Abstract
Purpose
The goal of this review is to provide a comprehensive overview of ML technologies used to diagnose, detect, predict, monitor, treat, control, and manage TB. In addition, the study aimed to present future challenges, research directions, and recommendations for diagnosing, detecting, predicting, and monitoring TB treatment using ML technologies.
Methods
Review of published papers regarding diagnosis, detection, prediction, and monitoring of TB treatment, using ML technologies. In line with other TB case studies and reports of organizational institutionalism and implementation studies for a digital health.
Results
The reviewed related research has successfully demonstrated that the application of ML technologies in the diagnosis, detection, prediction, monitoring, treatment, control and management of TB plays an important role in improving the quality of TB care and human health. The literature analyzed identified the key areas including future challenges, research directions and recommendations for diagnosing, detecting, predicting and monitoring TB treatment using ML technologies.
Conclusions
Knowledge of the state-of-the-art in the application of ML technologies in TB management and the identified research directions is beneficial for researchers and healthcare experts. It is recommended that policymakers should develop a mechanism to support the adoption of best practice of ML technologies regulations in the country's healthcare sector.






Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
WHO. Global tuberculosis report. Figshare. https://www.who.int/publications/i/item/9789240013131. Accessed 15 June 2022.
Rabozzi LG, Bonizzi E, Crespi C, et al. Emerging zoonoses: the one health approach. Safety Health Work. 2012;3:77–83.
Purohit M, Mustafa T. Laboratory diagnosis of extrapulmonary tuberculosis (EPTB) in a resource-constrained setting: State of the art, challenges and the need. J Clin Diag Res 2015;9(4):EE01.
Meraj SS, Yaakob R, Azman A, et al. Artificial intelligence in diagnosing tuberculosis. 2019.
Poling A, Weetjens B, Cox C, et al. Tuberculosis detection by giant African pouched rats. Behav Analyst. 2011;34(1):47–54.
CDC. Facts. Figshare. https://www.who.int/publications/i/item/9789240013131. Accessed 17 June 2022.
Alqudaihi KS, Aslam N, Khan IU, Almuhaideb AM, Alsunaidi SJ, et al. Cough sound detection and diagnosis using artificial intelligence techniques: Challenges and opportunities. IEEE Access. 2021;9:102327–44.
Botha GHR, Theron G, Warren RM, Klopper M, Dheda K, Helden PDV, et al. Detection of tuberculosis by automatic cough sound analysis. Physiol Meas. 2018;39(4):45005.
Exarchos KP, Aggelopoulou A, Oikonomou A, Biniskou T, Beli V, Antoniadou E, Kostikas K. Malay Kishore Dutta; Vojtech Myska; Radim Burget. IEEE J Biomed Health Inform. 2022;26(5):2331–8.
Doshi R, Falzon D, Thomas BV, Temesgen Z, Sadasivan L, Migliori GB, Raviglione M. Tuberculosis control, and the where and why of artificial intelligence. ERJ Open Res. 2017;3(2):1–5.
Kathrin Z, Riou J, Carl M, Marie B, Anastasia K, Simon B, et al. Estimating tuberculosis transmission risks in a primary care clinic in South Africa: Modeling of environmental and clinical data. J Infect Dis. 2022;225(9):1642–52.
Chaurasia V, Pal S. Data mining approach to detect heart disease. Int J Adv Comput Sci Inf Technol. 2013;2(4):ISSN: 2296–1739.
Prasanna D, Hsu KW, Srivastava J. Data mining for healthcare management. PSIAM Int Conf Data Mining.
Collin SM, Wurie F, Muzyamba MC, et al. Effectiveness of interventions for reducing TB incidence in countries with low TB incidence: a systematic review of reviews. Eur Respir Rev. 2019;28(4):1–28.
Batko K, Slȩzak A. The use of Big Data Analytics in healthcare. J Big Data. 2022;9(3):1–24.
Mirbabaie M, Stieglitz S, Frick NR, et al. Artificial intelligence in disease diagnostics: a critical review and classification on the current state of research guiding future. Direction Health Technol. 2021;11:693–731.
Stokes K, et al. A machine learning model for supporting symptom-based referral and diagnosis of bronchitis and pneumonia in limited resource settings. Biocybern Biomed Eng. 2021;41:1288–302.
Kovačevič Ž, et al. Prediction of medical device performance using machine learning techniques: Infant incubator case study. Health Technol. 2019. https://doi.org/10.1007/s12553-019-00386-5.
Badnjevi A, et al. Evidence-based clinical engineering: Machine learning algorithms for prediction of defibrillator performance. Biomed Signal Process Control. 2019.
Begic E, Pokvic LG, et al. From heart murmur to echocardiography: Congenital heart defects diagnostics using machine learning algorithms. Medicina Academica Mostariensia. 2019;9(2):236–46.
Ann A, Doreen BM. Leveraging data and AI to deliver on the promise of digital health. International Journal of Medical Informatics Benefits, Pitfalls, and Potential Bias in Health Care AI. 2021.
Callahan A, Shah NH. Machine learning in healthcare. In Key Advances in Clinical Informatics; Elsevier: Amsterdam, The Netherlands; 2021. p. 279–91.
Deelder W, et al. A modified decision tree approach to improve the prediction and mutation discovery for drug resistance in Mycobacterium tuberculosis. BMC Genom. 2022;23(46):2–7.
Gerald LB, et al. A decision tree for tuberculosis contact investigation: the one health approach. Am J Respir Crit Care Med. 2002;166(8):1122–7.
Ameri H, Alizadeh S, Hadizadeh M. Assessing the effects of infertility treatment drugs using clustering algorithms and data Mmining techniques. J Mazandaran Univ Med Sci. 2014;24:26–35 (Persian).
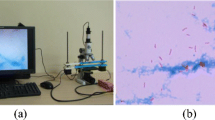
Zheng C, Liu J, Qiu G. Tuberculosis bacteria detection based on Random Forest using fluorescent images. 9th International Congress on Image and Signal Processing. BioMedical Engineering and Informatics (CISP-BMEI). 2016.
Ayas S, Ekinci M. Random forest-based tuberculosis bacteria classification in images of ZN-stained sputum smear samples. SIViP. 2014;8:49–61.
Basha SM, Rajput DS. Survey on evaluating the performance of machine learning algorithms: Past contributions and future roadmap. In Deep Learning and Parallel Computing Environment for Bioengineering Systems; Elsevier: Amsterdam, The Netherlands; 2019. p. 153–64.
Bordoloi DJ, Tiwari R. Optimum multi-fault classification of gears with integration of evolutionary and SVM algorithms. Mech Mach Theory. 2014;73:49–60.
Abbasi HN, Firouzi JF, Tabarsi P. Diagnosis Of pulmonary tuberculosis using artificial intelligence (Naive Bayes Algorithm). 2020;13(6):419–28.
Marx FM, Yaesoubi R, Menzies NA, Salomon JA, Bilinski A, Beyers B, Cohen T. Tuberculosis control interventions targeted to previously treated people in a high incidence setting: a modelling study. Lancet Global Health. 2018;6(4):e426–35.
Samaneh K, Yang Y, Timoth M, et al. Application of machine learning techniques to tuberculosis drug resistance analysis. 2019.
Kailasam P. Prediction of tuberculosis diagnosis using weighted KNN classifier, the Kopanyo study. Mukt Shabd J. 2021;1–8.
Moonan PK, Zetola NM, Tobias JL, et al. A neighbor-based approach to identify tuberculosis exposure, the Kopanyo study. Emerg Infect Dis. 2020;26(5):1010–3.
Mahmoud RS, Shahaboddin S, Shahram GH, et al. Diagnosing tuberculosis with a novel support vector machine-based artificial immune recognition system. Iran Red Crescent Med J. 2015;17(5):1–9.
Keethansana K, Maheshi BD. Prediction of treatment failure of tuberculosis using support vector machine with genetic algorithm. Int J Mycobacteriol. 2021;10(3):279–84.
Rakhmetulayev S, Duisebekova K, Mamyrbekov A, et al. Application of classification algorithm based on SVM for determining the effectiveness of treatment of tuberculosis. Proc Comput Sci. 2021;130(3):231–8.
Ali MH, Khan DM, Jamal K, Ahmad Z, Manzoor S, Khan Z. Prediction of multidrug-resistant tuberculosis using machine learning algorithms in swat, Pakistan. J Healthc Eng. 2021.
Nagabhushanam D, Naresh N, Raghunath A, Praveen Kumar K, et al. Prediction of tuberculosis using data mining techniques on Indian patient’s data. IJCST. 2013;4:262–5.
Khan MT, Kaushik AC, Linxiang, et al. Artificial neural networks for prediction of tuberculosis disease. Front Microbiol. 2019;4:262–5. https://doi.org/10.3389/fmicb.2019.00395.
Luo Y, Xue Y, Song H, Tang G, Liu W, Bai H, Yuan X, Tong S, Wang F, Cai Y, Sun Z. Machine learning based on routine laboratory indicators promoting the discrimination between active tuberculosis and latent tuberculosis. J Infect. 2022.
Xiong Y, Ba X, Hou A, et al. Automatic detection of mycobacterium tuberculosis using artificial intelligence. World Health Organization, European Respiratory Society; 2018. 2015.
Ruihua G, Kalpdrum P, Chakresh K, et al. Detection of tuberculosis based on deep learning based methods. J Phys. 2021.
Lino Ferreira da Silva Barros MH, Oliveira Alves G, Morais Florencio Souza L, et al. Benchmarking machine learning models to assist in the prognosis of tuberculosis. Informatics.
Salcedo J, Rosales M, Kim JS, et al. Cost-effectiveness of artificial intelligence monitoring for active tuberculosis treatment: a modeling study. PLoS One.
Lee Y, Raviglione MC, Flahault A. Use of digital technology to enhance tuberculosis control: Scoping. 2020.
Guo R, Pass K, Jain CK. Tuberculosis diagnostics and localization in chest x-rays via deep learning models. Medicine and Public Health. 2020.
Lapao LV. Seriously implementing health capacity strengthening programs in Africa. Int J Health Policy Manag. 2015;4(10):691–3. https://doi.org/10.15171/ijhpm.2015.130.
Anatole M, Lisa RH, Kenneth S, Cindy C. Mentorship and coaching to support strengthening healthcare systems: Lessons learned across the five Population Health Implementation and Training partnership projects in sub-Saharan Africa. BMC Health Serv Res. 2021;17(3):1–24. https://doi.org/10.1186/s12913-017-2656-7.
Tesema AG, Abimbola S, Mulugeta A, Ajisegiri WS, Narasimhan P, et al. Health system capacity and readiness for delivery of integrated non-communicable disease services in primary health care: a qualitative analysis of the Ethiopian experience. PLOS Glob Public Health. 2021;1(10):1–16. https://doi.org/10.1371/journal.pgph.0000026.
Ellen MHM, Claire R Moodie, Ochola, Suzanne C, Suzanne C. Innovations in TB data quality: An M & E Workshop Facilitators Guide; 2019.
WHO. Understanding and using tuberculosis data. 2014.
Jessica S, François C, Leduc N, Myra P, Melki W, Charfi F, et al. Building system capacity for the integration of mental health at the level of primary care in Tunisia: a study protocol in global mental health. BMC Health Serv Res. 2017;17(38):1–16. https://doi.org/10.1186/s12913-017-1992-y.
Moucheraud C, Schwitters A, Boudreaux C, et al. Sustainability of health information systems: a three-country qualitative study in southern Africa. BMC Health Serv Res. 2017;17(1):1–11.
Baloch NA, Pai M. Tuberculosis control: Business models for the private sector. Lancet Infect Dis. 2012;12(8):579–80.
Shibanuma A. Sustainability of a national programme for drug-resistant TB: Why does a well-designed programme stagnate? Public Health Action. 2020;10(4):133–133. https://doi.org/10.5588/pha.20.0075.
Nabyonga-Orem J, Asamani JA, Makanga. The state of health research governance in Africa: What do we know and how can we improve? Health Res Policy Sys.t 2021;19(11):1–14.
Kathleen L, David AS, Anneke L, et al. Patient data ownership: Who owns your health? J Law Biosci. 2021;8(2):1–50.
Galvin HK, DeMuro PR. Developments in privacy and data ownership in mobile health technologies, 2016–2019. Yearb Med Inform. 2020;29(1):32–43.
Michelsen K, Brand H, Achterberg P, Wilkinson J. Promoting better integration of health information systems: Best practices and challenges. World Health Organization (WHO) Regional office for Europe, Health Evidence Network synthesis report. 2015.
Walker D, Lawrence J, Yeager V. Progress and challenges with connecting hospitals with the public health system. Health Serv Res. 2020.
Sunny I, Humphrey K, Derrick M, Kajali G, Noel C, Okeibunor J. Strengthening health systems using innovative digital health technologies in Africa. Front Digital Health. 2022;4:1–8.
Mukasa E, Kimaro H, Kiwanuka A, et al. Challenges and strategies for standardizing information systems for integrated TB/HIV services in Tanzania: a case study of Kinondoni municipality. Electron J Inf Syst Develop Countries. 2020;79:1–11.
Ishijima H, Mapunda M, Mndeme M, et al. Challenges and opportunities for effective adoption of HRH information systems in developing countries. Electron J Inf Syst Dev Countries. 2020;(2):21–38.
Acknowledgements
We thank the anonymous reviewers for their insightful comments and suggestions that helped us improve the quality of the paper. This work was supported in part by the government of Tanzania through the Research and Innovation Grants of Sokoine University of Agriculture (SUA).
Funding
This work was supported by the Sokoine University of Agriculture [grant number CC003].
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this work.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
All authors participated equally in this work.
Consent for publication
All authors have declared a will to publish this work.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jonathan, J., Barakabitze, A.A. ML technologies for diagnosing and treatment of tuberculosis: a survey. Health Technol. 13, 17–33 (2023). https://doi.org/10.1007/s12553-023-00727-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-023-00727-5