Abstract
The advent of transcatheter aortic valve replacement (TAVR) has dramatically transformed the clinical approach to severe aortic stenosis. Over the last decade, several trials have shown the equivalence or even superiority of transcatheter valve replacement over the conventional surgical approach. As a result, TAVR as a treatment for severe, symptomatic aortic stenosis has rapidly extended from inoperable or prohibited-risk patients to intermediate-risk patients. The success of TAVR has led to the wide adaptation of this technique and, subsequently, a significant increase in the number of these procedures performed annually. As the number of these procedures is expected to further increase, especially if its indication will include those with low surgical risk, there is a great demand to improve patient recovery and early discharge without compromising outcomes. In this review, we will discuss the role of echocardiography in the perioperative planning and assessment of transcatheter aortic valve replacement. In addition, we will review the current evidence behind the use of intraprocedureal transthoracic echocardiography and the recommended steps for successful transition from transesophageal to transthoracic echocardiography.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transcatheter aortic valve replacement (TAVR) has revolutionized the approach to symptomatic severe aortic stenosis (AS). As the clinical trials showed equivalence or even superiority of TAVR in the treatment of severe AS in inoperable/prohibited-risk and high-risk patients over the conventional treatment [1,2,3,4], TAVR was granted a Class I recommendation in American Heart Association/American College of Cardiology (AHA/ACC) valvular guidelines for the treatment of this group of patients [5, 6]. In addition, TAVR has a Class IIa recommendation in the AHA/ACC guidelines for the treatment of intermediate-risk patients with severe symptomatic AS [5, 6]. However, this recommendation is expected to advance to Class I as subsequent clinical trials have shown overwhelming evidence of safety and efficacy [7, 8].
During the early years of TAVR, the primary focus was on patient safety and procedural success. All of these early cases were performed using general anesthesia and transesophageal echocardiography (TEE). As the number of TAVR procedure performed annually has steadily increased [9, 10], attention has shifted to reducing patient recovery time and hospital length of stay. Such measures are important to address, especially with ongoing trials assessing the efficacy of TAVR among low-risk patients and the anticipation of its utilization among this patient population [11]. In an attempt to reduce the invasiveness, cost, and post-operative hospitalization, a “minimalistic approach” was adopted to perform TAVR utilizing the transfemoral access with monitored anesthesia care (MAC)/conscious sedation and intraprocedural transthoracic echocardiography (TTE). This minimalist approach has shown similar outcomes in comparison to conventional TAVR performed in the hybrid operating room using general anesthesia and transesophageal echocardiography (TEE) guidance [12,13,14].
Many centers, including ours, have made this transitional change from the use of general anesthesia and intraprocedural TEE to the use of MAC and TTE guidance. This transition was made possible with the advances and improvement in transcatheter heart valve (THV) design and the increased experience of the TAVR team. For a successful and smooth transition to perform TAVR under MAC and TTE guidance, the TAVR team (including the imagers) must acquire in-depth knowledge about the aortic root complex anatomy, echocardiographic imaging of the aortoannular complex, and the technical features and nuances of the commercially available THV.
Echocardiography for transcatheter aortic valve replacement
Pre-procedural assessment
The first step in the preprocedural imaging for TAVR is the assessment of the aortic valve (AV) morphology and the severity of the valve stenosis using TTE (Table 1). Identifying the presence of a bicuspid aortic valve, a traditional exclusion criteria for early TAVR trials, is essential. The number of leaflets is determined using the AV short-axis view during systole. In addition, it is important to determine the severity of the valvular calcification and its extension into the left ventricular outflow tract (LVOT), a strong predictor of post-TAVR paravalvular regurgitation (PVR) [15, 16]. To assess the AS severity, three parameters must be quantified accurately, namely, AV velocity and velocity time integral (VTIAV), left ventricular outflow tract (LVOT) velocity and velocity time integral (VTILVOT), and LVOT diameter. Careful calculation of stroke volume is also important since gradients are dependent on flow. In addition, it is essential to assess the left ventricular systolic and diastolic function and the presence of any concomitant significant valvular lesion(s). Published guidelines elegantly outline how to perform accurate assessment and quantification of AS [17].
The other essential step in the preprocedural imaging is the assessment of the aortoannular complex. Piazza et al. [18] described the aortic root as a complex 3-dimensional (3D) structure that separates the LVOT from the systemic circulation with 3 circular rings (sinotubular junction, anatomic ventriculo-arterial junction, and the aortic annulus) and a crown-like ring (interleaflet trigones) (Fig. 1). The tightest point in the aortic root is the aortic annulus, a virtual ring with its three anchors at nadir of the AV leaflets. Aortic annulus measured in systole is the main parameter used for sizing of TAVR [19, 20]. Accurate sizing of the aortic annulus is essential to avoid undersizing of the THV, which increases the risk of prosthesis embolization and PVR, or oversizing of the THV, which can result in underexpansion of the THV, conduction disturbances, and annulus rupture [19, 20].
Schematic presentation of the aortic root. Aortic root consists of 3 circular rings (aortic annulus, anatomic annulus, and sinotubular junction). The anatomic annulus (yellow ring) is at the attachment of the semilunar aortic leaflet to the aortic sinuses. The aortic annulus (orange ring) is a virtual annulus determined by the lowest hinge points of the aortic leaflets. Aortic valve leaflets are depicted in this figure showing the continuity of left coronary cusp (L) with aortomitral curtain and MVAL, the relationship of the right coronary cusp (R) to the muscular septum, and the relationship of the non-coronary cusp (NC) with the membranous septum. There is close proximity of the atrioventricular node and bundle as it passes below the membranous septum on the top of the muscular septum and then it divides into right and left bundle branches. This figure adopted with permission from Hahn et al [20]. IVS interventricular septum, L left coronary cusp, LMA left main artery ostium, MVAL mitral valve anterior leaflet, NC non-coronary cusp, R right coronary cusp, RCA right coronary artery ostium
Multidetector computed tomography (MDCT) is currently the primary modality used for aortoannular assessment given its high resolution and the 3D nature of the study. MDCT also provides essential information about the coronary height, severity and location of the aortic root calcification, and peripheral vascular assessment for the determination of the appropriate access site for TAVR [19, 20]. Although MDCT has shown to be more accurate in measuring the aortic annulus and reducing PVR after TAVR compared to 2-dimensional (2D) echo [21,22,23], other studies utilizing 3D echo have demonstrated similar precision in assessing the aortic annulus and equivalent accuracy in predicting PVR. Therefore, 3D echo, especially when TEE is utilized [24,25,26,27,28], is a feasible alternative modality for the assessment of aortic root and coronary heights in preprocedural planning for TAVR when the patient cannot undergo MDCT (Table 1).
Intraprocedural assessment
Echocardiography is useful for intraprocedural monitoring of TAVR during the different steps of THV deployment. Either TTE or TEE can be utilized during the procedure, besides fluoroscopy and aortography, for guiding the wire/catheter positioning, assessing post-balloon valvuloplasty results, appropriate positioning of the THV prior to deployment, and evaluating post-deployment results and complication(s) (Table 2). It is critical to be familiar with the THV used in the institution and the landmarks and measurement used to ensure appropriate landing zone of the valve. For example, in the balloon-expandable (Sapien 3, Edward Lifesciences) prosthesis, the valve depth should be 1–2 mm below the aortic annulus but because this valve, once it is deployed, can only be shortened from the ventricular size, it is more critical to assess the aortic aspect of the valve ensuring the valve is below the sinotubular junction and covering the native leaflets [20]. Another example is the self-expanding (Corevalve, Medtronic), the focus should be on the ventricular side of the valve to ensure that it extends 2-4 mm (not more than 6 mm) below the annulus [20]. Low implantation of the valve can result in conduction abnormalities, inference with mitral valve function, and embolization of the valve to the left ventricle. Too high implantation of the valve increases the risk of valve embolization to the aorta, jeopardizing the coronary flow, and aortic root injury (Fig. 2).
Transcatheter heart valve malpositioning. a Midesophageal LVOT long-axis view demonstrating a balloon expandable (Sapien 3, Edwards Lifesciences) valve that is implanted too low in the LVOT (yellow arrow). b Midesophageal LVOT long-axis view showing a balloon expandable (Sapien 3, Edwards Lifesciences) valve implanted too high in the aorta (red arrow). Ao aorta, LA left atrium, LV left ventricle, LVOT left ventricular outflow tract
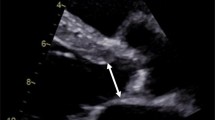
The main difference between TTE and TEE during the intraprocedural monitoring for TAVR is that TEE provides continuous monitoring during the procedure with higher image resolution but these advantages are at the expense of being more invasive (Table 3). Otherwise, both TTE and TEE offer comparable information to ensure appropriate THV placement and to identify periprocedural complication(s). In either modality, multiple views above, through, and below the THV with multiple-beat sweeps are essential to identify periprocedural complications, especially PVR (Fig. 3). As experience with TAVR has grown, there has been a further shift to using fluoroscopy alone to guide THV placement [29] and using TTE immediately after valve deployment to assure proper placement and to assess for valvular and perivalvular regurgitation.
a Mid-esohpageal LVOT long-axis view is revealing a posteriorly located PVR (white arrow). b midesophageal AV short-axis view demonstrated a posteriorly located PVR at 12 o’clock (white arrow). c Midesophageal AV short-axis view demonstrating a central, valvular, regurgitation secondary to incomplete expansion of the prosthetic valve (red arrow). d Transthoracic PLAX view showing an anteriorly located PVR (yellow arrow). e Transthoracic PSAX view showing an anteriorly located PRV at 1 o’clock (yellow arrow). f Transthoracic A3C view showing a regurgitation jet that is difficult to determine its mechanism, PVR versus valvular regurgitation, from the same patient in panel D and E (yellow arrow). A3C apical 3-chamber, Ao aorta, LA left atrium, LV left ventricle, LVOT left ventricular outflow tract, PLAX parasternal long-axis, PSAX parasternal short-axis, PVR paravalvular regurgitation, RA right atrium, RV right ventricle
Postprocedural assessment
A comprehensive TTE is essential after TAVR to establish a baseline evaluation prior to discharge. The post-TAVR echo should have a full evaluation of the cardiac chambers, valvular function and position, including the calculation of the newly implanted THV area and gradients as well as the presence or absence of any procedural complication(s) (Table 4).
For the assessment of the THV function and its effective orifice area (EOA), an accurate measurement of the LVOT is essential. The LVOT should be measured at the ventricular edge of the THV stent, especially when a balloon-expandable valve is used, from the outer-edge to outer-edge while the pulsed-Doppler sample volume placed just proximal to the ventricular edge of the valve stent [20, 30]. Similar to preprocedural assessment, the AV velocity and VTI should be measured using continuous-wave Doppler obtained from multiple views including the right parasternal. A normal THV has a peak velocity of < 3 m/s, a mean pressure gradient of < 20 mmHg, an effective orifice area (EOA) > 1.1 cm2 and indexed EOA > 0.85 cm2/m2. The Doppler velocity index (normally > 0.35) is also useful to report especially when the LVOT diameter is difficult to measure [30].
The determination of the presence or absence of PVR is important to be documented in the baseline echo post-TAVR. This assessment should include describing the location, number, and severity of the PVR. For better identification and quantification of the PVR, multiple imaging planes with color Doppler and multi-beat sweeps are required to ensure complete visualization of the regurgitant jet(s). The main views in TTE for PVR assessment are: parasternal long-axi (with lateral to medial sweeps), parasternal short-axis (with aorta to LVOT sweeps), and Apical 3- and 5-chamber views (with rotational sweeps and off-axis views). Although multiple qualitative, semi-quantitative, and quantitative parameters are suggested by the Valve Academic Research Consortium-consensus document [30] for the determination of PVR severity, frequently these parameters are either difficult to obtain or not accurate in post-TAVR assessment of PVR. The main semi-quantitative parameter proposed for the assessment of PVR is the circumferential extent of PVR. This parameter is measured in the parasternal short-axis view at the ventricular side of the valve stent and, therefore, it is essential to obtain multiple imaging planes through the valve to ensure the full visualization of the jet(s). However, an imaging plane too far into the LVOT will overestimate the extent of the PVR as the jet widens. Due to the complexity and difficulty in determining the PVR severity, Pibarot et al. [31] have suggested a 5-class grading scale for more accurate assessment of PVR.
Outcome comparison between intraprocedural TTE versus TEE
With the rapid adoption of TAVR for the treatment of severe aortic stenosis and the increased experience of operators with pre-TAVR planning and device implantation, there has been a gradual transition to improve the quality and cost of care for the TAVR population. In the early experience of TAVR implantation, TEE was used to assist with valve sizing, to monitor for appropriate valve placement across the aortic valve annulus and to identify procedural complications rapidly. However, newer generation device registries suggest that there is a temporal trend towards simplified or “minimalist” TAVR, with the use of local anesthesia and conscious sedation under TTE guidance and the avoidance of invasive hemodynamic monitoring, general anesthesia, and TEE that characterized the early TAVR experience [32, 33].
At the center of the debate for TEE-guided TAVR versus TTE-guided TAVR is the detection of PVR. This is because major complications are usually quickly identified due to hemodynamic instability. Rapid conversion to general anesthesia and placement of a TEE probe can then quickly be performed. Correct device placement has been shown to be effective with angiographic guidance [29] and, thus, has become less reliant on echo. The presence of moderate or greater perivalvular leak, defined using the Valve Academic Research Consortium 2 guidelines, has been identified as a risk factor for post-procedural mortality and impaired left ventricular remodeling [30, 34,35,36,37,38].
The evaluation of PVR by both TTE and TEE can be difficult and thus, skill is required to acquire and interpret the images. The metallic annulus of the deployed valve along with the compacted calcified valve leads to significant acoustic shadowing of the valvular annulus. It is also difficult to follow the true path of the perivalvular leak, as the regurgitant blood likely follows a non-linear pathway around the valvular annulus leading to over- and underestimation of the significance of each regurgitant lesion. Pre-procedural planning using multi-detector computed tomography may assist in the identification of those patients at increased risk of hemodynamically significant PVR, as data suggest that valve calcium score, extremes of implantation depth and valve under-sizing are predictive of greater than moderate perivalvular regurgitation [34, 39]. Abdel-Wahab and colleagues also suggest that pre-procedural use of TEE for determination of valve size is associated with moderate perivalvular regurgitation [40]. Patients with these factors may require extra care in identifying hemodynamically significant PVR. Regardless, post-procedure TTE and intra-procedure TEE have modest agreement in the detection of PVR [14, 41].
The adoption of minimalist TAVR has been extensively studied. The adoption of a minimalist TAVR protocol including local anesthesia combined with conscious sedation, angiographic placement of the TAVR valve, and use of post-procedure TTE has shown to require less procedural adrenergic support [42] and has led to a significantly decreased procedure time [13, 43,44,45]. Patients undergoing minimalist TAVR also have decreased post-procedural monitoring in the cardiac intensive care unit [13, 43, 46] and decreased hospital length of stay [13, 43, 44, 47]. This decreased length of stay translates into decreased cost of hospitalization [13, 47]. Importantly, there is no significant increase in significant PVR, major complications or mortality with minimalist TAVR [13, 42,43,44,45, 47,48,49,50]. These profound effects on patient care have led to the development of care pathways to improve and expedite safe and high-quality post-procedure TAVR care [51,52,53,54,55].
Transition from TEE to TTE during the TAVR procedure
As the learning curve and experience of the operator increase with the number of procedures performed, the transition from conventional approach with general anesthesia and TEE to the minimalist approach with MAC and TTE is possible. However, the change should be performed in a stepwise fashion and fulfilling specific requirements. In general, centers with low volume (< 50/year) and, thus, less experience would not be advised to adopt the minimalistic approach [56, 57]. Highly experienced sonographers or physicians with extensive training in TAVR imaging are pivotal for this transition. Moreover, the immediate availability of non-invasive cardiologist or anesthesiologist with expertise in TAVR imaging and the ability to quickly switch from TTE to TEE is mandatory.
The transition from the conventional to the minimalist approach is recommended once a center has achieved sufficient experience with TAVR. There is no specific number to determine the appropriate time for safe transition to the minimalistic approach, but in general, approximately one hundred cases is considered to be an acceptable transitional point. During the pre-transition phase, the selected sonographers or physicians that will be performing the TTE imaging during the TAVR procedure should undergo extensive training for TAVR imaging. The training should include an understanding of the aorto-annular anatomy, AV stenosis assessment, the correct positioning of the different THV utilized in the institution, and the methods of assessing complications including PVR and annulus perforation using multiple continuous sweeps and off-axis views. A clear and well-established protocol for periprocedural TTE assessment of TAVR should be reviewed by the TAVR team and approved by the director of the echo lab to ensure a comprehensive assessment of the AV. Table 5 is the protocol adopted by our echo lab for TAVR imaging.
Finally, it is essential to establish a TAVR team consisting of the interventional cardiologist, cardiothoracic surgeon, anesthesiologists and non-invasive cardiac imagers. All cases should be discussed ahead of time to determine the risk of the procedure and whether general anesthesia and TEE are needed based on the patient’s characteristics and the selected access site. In addition, it is critical to distribute a weekly updated list of the TAVR procedures to the assigned team members performing the procedure.
Conclusion
TAVR has become the standard of care for the management of those with symptomatic severe AS and high or prohibitive surgical risk and a reasonable option for those at intermediate risk. The indications for TAVR have expanded rapidly over the last decade. As a result, there has been a dramatic increase in the number of TAVR procedure performed worldwide. A minimalistic approach utilizing MAC and TTE procedural guidance has emerged as a safe and efficient approach in the appropriate patients in institutions with adequate experience with TAVR without compromising the procedural success and clinical outcomes.
Abbreviations
- AS:
-
Aortic stenosis
- AV:
-
Aortic valve
- EOA:
-
Effective orifice area
- LVOT:
-
Left ventricular outflow tract
- MDCT:
-
Multidetector computed tomography
- PVR:
-
Paravalvular regurgitation
- TAVR:
-
Transcatheter aortic valve replacement
- TEE:
-
Transesophageal echocardiography
- THV:
-
Transcatheter heart valve
- TTE:
-
Transthoracic echocardiography
- VTI:
-
Velocity time Integral
- 2-D:
-
2-dimensional
- 3-D:
-
3-dimensional
References
Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363:1597–607.
Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364:2187–98.
Makkar RR, Fontana GP, Jilaihawi H, et al. Transcatheter aortic-valve replacement for inoperable severe aortic stenosis. N Engl J Med. 2012;366:1696–704.
Adams DH, Popma JJ, Reardon MJ, et al. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med. 2014;370:1790–8.
Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC Guideline for the management of patients with valvular heart disease: a report of the american college of cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol. 2017;70:252–89.
Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2017;38:2739–91.
Leon MB, Smith CR, Mack MJ, et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016;374:1609–20.
Reardon MJ, Van Mieghem NM, Popma JJ, et al. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2017;376:1321–31.
Grover FL, Vemulapalli S, Carroll JD, et al. 2016 Annual Report of The Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. J Am Coll Cardiol. 2017;69:1215–30.
Holmes DR Jr, Nishimura RA, Grover FL, et al. Annual outcomes with transcatheter valve therapy: from the STS/ACC TVT registry. Ann Thorac Surg. 2016;101:789–800.
Thyregod HG, Steinbruchel DA, Ihlemann N, et al. Transcatheter versus surgical aortic valve replacement in patients with severe aortic valve stenosis: 1-year results from the all-comers NOTION randomized clinical trial. J Am Coll Cardiol. 2015;65:2184–94.
Gurevich S, Oestreich B, Kelly RF, et al. Outcomes of transcatheter aortic valve replacement using a minimalist approach. Cardiovasc Revasc Med. 2018;19:192–5.
Babaliaros V, Devireddy C, Lerakis S, et al. Comparison of transfemoral transcatheter aortic valve replacement performed in the catheterization laboratory (minimalist approach) versus hybrid operating room (standard approach): outcomes and cost analysis. JACC Cardiovasc Interv. 2014;7:898–904.
Hayek SS, Corrigan FE 3rd, Condado JF, et al. Paravalvular regurgitation after transcatheter aortic valve replacement: comparing transthoracic versus transesophageal echocardiographic guidance. J Am Soc Echocardiogr. 2017;30:533–40.
Khalique OK, Hahn RT, Gada H, et al. Quantity and location of aortic valve complex calcification predicts severity and location of paravalvular regurgitation and frequency of post-dilation after balloon-expandable transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2014;7:885–94.
Hansson NC, Norgaard BL, Barbanti M, et al. The impact of calcium volume and distribution in aortic root injury related to balloon-expandable transcatheter aortic valve replacement. J Cardiovasc Comput Tomogr. 2015;9:382–92.
Baumgartner H, Hung J, Bermejo J, et al. Recommendations on the Echocardiographic Assessment of Aortic Valve Stenosis: a Focused Update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J Am Soc Echocardiogr. 2017;30:372–92.
Piazza N, de Jaegere P, Schultz C, et al. Anatomy of the aortic valvar complex and its implications for transcatheter implantation of the aortic valve. Circ Cardiovasc Interv. 2008;1:74–81.
Kasel AM, Cassese S, Bleiziffer S, et al. Standardized imaging for aortic annular sizing: implications for transcatheter valve selection. JACC Cardiovasc Imaging. 2013;6:249–62.
Hahn RT, Nicoara A, Kapadia S, et al. Echocardiographic imaging for transcatheter aortic valve replacement. J Am Soc Echocardiogr. 2018;31:405–33.
Pontone G, Andreini D, Bartorelli AL, et al. Aortic annulus area assessment by multidetector computed tomography for predicting paravalvular regurgitation in patients undergoing balloon-expandable transcatheter aortic valve implantation: a comparison with transthoracic and transesophageal echocardiography. Am Heart J. 2012;164:576–84.
Tsang JF, Lytwyn M, Farag A, et al. Multimodality imaging of aortic dimensions: comparison of transthoracic echocardiography with multidetector row computed tomography. Echocardiography. 2012;29:735–41.
Tsuneyoshi H, Komiya T, Shimamoto T. Accuracy of aortic annulus diameter Measurement: comparison of multi-detector CT, two- and three-dimensional echocardiography. J Card Surg. 2016;31:18–22.
Husser O, Holzamer A, Resch M, et al. Prosthesis sizing for transcatheter aortic valve implantation–comparison of three dimensional transesophageal echocardiography with multislice computed tomography. Int J Cardiol. 2013;168:3431–8.
Janosi RA, Plicht B, Kahlert P, et al. Quantitative analysis of aortic valve stenosis and aortic root dimensions by three-dimensional echocardiography in patients scheduled for transcutaneous aortic valve implantation. Curr Cardiovasc Imaging Rep. United States2014:9296.
Jilaihawi H, Doctor N, Kashif M, et al. Aortic annular sizing for transcatheter aortic valve replacement using cross-sectional 3-dimensional transesophageal echocardiography. J Am Coll Cardiol. 2013;61:908–16.
Khalique OK, Kodali SK, Paradis JM, et al. Aortic annular sizing using a novel 3-dimensional echocardiographic method: use and comparison with cardiac computed tomography. Circ Cardiovasc Imaging. 2014;7:155–63.
Tamborini G, Fusini L, Muratori M, et al. Feasibility and accuracy of three-dimensional transthoracic echocardiography vs. multidetector computed tomography in the evaluation of aortic valve annulus in patient candidates to transcatheter aortic valve implantation. Eur Heart J Cardiovasc. Imaging. 2014;15:1316–23.
Attizzani GF, Ohno Y, Latib A, et al. Transcatheter aortic valve implantation under angiographic guidance with and without adjunctive transesophageal echocardiography. Am J Cardiol. 2015;116:604–11.
Kappetein AP, Head SJ, Genereux P, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. J Am Coll Cardiol. 2012;60:1438–54.
Pibarot P, Hahn RT, Weissman NJ, et al. Assessment of paravalvular regurgitation following TAVR: a proposal of unifying grading scheme. JACC Cardiovasc Imaging. 2015;8:340–60.
Wendler O, Schymik G, Treede H, et al. SOURCE 3: 1-year outcomes post-transcatheter aortic valve implantation using the latest generation of the balloon-expandable transcatheter heart valve. Eur Heart J. 2017;38:2717–26.
Auffret V, Lefevre T, Van Belle E, et al. Temporal trends in transcatheter aortic valve replacement in France: FRANCE 2 to FRANCE TAVI. J Am Coll Cardiol. 2017;70:42–55.
Athappan G, Patvardhan E, Tuzcu EM, et al. Incidence, predictors, and outcomes of aortic regurgitation after transcatheter aortic valve replacement: meta-analysis and systematic review of literature. J Am Coll Cardiol. 2013;61:1585–95.
Kodali S, Pibarot P, Douglas PS, et al. Paravalvular regurgitation after transcatheter aortic valve replacement with the Edwards sapien valve in the PARTNER trial: characterizing patients and impact on outcomes. Eur Heart J. 2015;36:449–56.
Tamburino C, Capodanno D, Ramondo A, et al. Incidence and predictors of early and late mortality after transcatheter aortic valve implantation in 663 patients with severe aortic stenosis. Circulation. 2011;123:299–308.
Zahn R, Gerckens U, Linke A, et al. Predictors of one-year mortality after transcatheter aortic valve implantation for severe symptomatic aortic stenosis. Am J Cardiol. 2013;112:272–9.
Abdel-Wahab M, Zahn R, Horack M, et al. Aortic regurgitation after transcatheter aortic valve implantation: incidence and early outcome. Results from the German transcatheter aortic valve interventions registry. Heart. 2011;97:899–906.
Watanabe Y, Lefevre T, Arai T, et al. Can we predict postprocedural paravalvular leak after Edwards SAPIEN transcatheter aortic valve implantation? Catheter Cardiovasc Interv. 2015;86:144–51.
Abdel-Wahab M, Comberg T, Buttner HJ, et al. Aortic regurgitation after transcatheter aortic valve implantation with balloon- and self-expandable prostheses: a pooled analysis from a 2-center experience. JACC Cardiovasc Interv. 2014;7:284–92.
Teeter EG, Dakik C, Cooter M, et al. Assessment of paravalvular leak after transcatheter aortic valve replacement: transesophageal echocardiography compared with transthoracic echocardiography. J Cardiothorac Vasc Anesth. 2017;31:1278–84.
Motloch LJ, Rottlaender D, Reda S, et al. Local versus general anesthesia for transfemoral aortic valve implantation. Clin Res Cardiol. 2012;101:45–53.
Yamamoto M, Meguro K, Mouillet G, et al. Effect of local anesthetic management with conscious sedation in patients undergoing transcatheter aortic valve implantation. Am J Cardiol. 2013;111:94–9.
Frohlich GM, Lansky AJ, Webb J, et al. Local versus general anesthesia for transcatheter aortic valve implantation (TAVR)–systematic review and meta-analysis. BMC Med. 2014;12:41.
Sengupta PP, Wiley BM, Basnet S, et al. Transthoracic echocardiography guidance for TAVR under monitored anesthesia care. JACC Cardiovasc Imaging. 2015;8:379–80.
Jensen HA, Condado JF, Devireddy C, et al. Minimalist transcatheter aortic valve replacement: the new standard for surgeons and cardiologists using transfemoral access? J Thorac Cardiovasc Surg. 2015;150:833–9.
Attizzani GF, Alkhalil A, Padaliya B, et al. Comparison of outcomes of transfemoral transcatheter aortic valve implantation using a minimally invasive versus conventional strategy. Am J Cardiol. 2015;116:1731–6.
Oguri A, Yamamoto M, Mouillet G, et al. Clinical outcomes and safety of transfemoral aortic valve implantation under general versus local anesthesia: subanalysis of the French Aortic National CoreValve and Edwards 2 registry. Circ Cardiovasc Interv. 2014;7:602–10.
Durand E, Borz B, Godin M, et al. Transfemoral aortic valve replacement with the Edwards SAPIEN and Edwards SAPIEN XT prosthesis using exclusively local anesthesia and fluoroscopic guidance: feasibility and 30-day outcomes. JACC Cardiovasc Interv. 2012;5:461–7.
Bergmann L, Kahlert P, Eggebrecht H, et al. Transfemoral aortic valve implantation under sedation and monitored anaesthetic care—a feasibility study. Anaesthesia. 2011;66:977–82.
Lauck SB, Wood DA, Achtem L, et al. Risk stratification and clinical pathways to optimize length of stay after transcatheter aortic valve replacement. Can J Cardiol. 2014;30:1583–7.
Lauck SB, Wood DA, Baumbusch J, et al. Vancouver transcatheter aortic valve replacement clinical pathway: minimalist approach, standardized care, and discharge criteria to reduce length of stay. Circ Cardiovasc Qual Outcomes. 2016;9:312–21.
Noad RL, Johnston N, McKinley A, et al. A pathway to earlier discharge following TAVI: assessment of safety and resource utilization. Catheter Cardiovasc Interv. 2016;87:134–42.
Serletis-Bizios A, Durand E, Cellier G, et al. A prospective analysis of early discharge after transfemoral transcatheter aortic valve implantation. Am J Cardiol. 2016;118:866–72.
Durand E, Eltchaninoff H, Canville A, et al. Feasibility and safety of early discharge after transfemoral transcatheter aortic valve implantation with the Edwards SAPIEN-XT prosthesis. Am J Cardiol. 2015;115:1116–22.
Carroll JD, Vemulapalli S, Dai D, et al. Procedural experience for transcatheter aortic valve replacement and relation to outcomes: the STS/ACC TVT registry. J Am Coll Cardiol. 2017;70:29–41.
Wassef AWA, Rodes-Cabau J, Liu Y, et al. The learning curve and annual procedure volume standards for optimum outcomes of transcatheter aortic valve replacement: findings from an international registry. JACC Cardiovasc Interv. 2018;11:1669–79.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Menhel Kinno, Eric P. Cantey and Vera H. Rigolin declare that they have no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kinno, M., Cantey, E.P. & Rigolin, V.H. The transition from transesophageal to transthoracic echocardiography during transcatheter aortic valve replacement: an evolving field. J Echocardiogr 17, 25–34 (2019). https://doi.org/10.1007/s12574-018-0409-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12574-018-0409-1