acute myocardial infarction. Chest 1996; 110: 825-8.
American Society of Anesthesiologists. Practice advisory for the perioperative management of patients with cardiac implantable electronic devices: pacemakers and implantable cardioverter-defibrillators: an updated report by the american society of anesthesiologists task force on perioperative management of patients with cardiac implantable electronic devices. Anesthesiology 2011; 114: 247-61.
Khan AY, Berkowitz D, Krimsky WS, Hogarth DK, Parks C, Bechara R. Safety of pacemakers and defibrillators in electromagnetic navigation bronchoscopy. Chest 2013; 143: 75-81.
Putz L, Mayné A, Dincq AS. Jet Ventilation during rigid bronchoscopy in adults: a focused review. BioMed Res Int 2016; 2016: 4234861.
Jeon K, Kim H, Yu CM, et al. Rigid bronchoscopic intervention in patients with respiratory failure caused by malignant central airway obstruction. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer 2006; 1: 319-23.
Dincq AS, Gourdin M, Collard E, et al. Anesthesia for adult rigid bronchoscopy. Acta Anaesthesiol Belg 2014; 65: 95-103.
Freitag L, Darwiche K. Endoscopic treatment of tracheal stenosis. Thorac Surg Clin 2014; 24: 27-40.
Farrell PT. Rigid bronchoscopy for foreign body removal: anaesthesia and ventilation. Paediatr Anaesth 2004; 14: 84-9.
Bakan M, Topuz U, Umutoglu T, et al. Remifentanil-based total intravenous anesthesia for pediatric rigid bronchoscopy: comparison of adjuvant propofol and ketamine. Clin Sao Paulo Braz 2014; 69: 372-7.
Purugganan RV. Intravenous anesthesia for thoracic procedures. Curr Opin Anaesthesiol 2008; 21: 1-7.
Conacher ID. Anaesthesia and tracheobronchial stenting for central airway obstruction in adults. Br J Anaesth 2003; 90: 367-74.
Conway A, Rolley J, Sutherland JR. Midazolam for sedation before procedures. Cochrane Database Syst Rev 2016; 5: CD009491.
Matot I, Sichel JY, Yofe V, Gozal Y. The effect of clonidine premedication on hemodynamic responses to microlaryngoscopy and rigid bronchoscopy. Anesth Analg 2000; 91: 828-33.
Gaumann DM, Tassonyi E, Fathi F, Griessen M. Effects of topical laryngeal lidocaine on sympathetic response to rigid panendoscopy under general anesthesia. ORL J Oto-Rhino-Laryngol Its Relat Spec 1992; 54: 49-53.
Grønnebech H, Johansson G, Smedebøl M, Valentin N. Glycopyrrolate vs. atropine during anaesthesia for laryngoscopy and bronchoscopy. Acta Anaesthesiol Scand 1993; 37: 454-7.
Cowl CT, Prakash UB, Kruger BR. The role of anticholinergics in bronchoscopy. A randomized clinical trial. Chest 2000; 118: 188-92.
Shen X, Hu CB, Ye M, Chen YZ. Propofol-remifentanil intravenous anesthesia and spontaneous ventilation for airway foreign body removal in children with preoperative respiratory impairment. Paediatr Anaesth 2012; 22: 1166-70.
Hohlrieder M, Tiefenthaler W, Klaus H, et al. Effect of total intravenous anaesthesia and balanced anaesthesia on the frequency of coughing during emergence from the anaesthesia. Br J Anaesth 2007; 99: 587-91.
Bould MD, Mahtani DG, Davies R, Roughton M, Hunter DN, Kelleher A. Bispectral index values during elective rigid bronchoscopy: a prospective observational pilot study. Anaesthesia 2007; 62: 438-45.
Myles PS, Leslie K, McNeil J, Forbes A, Chan MT. Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial. Lancet Lond Engl 2004; 363: 1757-63.
Brodsky JB. Anesthetic considerations for bronchoscopic procedures in patients with central-airway obstruction. J Bronchol Interv Pulmonol 2001; 8: 36-43.
Prakash N, McLeod T, Gao Smith F. The effects of remifentanil on haemodynamic stability during rigid bronchoscopy. Anaesthesia 2001; 56: 576-80.
Agnew NM, Tan NH, Scawn ND, Pennefather SH, Russell GN. Choice of opioid supplementation for day-case rigid bronchoscopy:a randomized placebo-controlled comparison of a bolus of remifentanil and alfentanil. J Cardiothorac Vasc Anesth 2003; 17: 336-40.
Goudra BG, Singh PM, Manjunath AK, et al. Effectiveness of high dose remifentanil in preventing coughing and laryngospasm in non-paralyzed patients for advanced bronchoscopic procedures. Ann Thorac Med 2014; 9: 23-8.
Chen K, Shen X. Dexmedetomidine and propofol total intravenous anesthesia for airway foreign body removal. Ir J Med Sci 2014; 183: 481-4.
Chen KZ, Ye M, Hu CB, Shen X. Dexmedetomidine vs remifentanil intravenous anaesthesia and spontaneous ventilation for airway foreign body removal in children. Br J Anaesth 2014; 112: 892-7.
Liao R, Li JY, Liu GY. Comparison of sevoflurane volatile induction/maintenance anaesthesia and propofol-remifentanil total intravenous anaesthesia for rigid bronchoscopy under spontaneous breathing for tracheal/bronchial foreign body removal in children. Eur J Anaesthesiol 2010; 27: 930-4.
Malherbe S, Whyte S, Singh P, Amari E, King A, Ansermino JM. Total intravenous anesthesia and spontaneous respiration for airway endoscopy in children–a prospective evaluation. Paediatr Anaesth 2010; 20: 434-8.
Ghezel-Ahmadi V, Ghezel-Ahmadi D, Mangen J, et al. Comparing Patient satisfaction and intubating conditions using succinylcholine or low-dose rocuronium for rigid bronchoscopy: a randomized study. Thorac Cardiovasc Surg 2015; 63: 526-32.
Murphy GS, Brull SJ. Residual neuromuscular block: lessons unlearned. Part I: definitions, incidence, and adverse physiologic effects of residual neuromuscular block. Anesth Analg 2010; 111: 120-8.
Mihara T, Uchimoto K, Morita S, Goto T. The efficacy of lidocaine to prevent laryngospasm in children: a systematic review and meta-analysis. Anaesthesia 2014; 69: 1388-96.
Ayers ML, Beamis JF. Rigid bronchoscopy in the twenty-first century. Clin Chest Med 2001; 22: 355-64.
Liu Y, Chen L, Li S. Controlled ventilation or spontaneous respiration in anesthesia for tracheobronchial foreign body removal: a meta-analysis. Paediatr Anaesth 2014; 24: 1023-30.
Li S, Liu Y, Tan F, Chen J, Chen L. Efficacy of manual jet ventilation using Manujet III for bronchoscopic airway foreign body removal in children. Int J Pediatr Otorhinolaryngol 2010; 74: 1401-4.
Evans E, Biro P, Bedforth N. Jet ventilation. Contin Educ Anaesth Crit Care Pain 2007; 7: 2-5.
Slutsky AS, Drazen JM. Ventilation with small tidal volumes. N Engl J Med 2002; 347: 630-1.
Bradley JL, Moyes EN, Parke FW. Modifications of Sanders’ technique of ventilation during bronchoscopy. Thorax 1971; 26: 112-4.
Rezaie-Majd A, Bigenzahn W, Denk DM, et al. Superimposed high-frequency jet ventilation (SHFJV) for endoscopic laryngotracheal surgery in more than 1500 patients. Br J Anaesth 2006; 96: 650-9.
Simon M, Gottschall R, Gugel M, Fritz H, Mohr S, Klein U. Comparison of transcutaneous and endtidal CO2-monitoring for rigid bronchoscopy during high-frequency jet ventilation. Acta Anaesthesiol Scand 2003; 47: 861-7.
Frietsch T, Krafft P, Becker HD, Buelzebruck H, Wiedemann K. Intermittent capnography during high-frequency jet ventilation for prolonged rigid bronchoscopy. Acta Anaesthesiol Scand 2000; 44: 391-7.
Jiang Y, Kacmarek RM. Efficacy of superimposed high-frequency jet ventilation applied to variable degrees of tracheal stenosis: one step forward to optimized patient care. Anesthesiology 2015; 123: 747-9.
Nisi F, Galzerano A, Cicchitto G, Puma F, Peduto VA. Improving patient safety after rigid bronchoscopy in adults: laryngeal mask airway versus face mask - a pilot study. Med Devices Auckl NZ 2015; 8: 201-6.
Ost DE, Ernst A, Grosu HB, et al. Complications following therapeutic bronchoscopy for malignant central airway obstruction: results of the AQuIRE Registry. Chest 2015; 148: 450-71.
Ernst A, Simoff M, Ost D, Goldman Y, Herth FJ. Prospective risk-adjusted morbidity and mortality outcome analysis after therapeutic bronchoscopic procedures: results of a multi-institutional outcomes database. Chest 2008; 134: 514-9.
Gambrill VL. Diagnosis and treatment of tension pneumothorax under anesthesia: a case report. AANA J 2002; 70: 21-4.
Wahlen BM, Al-Thani H, El-Menyar A. Ventrain: from theory to practice. Bridging until re-tracheostomy. BMJ Case Rep 2017; 2017.
Borg PA, Hamaekers AEW, Lacko M, Jansen J, Enk D. Ventrain® for ventilation of the lungs. Br J Anaesth 2012; 109: 833-4.
Fearnley RA, Badiger S, Oakley RJ, Ahmad I. Elective use of the Ventrain for upper airway obstruction during high-frequency jet ventilation. J Clin Anesth 2016; 33: 233-5.
Ihra GC, Heid A, Pernerstorfer T. Airway stenosis-related increase of pulmonary pressure during high-frequency jet ventilation depends on injector’s position. Anesth Analg 2009; 109: 461-5.
Smith LP, Roy S. Operating room fires in otolaryngology: risk factors and prevention. Am J Otolaryngol 2011; 32: 109-14.
Remz M, Luria I, Gravenstein M, et al. Prevention of airway fires: do not overlook the expired oxygen concentration. Anesth Analg 2013; 117: 1172-6.
Akhtar N, Ansar F, Baig MS, Abbas A. Airway fires during surgery: management and prevention. J Anaesthesiol Clin Pharmacol 2016; 32: 109-11.
Moore RF, Lile DJ, Abbas AE. Current status of spray cryotherapy for airway disease. J Thorac Dis 2017; 9(Suppl 2): S122-9.
Reddy C, Majid A, Michaud G, et al. Gas embolism following bronchoscopic argon plasma coagulation: a case series. Chest 2008; 134: 1066-9.
Grosu HB, Morice RC, Sarkiss M, et al. Safety of flexible bronchoscopy, rigid bronchoscopy, and endobronchial ultrasound-guided transbronchial needle aspiration in patients with malignant space-occupying brain lesions. Chest 2015; 147: 1621-8.
Espinoza A, Neumann K, Halvorsen PS, Sundset A, Kongerud J, Fosse E. Critical airway obstruction: challenges in airway management and ventilation during therapeutic bronchoscopy. J Bronchol Interv Pulmonol 2015; 22: 41-7.
Perrin G, Colt HG, Martin C, Mak MA, Dumon JF, Gouin F. Safety of interventional rigid bronchoscopy using intravenous anesthesia and spontaneous assisted ventilation. A prospective study. Chest 1992; 102: 1526-30.
Tazi-Mezalek R, Musani AI, Laroumagne S, et al. Airway stenting in the management of iatrogenic tracheal injuries: 10-Year experience. Respirol Carlton Vic 2016; 21: 1452-8.
Conflicts of interest
Adnan Majid: Paid consultant for PneumRx, Inc., paid consultant for Olympus Corporations of the Americas, paid consultant for Broncus Medical Inc., and paid consultant for Boston Scientific Corp.
Editorial responsibility
This submission was handled by Dr. Hilary P. Grocott, Editor-in-Chief, Canadian Journal of Anesthesia.
Author contributions
Andrés de Lima, Fayez Kheir, Adnan Majid, and John Pawlowski contributed substantially to all aspects of this manuscript, including conception and design; acquisition, analysis, and interpretation of data; and drafting the article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Lima, A., Kheir, F., Majid, A. et al. Anesthesia for interventional pulmonology procedures: a review of advanced diagnostic and therapeutic bronchoscopy. Can J Anesth/J Can Anesth 65, 822–836 (2018). https://doi.org/10.1007/s12630-018-1121-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-018-1121-3