Abstract
Background
Shift work with sleep disruption is a systemic stressor that may possibly be associated with blood pressure dysregulation and hypertension.
Purpose
We hypothesize that rotation to a simulated night shift with sleep deprivation will produce blood pressure elevations in persons at risk for development of hypertension.
Method
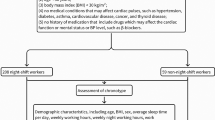
We examined the effects of a simulated night shift on resting blood pressure in 51 diurnal young adults without current hypertension. Resting blood pressure was monitored throughout a 24-h period of total sleep deprivation with sustained cognitive work. Twelve participants (23.5%) reported one or more parents with a diagnosis of hypertension. Ten participants were classified as prehypertensive by JNC-7 criteria. Only two prehypertensive subjects reported parental hypertension.
Results
Results indicate that, as the night shift progressed, participants with a positive family history of hypertension showed significantly higher resting diastolic blood pressure than those with a negative family history of hypertension (p = 0.007). Prehypertensive participants showed elevated blood pressure throughout the study.
Conclusion
These data suggest that rotation to a simulated night shift with sleep deprivation may contribute to blood pressure dysregulation in persons with a positive family history of hypertension.


Similar content being viewed by others
References
National Sleep Foundation. 2006 Sleep in America poll. 2006. January 8, 2007 from http://www.sleepfoundation.org/_content/hottopics/2006_summary_of_findings.pdf.
Pickering TG. Could hypertension be a consequence of the 24/7 society? The effects of sleep deprivation and shift work. J Clin Hypertens. 2006;8:819–22.
Egan BM. Sleep and hypertension: burning the candle at both ends really is hazardous to your health. Hypertension. 2006;47:816–7.
Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering T, et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47:833–9.
Gottlieb DJ, Redline S, Nieto FJ, Baldwin CM, Newman AB, Resnick HE, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29:1009–14.
Wright K. Too little sleep: a risk factor for obesity? Obesity Management. 2006;2:140–5.
Leineweber C, Kecklund G, Janszky I, Akerstedt T, Orth-Gomér K. Poor sleep increases the prospective risk for recurrent events in middle-aged women with coronary disease. J Psychosom Res. 2003;54(2):121–7.
Akerstedt T, Knutsson A, Alfredsson L, Theorell T. Shiftwork and cardiovascular disease. Scand J Work Environ & Health. 1984;10:409–14.
Knutsson A, Akerstedt T, Jonsson B, Orth-gomer K. Increased risk of ischaemic heart disease in shift workers. Lancet. 1986;8498:89–92.
Yamasaki F, Schwartz JE, Gerber LM, Warren K, Pickering TG. Impact of shift work and race/ethnicity on the diurnal rhythm of blood pressure and catecholamines. Hypertension. 1998;32:417–23.
Su T, Lin L, Baker D, Schnall P, Chen M, Hwang W, et al. Elevated blood pressure, decreased heart rate variability and incomplete blood pressure recovery after a 12-hour night shift work. J Occup Health. 2008;50:380–6.
Suwazono Y, Dochi M, Dakata K, Okubo Y, Oishi M, Tanaka K, et al. Shift work is a risk factor for increased blood pressure in Japanese men: a 14-year historical cohort study. Hypertension. 2008;52:581–6.
Esler M. The sympathetic system and hypertension. Am J Hypertens. 2000;13:99S–105.
McCubbin JA, Richardson JE, Langer AW, Kizer JS, Obrist PA. Sympathetic neuronal function and left ventricular performance during behavioral stress in young adults: the relationship between plasma catecholamines and systolic time intervals. Psychophysiol. 1983;20:102–10.
al’Absi M, Lovallo WR. Cortisol concentrations in serum of borderline hypertensive men exposed to a novel experimental setting. Psychoneuroendocrinol. 1993;18:355–63.
McCubbin JA, Surwit RS, Williams RB, Nemeroff CB, McNeilly M. Altered pituitary hormone response to naloxone in hypertension development. Hypertension. 1989;14:636–44.
Chang HM, Wu UI, Lin TB, Lan CT, Chien WC, Huang WL, et al. Total sleep deprivation inhibits the neuronal nitric oxide synthase and cytochrome oxidase reactivities in the nodose ganglion of adult rats. J Anat. 2006;209:239–50.
Mion D, Krieger EM. Blood pressure regulation after deprivation of rapid-eye-movement sleep in rats. J Hypertension. 1988;6 Suppl 4:74–6.
Tochikubo O, Ikeda A, Miyajima E, Masao I. Effects of insufficient sleep on blood pressure monitored by a new multibiomedical recorder. Hypertension. 1996;27:1318–24.
Ogawa Y, Kanbayashi T, Saito Y, Takahashi Y, Kitajima T, Takahashi K, et al. Total sleep deprivation elevates blood pressure through arterial baroreflex resetting: a study with microneurographic technique. Sleep. 2003;26:986–9.
Bonnet MH, Arand DL. Heart rate variability in insomniacs and matched normal sleepers. Psychosom Med. 1998;60:610–5.
JNC, 7. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. NIH Publication No. 03-5233, pp. 1–52. Washington, DC: US Department of Health and Human Services; 2003.
Hunt S, Williams RR, Barlow GK. A comparison of positive family history definitions for defining risk of future disease. J Chron Dis. 1986;39:809–21.
Light KC. Psychosocial precursors of hypertension: experimental evidence. Circ. 1987;76:I67–76.
Gerin W, Pickering TG. Association between delayed recovery of blood pressure after acute mental stress and parental history of hypertension. J Hypertens. 1995;13:603–10.
Pilcher JJ, McClelland LE, Moore DD, Haarmann H, Baron J, Wallsten TS, et al. Language performance under sustained work and sleep deprivation conditions. Aviation Space Environ Med. 2007;78:B25–38.
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure. Hypertension. 2005;45:142–61.
Hastrup J, Light KC, Obrist PA. Parental hypertension and cardiovascular response to stress in healthy young adults. Psychophysiol. 1982;19:615–22.
Manuck SB, Giordani B, McQuaid KJ, Garrity SJ. Behaviorally induced cardiovascular reactivity among sons of reported hypertensive and normotensive parents. J Psychosom Res. 1981;25:261–9.
McCubbin JA, Helfer SG, Switzer FS, Galloway C, Griffith WV. Opioid analgesia in persons at risk for hypertension. Psychosom Med. 2006;68:116–20.
Moore-Ede MC, Richardson GS. Medical implications of shift-work. Rev Méd. 1985;36:607–17.
Peter JH, Penzel T, Podszus T, von Wichert P, editors. Sleep and health risk. Berlin: Springer; 1991.
Sternberg H, Rosenthal T, Shamiss A, Green M. Altered circadian rhythm of blood pressure in shift workers. J Hum Hypertension. 1995;9:349–53.
Rutenfranz J, Colquhoun WP, Knauth P, Ghata JN. Biomedical and psychosocial aspects of shift work. Scand J Work Environ Health. 1977;3:165–82.
Monk TH. Coping with the stress of shift work. Work Stress. 1988;2:169–72.
Penn PE, Bootzin RR. Behavioral techniques for enhancing alertness and performance in shift work. Work Stress. 1990;4:213–26.
Scott AJ, Ladou J. Shift-work: effects on sleep and health with recommendations for medical surveillance and screening. Occup Environ Med. 1990;5:273–99.
Folkard S, Minors DS, Waterhouse JM. Chronobiology and shift work: current issues and trends. Chronobiologia. 1985;12:31–54.
Minors DS, Scott AR, Waterhouse JM. Circadian arrhythmia: shift-work, travel and health. Occup Environ Med. 1986;36:39–44.
Tepas DI, Carvalhais AB. Sleep patterns of shiftworkers. Occup Med. 1990;5:199–208.
Pilcher JJ, Lambert BJ, Huffcutt AI. Differential effects of permanent and rotating shifts on self-report sleep length: a meta-analytic review. Sleep. 2000;23:155–63.
Kitamura T, Onishi K, Dohi T, Okinaka T, Isaka N, Nakano T. Circadian rhythm of blood pressure is transformed from a dipper to a non-dipper pattern in shift workers with hypertension. J Hum Hypertension. 2002;16:193–7.
Campbell TS, Key BL, Ireland AD, Bacon SL, Ditto B. Early socioeconomic status is associated with adult nighttime blood pressure dipping. Psychosom Med. 2008;70:276–81.
Sherwood A, Steffen PR, Blumenthal JA, Kuhn C, Hinderliter AL. Nighttime blood pressure dipping: the role of the sympathetic nervous system. Am J Hypertens. 2002;15:111–8.
Acknowledgements
The authors gratefully acknowledge the support from the Center for Advanced Study of Language, University of Maryland, College Park, Maryland, USA. We also thank our research staff, graduate students, and undergraduate students at Clemson University for their assistance in data gathering for the study and data management. These individuals include Jesse Allen, J. Adam Beeco, Tracy Lindquist, Bridget McConnell, Eric McKibben, Joe Mulvihill, Kristina O’Connell, Tyler Pierce, Ginger Pottorff, Susan Redmond, Hilary Schoon, Colin Shive, Sarah Spainhour, Rebekkah Wills, Cassandra Wright, and Mark Zajack.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McCubbin, J.A., Pilcher, J.J. & Moore, D.D. Blood Pressure Increases During a Simulated Night Shift in Persons at Risk for Hypertension. Int.J. Behav. Med. 17, 314–320 (2010). https://doi.org/10.1007/s12529-010-9117-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-010-9117-6