Abstract
Objective
To assess frequency, clinical indications, and cumulative effective dose (CED) of patients undergoing multiple 18F-FDG PET/CT imaging.
Methods
Retrospective analysis of 18F-FDG PET/CT scans performed at a university hospital for 11 years was done. The effective dose was estimated from activity administered and dose-length-product.
Results
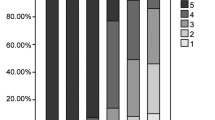
A total of 55,424 18F-FDG PET/CT scans were performed in 32,658 patients. The average injected activity was 421 MBq and median 417 MBq. 24.2% of the patients were scanned 2–5 times in a year, 16.7% of them being unique patients (not counted as a separate patient in different years). The maximum PET/CT scans in a year for any patient was five. 23,571 (72.2%) patients underwent a single 18 F-FDG PET/CT scan, while 9087 (27.8%) unique patients underwent 2–23 scans during 11 years. 82% of the scanned patients had a malignant disease, and 2.4% of patients with ≥ 2 18 scans in a year had non-malignant indications. 1.4% of patients received CED ≥ 100 mSv in one year from multiple 18 F-FDG PET/CT scans and 0.8% of them received ≥ 100 mSv in a year more than one time, the CED of 27.8% (9087 patients) who underwent 2 to 23 18F-FDG PET/CT scans over 11-years ranged from 38 to 575 mSv (median: 271 mSv).
Conclusion
This largest ever study covering analysis of 11-years’ data of 18F-FDG PET/CT patients showed that a sizeable number of patients, largely with malignant disease (82%) undergo recurrent imaging during one year and non-ignorable fraction exceed 100 mSv in one year.





Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding authors upon request.
Change history
13 January 2023
A Correction to this paper has been published: https://doi.org/10.1007/s12553-023-00729-3
References
Almuhaideb A, Papathanasiou N, Bomanji J. 18F-FDG PET/CT imaging in oncology. Ann Saudi Med. 2011;31(1):3–13. https://doi.org/10.4103/0256-4947.75771. PMID: 21245592; PMCID: PMC3101722.
Zhuang H, Codreanu I. Growing applications of FDG PET-CT imaging in non-oncologic conditions. J Biomed Res. 2015;29(3):189–202. https://doi.org/10.7555/JBR.29.20140081. Epub 2015 Mar 8. PMID: 26060443; PMCID: PMC4449487.
Lawal I, Sathekge M. F-18 FDG PET/CT imaging of cardiac and vascular inflammation and infection. Br Med Bull. 2016;120(1):55–74. https://doi.org/10.1093/bmb/ldw035. Epub 2016 Sep 10. PMID: 27613996.
Love C, Tomas MB, Tronco GG, Palestro CJ. FDG PET of infection and inflammation. Radiographics. 2005;25(5):1357–68. https://doi.org/10.1148/rg.255045122. PMID: 16160116.
Kinahan PE, Fletcher JW. Positron emission tomography-computed tomography standardized uptake values in clinical practice and assessing response to therapy. Semin Ultrasound CT MR. 2010;31(6):496–505. https://doi.org/10.1053/j.sult.2010.10.001. PMID: 21147377; PMCID: PMC3026294.
Koolen BB, Vrancken Peeters MJ, Aukema TS, Vogel WV, Oldenburg HS, van der Hage JA, Hoefnagel CA, Stokkel MP, Loo CE, Rodenhuis S, Rutgers EJ, Valdés Olmos RA. 18F-FDG PET/CT as a staging procedure in primary stage II and III breast cancer: comparison with conventional imaging techniques. Breast Cancer Res Treat. 2012;131(1):117–26. https://doi.org/10.1007/s10549-011-1767-9. Epub 2011 Sep 21. PMID: 21935602.
Boellaard R, Delgado-Bolton R, Oyen WJ, Giammarile F, Tatsch K, Eschner W, Verzijlbergen FJ, Barrington SF, Pike LC, Weber WA, Stroobants S, Delbeke D, Donohoe KJ, Holbrook S, Graham MM, Testanera G, Hoekstra OS, Zijlstra J, Visser E, Hoekstra CJ, Pruim J, Willemsen A, Arends B, Kotzerke J, Bockisch A, Beyer T, Chiti A, Krause BJ. European Association of Nuclear Medicine (EANM). FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging. 2015;42(2):328–54. https://doi.org/10.1007/s00259-014-2961-x. Epub 2014 Dec 2. PMID: 25452219; PMCID: PMC4315529.
Prieto E, García-Velloso MJ, Rodríguez-Fraile M, Morán V, García-García B, Guillén F, Morales MI, Sancho L, Peñuelas I, Richter J, Martí-Climent JM. Significant dose reduction is feasible in FDG PET/CT protocols without compromising diagnostic quality. Phys Med. 2018;46:134–9. https://doi.org/10.1016/j.ejmp.2018.01.021. Epub 2018 Feb 6. PMID: 29519399.
Sagara H, Inoue K, Yaku H, Ohsawa A, Someya T, Yanagisawa K, Ohashi S, Ishigaki R, Wakabayashi M, Muramatsu Y, Fujii H. Optimization of injection dose in 18F-FDG PET/CT based on the 2020 national diagnostic reference levels for nuclear medicine in Japan. Ann Nucl Med. 2021. https://doi.org/10.1007/s12149-021-01656-x. Epub ahead of print. PMID: 34287782.
Indrakanti S, Li X, Rehani MM. Patients undergoing multiple 18F-FDG PET/CT exams: Assessment of frequency, dose and disease classification. Br J Radiol. 2022;95(1135):20211225. https://doi.org/10.1259/bjr.20211225. Epub 2022 May 5. PMID: 35348374.
ICRP. Radiation Dose to Patients from Radiopharmaceuticals: A Compendium of Current Information Related to Frequently Used Substances. 2015
Deak PD, Smal Y, Kalender WA. Multisection CT protocols: sex- and age-specific conversion factors used to determine effective dose from dose-length product. Radiology. 2010;257(1):158–66. https://doi.org/10.1148/radiol.10100047.
UNSCEAR. Biological Mechanisms of radiation actions at low doses: a white paper to guide the scientific committee’s future program of work. New York: United Nations; 2012. United Nations Scientific Committee.
Brower C, Rehani MM. Radiation risk issues in recurrent imaging. Br J Radiol. 2021;94(1126):20210389. https://doi.org/10.1259/bjr.20210389. Epub 2021 Jun 23. PMID: 34161140.
Rehani MM, Brady Z. Contemporary issues in radiation protection in medical imaging: introductory editorial. Br J Radiol. 2021;94(1126):bjr20219004. https://doi.org/10.1259/bjr.20219004. PMID: 34545765.
OECD. Health care resources (Edition 2019), OECD Health Statistics (database). 2020. https://doi.org/10.1787/36551532-en. Accessed on 01 September 2021. https://stats.oecd.org/Index.aspx?ThemeTreeId=9.
Rehani MM, Hauptmann M. Estimates of the number of patients with high cumulative doses through recurrent CT exams in 35 OECD countries. Phys Med. 2020;76:173–6. https://doi.org/10.1016/j.ejmp.2020.07.014. Epub 2020 Jul 18. PMID: 32693353.
Vali R, Alessio A, Balza R, Borgwardt L, Bar-Sever Z, Czachowski M, Jehanno N, Kurch L, Pandit-Taskar N, Parisi M, Piccardo A, Seghers V, Shulkin BL, Zucchetta P, Lim R. SNMMI Procedure Standard/EANM Practice Guideline on Pediatric 18F-FDG PET/CT for Oncology 1.0. J Nucl Med. 2021;62(1):99–110. https://doi.org/10.2967/jnumed.120.254110. PMID: 33334912.
European Commission. Medical Radiation Exposure of the European Population. Radiation Protection N° 180. 2015. r https://ec.europa.eu/energy/sites/ener/files/documents/RP180%20part2.pdf.
Abe K, Hosono M, Igarashi T, Iimori T, Ishiguro M, Ito T, Nagahata T, Tsushima H, Watanabe H. The 2020 national diagnostic reference levels for nuclear medicine in Japan. Ann Nucl Med. 2020;34(11):799–806. https://doi.org/10.1007/s12149-020-01512-4. Epub 2020 Aug 27. PMID: 32852747; PMCID: PMC7584529.
Song HC, Na MH, Kim J, Cho SG, Park JK, Kang KW. Korean Society of Nuclear Medicine Diagnostic Reference Level Task Force. Diagnostic reference levels for Adult Nuclear Medicine Imaging established from the National Survey in Korea. Nucl Med Mol Imaging. 2019;53(1):64–70. https://doi.org/10.1007/s13139-019-00585-y. Epub 2019 Feb 1. PMID: 30828403; PMCID: PMC6377576.
Rehani MM, Melick ER, Alvi RM, Doda Khera R, Batool-Anwar S, Neilan TG, Bettmann M. Patients undergoing recurrent CT exams: assessment of patients with non-malignant diseases, reasons for imaging and imaging appropriateness. Eur Radiol. 2020;30(4):1839–46. https://doi.org/10.1007/s00330-019-06551-8. Epub 2019 Dec 2. PMID: 31792584.
AAPM/ACR/HPS Joint Statement on Proper Use of Radiation Dose Metric Tracking for Patients Undergoing Medical Imaging Exams. PP 35-A. https://www.aapm.org/org/policies/details.asp?id=1533, https://www.acr.org/Media-Center/ACR-News-Releases/2021/Disputed-EHR-Dose-Levels-Could-KeepPatients-From-Getting-Necessary-Imaging-Exams.
Seuri R, Rehani MM, Kortesniemi M. How tracking radiologic procedures and dose helps: experience from Finland. AJR Am J Roentgenol. 2013;200(4):771–5. https://doi.org/10.2214/AJR.12.10112.
Rehani MM, Brady Z. Contemporary issues in radiation protection in medical imaging: introductory editorial. Br J Radiol. 2021;94(1126):bjr20219004. https://doi.org/10.1259/bjr.20219004.
International Atomic Energy Agency, European Federation of Organizations for Medical Physics, European Society of Radiology, Global Diagnostic Imaging, Healthcare IT and Radiation Therapy Trade Association (DITTA), Heads of European Radiological Competent Authorities, Image Gently Alliance, International Organization for Medical Physics, International Society of Radiology, International Society of Radiographers and Radiological Technologists. Joint Position Statement And Call For Action For Strengthening Radiation Protection Of Patients Undergoing Recurrent Radiological Imaging Procedures. 18. May 2021. https://www.iaea.org/resources/article/joint-position-statement-and-call-for-action-for-strengthening-radiation-protection-of-patients-undergoing-recurrent-radiological-imaging-procedures.
Joint Position Statement on the IAEA Patient Radiation Exposure Tracking. European Society of Radiology (ESR), U.S. Food and Drug Administration (FDA), International Atomic Energy Agency (IAEA), International Organization for Medical Physics (IOMP), International Society of Radiographers & Radiological Technologists (ISRRT), World Health Organization (WHO), Conference of Radiation Control Program Directors, USA (CRCPD). 2012. https://www.iaea.org/sites/default/files/documents/rpop/iaea-smart-card-position-statement.pdf; https://www.iaea.org/sites/default/files/documents/rpop/cover-iaea-joint-position-statement-smart-card.pdf.
Rehani MM. Old enemy, new threat: you can’t solve today’s problems with yesterday’s solution. J Radiol Prot. 2021;41(2). https://doi.org/10.1088/13616498/abe2ba. Published 2021 Jun 1.
Vassileva J, Holmberg O. Radiation protection perspective to recurrent medical imaging: what is known and what more is needed? Br J Radiol. 2021;94(1126):20210477. https://doi.org/10.1259/bjr.20210477.
Rehani MM, Berris T. International Atomic Energy Agency study with referring physicians on patient radiation exposure and its tracking: a prospective survey using a web-based questionnaire. BMJ Open. 2012;2(5):e001425. Published 2012 Sep 20. https://doi.org/10.1136/bmjopen-2012-001425.
Martin CJ, Harrison JD, Rehani MM. Effective dose from radiation exposure in medicine: past, present, and future. Phys Med. 2020;79:87–92. https://doi.org/10.1016/j.ejmp.2020.10.020. Epub 2020 Nov 13. PMID: 33197830.
Mercuri M, Rehani MM, Einstein AJ. Tracking patient radiation exposure: challenges to integrating nuclear medicine with other modalities. J Nucl Cardiol. 2012;19(5):895–900. https://doi.org/10.1007/s12350-012-9586-x. PMID: 22695788; PMCID: PMC3683971.
Brower C, Rehani MM. Radiation risk issues in recurrent imaging. Br J Radiol. 2021:20210389. https://doi.org/10.1259/bjr.20210389. Epub ahead of print. PMID: 34161140.
Harrison JD, Balonov M, Bochud F, Martin C, Menzel HG, Ortiz-Lopez P, Smith-Bindman R, Simmonds JR, Wakeford R. ICRP Publication 147: Use of Dose Quantities in Radiological Protection. Ann ICRP. 2021;50(1):9–82. https://doi.org/10.1177/0146645320911864. PMID: 33653178.
Inoue Y, Nagahara K, Tanaka Y, Miyatake H, Hata H, Hara T. Methods of CT Dose Estimation in Whole-Body 18F-FDG PET/CT. J Nucl Med. 2015;56(5):695–700. https://doi.org/10.2967/jnumed.114.153718. Epub 2015 Apr 3. PMID: 25840979.
Quinn B, Dauer Z, Pandit-Taskar N, Schoder H, Dauer LT. Radiation dosimetry of 18F-FDG PET/CT: incorporating exam-specific parameters in dose estimates. BMC Med Imaging. 2016;16(1):41. https://doi.org/10.1186/s12880-016-0143-y. PMID: 27317478; PMCID: PMC4912712.
Martí-Climent JM, Prieto E, Morán V, Sancho L, Rodríguez-Fraile M, Arbizu J, García-Velloso MJ, Richter JA. Effective dose estimation for oncological and neurological PET/CT procedures. EJNMMI Res. 2017;7(1):37. https://doi.org/10.1186/s13550-017-0272-5. Epub 2017 Apr 24. PMID: 28439843; PMCID: PMC5403773.
Gallach M, Mikhail Lette M, Abdel-Wahab M, Giammarile F, Pellet O, Paez D. Addressing global inequities in Positron Emission Tomography-Computed tomography (PET-CT) for Cancer Management: a statistical model to Guide Strategic Planning. Med Sci Monit. 2020;26:e926544. https://doi.org/10.12659/MSM.926544. PMID: 32848125; PMCID: PMC7476356.
Fisher DR, Fahey FH. Appropriate use of effective dose in Radiation Protection and Risk Assessment. Health Phys. 2017;113(2):102–9. https://doi.org/10.1097/HP.0000000000000674. PMID: 28658055; PMCID: PMC5878049.
Costa PR, Yoshimura EM, Nersissian DY, Melo CS. Correlation between effective dose and radiological risk: general concepts. Radiol Bras. 2016;49(3):176–81. https://doi.org/10.1590/0100-3984.2014.0097. PMID: 27403018; PMCID: PMC4938448.
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the ethics committee xxxxx under decision No. 83045809-604.01.02-.
Consent to participate
Not applicable.
Conflicts of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The phrase “Original research” has been deleted in the article title.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abuqbeitah, M., Demir, M., Sönmezoğlu, K. et al. Patients undergoing multiple 18F-FDG PET/CT scans: frequency, clinical indications, and cumulative dose. Health Technol. 13, 89–97 (2023). https://doi.org/10.1007/s12553-022-00716-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-022-00716-0