Abstract
Background
The increasing population of diabetes mellitus in adolescent girls and women of childbearing age contributes to a large number of pregnancies with maternal pregestational diabetes mellitus. Congenital heart diseases are a common adverse outcome in mothers with pregestational diabetes mellitus. However, there is little systematic information between maternal pregestational diabetes mellitus and congenital heart diseases in the offspring.
Data sources
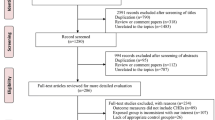
Literature selection was performed in PubMed. One hundred and seven papers were cited in our review, including 36 clinical studies, 26 experimental studies, 31 reviews, eight meta-analysis articles, and six of other types.
Results
Maternal pregestational diabetes mellitus poses a high risk of congenital heart diseases in the offspring and causes variety of phenotypes of congenital heart diseases. Factors such as persistent maternal hyperglycemia, oxidative stress, polymorphism of uncoupling protein 2, polymorphism of adiponectin gene, Notch 1 pathway, Nkx2.5 disorders, dysregulation of the hypoxia-inducible factor 1, and viral etiologies are associated with the occurrence of congenital heart diseases in the offspring of mothers with pregestational diabetes mellitus. Treatment options including blood sugar-reducing, anti-oxidative stress drug supplements and exercise can help to prevent maternal pregestational diabetes mellitus from inducing congenital heart diseases.
Conclusions
Our review contributes to a better understanding of the association between maternal pregestational diabetes mellitus and congenital heart diseases in the offspring and to a profound thought of the mechanism, preventive and therapeutic measurements of congenital heart diseases caused by maternal pregestational diabetes mellitus.

Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article.
References
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843.
Zimmet PZ, Magliano DJ, Herman WH, Shaw JE. Diabetes: a 21st century challenge. Lancet Diabetes Endocrinol. 2014;2:56–64.
Mayer-Davis EJ, Dabelea D, Lawrence JM. Incidence trends of type 1 and type 2 diabetes among youths, 2002–2012. N Engl J Med. 2017;377:301.
Menke A, Casagrande S, Cowie CC. Contributions of A1c, fasting plasma glucose, and 2-hour plasma glucose to prediabetes prevalence: NHANES 2011–2014. Ann Epidemiol. 2018;28:681-5.e2.
Andes LJ, Cheng YJ, Rolka DB, Gregg EW, Imperatore G. Prevalence of prediabetes among adolescents and young adults in the United States, 2005–2016. JAMA Pediatr. 2020;174:e194498.
Rughani A, Friedman JE, Tryggestad JB. Type 2 diabetes in youth: the role of early life exposures. Curr Diab Rep. 2020;20:45.
Chivese T, Werfalli MM, Magodoro I, Chinhoyi RL, Kengne AP, Norris SA, et al. Prevalence of type 2 diabetes mellitus in women of childbearing age in Africa during 2000–2016: a systematic review and meta-analysis. BMJ Open. 2019;9:e024345.
Peters TM, Brazeau AS. Exercise in pregnant women with diabetes. Curr Diab Rep. 2019;19:80.
Rezai S, LoBue S, Henderson CE. Diabetes prevention: reproductive age women affected by insulin resistance. Womens Health (Lond). 2016;12:427–32.
Arendt LH, Pedersen LH, Pedersen L, Ovesen PG, Henriksen TB, Lindhard MS, et al. Glycemic control in pregnancies complicated by pre-existing diabetes mellitus and congenital malformations: a Danish population-based study. Clin Epidemiol. 2021;13:615–26.
Eidem I, Stene LC, Henriksen T, Hanssen KF, Vangen S, Vollset SE, et al. Congenital anomalies in newborns of women with type 1 diabetes: nationwide population-based study in Norway, 1999–2004. Acta Obstet Gynecol Scand. 2010;89:1403–11.
Zegkos T, Ntiloudi D, Giannakoulas G. Parental alcohol exposure and congenital heart diseases in offspring: a causal link with controversial evidence. Eur J Prev Cardiol. 2020;27:407–9.
van der Linde D, Konings EE, Slager MA, Witsenburg M, Helbing WA, Takkenberg JJ, et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol. 2011;58:2241–7.
Chen Z, Li S, Guo L, Peng X, Liu Y. Prenatal alcohol exposure induced congenital heart diseases: from bench to bedside. Birth Defects Res. 2021;113:521–34.
Vincent F, Ternacle J, Denimal T, Shen M, Redfors B, Delhaye C, et al. Transcatheter aortic valve replacement in bicuspid aortic valve stenosis. Circulation. 2021;143:1043–61.
Engineer A, Saiyin T, Greco ER, Feng Q. Say NO to ROS: their roles in embryonic heart development and pathogenesis of congenital heart defects in maternal diabetes. Antioxidants (Basel). 2019;8:436.
Faraoni D, Nasr VG, DiNardo JA. Overall hospital cost estimates in children with congenital heart disease: analysis of the 2012 kid’s inpatient database. Pediatr Cardiol. 2016;37:37–43.
Bhatt AB, Foster E, Kuehl K, Alpert J, Brabeck S, Crumb S, et al. Congenital heart disease in the older adult: a scientific statement from the American heart association. Circulation. 2015;131:1884–931.
Ntiloudi D, Zegkos T, Bazmpani MA, Parcharidou D, Panagiotidis T, Hadjimiltiades S, et al. Pregnancy outcome in women with congenital heart disease: a single-center experience. Hellenic J Cardiol. 2018;59:155–9.
Ntiloudi D, Zegkos T, Koutsakis A, Giannakoulas G, Karvounis H. Pregnancy in patients with congenital heart disease: a contemporary challenge. Cardiol Rev. 2017;25:326–30.
Blue GM, Kirk EP, Sholler GF, Harvey RP, Winlaw DS. Congenital heart disease: current knowledge about causes and inheritance. Med J Aust. 2012;197:155–9.
Fung A, Manlhiot C, Naik S, Rosenberg H, Smythe J, Lougheed J, et al. Impact of prenatal risk factors on congenital heart disease in the current era. J Am Heart Assoc. 2013;2:e000064.
Catalano PM, Tyzbir ED, Roman NM, Amini SB, Sims EA. Longitudinal changes in insulin release and insulin resistance in nonobese pregnant women. Am J Obstet Gynecol. 1991;165:1667–72.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2005;28(Suppl 1):S37-42.
Mills JL, Baker L, Goldman AS. Malformations in infants of diabetic mothers occur before the seventh gestational week Implications for treatment. Diabetes. 1979;28:292–3.
Ejdesjo A, Wentzel P, Eriksson UJ. Influence of maternal metabolism and parental genetics on fetal maldevelopment in diabetic rat pregnancy. Am J Physiol Endocrinol Metab. 2012;302:E1198–209.
Hoang TT, Marengo LK, Mitchell LE, Canfield MA, Agopian AJ. Original findings and updated meta-analysis for the association between maternal diabetes and risk for congenital heart disease phenotypes. Am J Epidemiol. 2017;186:118–28.
Aberg A, Westbom L, Källén B. Congenital malformations among infants whose mothers had gestational diabetes or preexisting diabetes. Early Hum Dev. 2001;61:85–95.
Sylva M, van den Hoff MJ, Moorman AF. Development of the human heart. Am J Med Genet A. 2014;164A:1347–71.
Brade T, Pane LS, Moretti A, Chien KR, Laugwitz KL. Embryonic heart progenitors and cardiogenesis. Cold Spring Harb Perspect Med. 2013;3:a013847.
Buckingham M, Meilhac S, Zaffran S. Building the mammalian heart from two sources of myocardial cells. Nat Rev Genet. 2005;6:826–35.
Buijtendijk MFJ, Barnett P, van den Hoff MJB. Development of the human heart. Am J Med Genet C Semin Med Genet. 2020;184:7–22.
Dhanantwari P, Lee E, Krishnan A, Samtani R, Yamada S, Anderson S, et al. Human cardiac development in the first trimester: a high-resolution magnetic resonance imaging and episcopic fluorescence image capture atlas. Circulation. 2009;120:343–51.
Eriksen NB, Damm P, Mathiesen ER, Ringholm L. The prevalence of congenital malformations is still higher in pregnant women with pregestational diabetes despite near-normal HbA1c: a literature review. J Matern Fetal Neonatal Med. 2019;32:1225–9.
Liu S, Joseph KS, Lisonkova S, Rouleau J, Van den Hof M, Sauve R, et al. Association between maternal chronic conditions and congenital heart defects: a population-based cohort study. Circulation. 2013;128:583–9.
Øyen N, Diaz LJ, Leirgul E, Boyd HA, Priest J, Mathiesen ER, et al. Prepregnancy diabetes and offspring risk of congenital heart disease: a nationwide cohort study. Circulation. 2016;133:2243–53.
Wang H, Wender-Ozegowska E, Garne E, Morgan M, Loane M, Morris JK, et al. Insulin analogues use in pregnancy among women with pregestational diabetes mellitus and risk of congenital anomaly: a retrospective population-based cohort study. BMJ Open. 2018;8:e014972.
Yu Y, Arah OA, Liew Z, Cnattingius S, Olsen J, Sorensen HT, et al. Maternal diabetes during pregnancy and early onset of cardiovascular disease in offspring: population based cohort study with 40 years of follow-up. BMJ. 2019;367:l6398.
Luo L, Zhang S, Wang T, Diao J, Li J, Li Y, et al. Associations of maternal diabetes mellitus and adiponectin gene polymorphisms with congenital heart disease in offspring: a case-control study. Medicine (Baltimore). 2021;100:e24672.
Dervisoglu P, Kosecik M, Kumbasar S. Effects of gestational and pregestational diabetes mellitus on the foetal heart: a cross-sectional study. J Obstet Gynaecol. 2018;38:408–12.
Pavlinkova G, Salbaum JM, Kappen C. Maternal diabetes alters transcriptional programs in the developing embryo. BMC Genomics. 2009;10:274.
Culshaw LH, Savery D, Greene NDE, Copp AJ. Mouse whole embryo culture: evaluating the requirement for rat serum as culture medium. Birth Defects Res. 2019;111:1165–77.
Roest PA, van Iperen L, Vis S, Wisse LJ, Poelmann RE, Steegers-Theunissen RP, et al. Exposure of neural crest cells to elevated glucose leads to congenital heart defects, an effect that can be prevented by N-acetylcysteine. Birth Defects Res A Clin Mol Teratol. 2007;79:231–5.
Engineer A, Lim YJ, Lu X, Kim MY, Norozi K, Feng Q. Sapropterin reduces coronary artery malformation in offspring of pregestational diabetes mice. Nitric Oxide. 2020;94:9–18.
Saiyin T, Engineer A, Greco ER, Kim MY, Lu X, Jones DL, et al. Maternal voluntary exercise mitigates oxidative stress and incidence of congenital heart defects in pre-gestational diabetes. J Cell Mol Med. 2019;23:5553–65.
Moazzen H, Lu X, Ma NL, Velenosi TJ, Urquhart BL, Wisse LJ, et al. N-acetylcysteine prevents congenital heart defects induced by pregestational diabetes. Cardiovasc Diabetol. 2014;13:46.
Wang F, Reece EA, Yang P. Superoxide dismutase 1 overexpression in mice abolishes maternal diabetes-induced endoplasmic reticulum stress in diabetic embryopathy. Am J Obstet Gynecol. 2013;209:e1-7.
Wu Y, Reece EA, Zhong J, Dong D, Shen WB, Harman CR, et al. Type 2 diabetes mellitus induces congenital heart defects in murine embryos by increasing oxidative stress, endoplasmic reticulum stress, and apoptosis. Am J Obstet Gynecol. 2016;215:e1-10.
Kumar SD, Dheen ST, Tay SS. Maternal diabetes induces congenital heart defects in mice by altering the expression of genes involved in cardiovascular development. Cardiovasc Diabetol. 2007;6:34.
Fahed AC, Gelb BD, Seidman JG, Seidman CE. Genetics of congenital heart disease: the glass half empty. Circ Res. 2013;112:707–20.
Codazzi AC, Ippolito R, Novara C, Tondina E, Cerbo RM, Tzialla C. Hypertrophic cardiomyopathy in infant newborns of diabetic mother: a heterogeneous condition, the importance of anamnesis, physical examination and follow-up. Ital J Pediatr. 2021;47:197.
Bolin EH, Spray BJ, Mourani PM, Porter C, Collins RT 2nd. Mortality among infants of diabetic mothers with hypertrophic cardiomyopathy. J Matern Fetal Neonatal Med. 2022. https://doi.org/10.1080/14767058.2022.2066993.
Corrigan N, Treacy A, Brazil DP, McAuliffe FM. Cardiomyopathy and diastolic dysfunction in the embryo and neonate of a type 1 diabetic mouse model. Reprod Sci. 2013;20:781–90.
Han SS, Wang G, Jin Y, Ma ZL, Jia WJ, Wu X, et al. Investigating the mechanism of hyperglycemia-induced fetal cardiac hypertrophy. PLoS One. 2015;10:e0139141.
Levy PT, Tissot C, Horsberg Eriksen B, Nestaas E, Rogerson S, McNamara PJ, et al. Application of neonatologist performed echocardiography in the assessment and management of neonatal heart failure unrelated to congenital heart disease. Pediatr Res. 2018;84(Suppl 1):78–88.
Gheen KM, Reeves JT. Effect of size of ventricular septal defect and age on pulmonary hemodynamics at sea level. Am J Cardiol. 1995;75:66–70.
Otterstad JE, Nitter-Hauge S, Myhre E. Isolated ventricular septal defect in adults. Clinical and haemodynamic findings. Br Heart J. 1983;50:343–8.
Contractor T, Mandapati R. Arrhythmias in patients with atrial defects. Card Electrophysiol Clin. 2017;9:235–44.
Godt RE, Fogaca RT, Nosek TM. Alterations of myocardial contraction associated with a structural heart defect in embryonic chicks. Adv Exp Med Biol. 1998;453:453–8; discussion 9.
Russell NE, Foley M, Kinsley BT, Firth RG, Coffey M, McAuliffe FM. Effect of pregestational diabetes mellitus on fetal cardiac function and structure. Am J Obstet Gynecol. 2008;199:e1-7.
Russell NE, Higgins MF, Kinsley BF, Foley ME, McAuliffe FM. Heart rate variability in neonates of type 1 diabetic pregnancy. Early Hum Dev. 2016;92:51–5.
Maron BJ. Contemporary insights and strategies for risk stratification and prevention of sudden death in hypertrophic cardiomyopathy. Circulation. 2010;121:445–56.
Alcalai R, Seidman JG, Seidman CE. Genetic basis of hypertrophic cardiomyopathy: from bench to the clinics. J Cardiovasc Electrophysiol. 2008;19:104–10.
Morton SU, Pereira AC, Quiat D, Richter F, Kitaygorodsky A, Hagen J, et al. Genome-wide de novo variants in congenital heart disease are not associated with maternal diabetes or obesity. Circ Genom Precis Med. 2022;15:e003500.
Eriksson UJ, Cederberg J, Wentzel P. Congenital malformations in offspring of diabetic mothers–animal and human studies. Rev Endocr Metab Disord. 2003;4:79–93.
Zhao Z, Reece EA. New concepts in diabetic embryopathy. Clin Lab Med. 2013;33:207–33.
Jin YM, Zhao SZ, Zhang ZL, Chen Y, Cheng X, Chuai M, et al. High glucose level induces cardiovascular dysplasia during early embryo development. Exp Clin Endocrinol Diabetes. 2013;121:448–54.
Liu Y, Feng Q. NOing the heart: role of nitric oxide synthase-3 in heart development. Differentiation. 2012;84:54–61.
Liu Y, Lu X, Xiang FL, Poelmann RE, Gittenberger-de Groot AC, Robbins J, et al. Nitric oxide synthase-3 deficiency results in hypoplastic coronary arteries and postnatal myocardial infarction. Eur Heart J. 2014;35:920–31.
Schmidt TS, McNeill E, Douglas G, Crabtree MJ, Hale AB, Khoo J, et al. Tetrahydrobiopterin supplementation reduces atherosclerosis and vascular inflammation in apolipoprotein E-knockout mice. Clin Sci (Lond). 2010;119:131–42.
Heitzer T, Krohn K, Albers S, Meinertz T. Tetrahydrobiopterin improves endothelium-dependent vasodilation by increasing nitric oxide activity in patients with type II diabetes mellitus. Diabetologia. 2000;43:1435–8.
Cai S, Khoo J, Mussa S, Alp NJ, Channon KM. Endothelial nitric oxide synthase dysfunction in diabetic mice: importance of tetrahydrobiopterin in eNOS dimerisation. Diabetologia. 2005;48:1933–40.
Edgar K, Gardiner TA, van Haperen R, de Crom R, McDonald DM. eNOS overexpression exacerbates vascular closure in the obliterative phase of OIR and increases angiogenic drive in the subsequent proliferative stage. Invest Ophthalmol Vis Sci. 2012;53:6833–50.
Edgar KS, Matesanz N, Gardiner TA, Katusic ZS, McDonald DM. Hyperoxia depletes (6R)-5,6,7,8-tetrahydrobiopterin levels in the neonatal retina: implications for nitric oxide synthase function in retinopathy. Am J Pathol. 2015;185:1769–82.
Koenig SN, Bosse K, Majumdar U, Bonachea EM, Radtke F, Garg V. Endothelial Notch1 is required for proper development of the semilunar valves and cardiac outflow tract. J Am Heart Assoc. 2016;5:e003075.
Kerstjens-Frederikse WS, van de Laar IM, Vos YJ, Verhagen JM, Berger RM, Lichtenbelt KD, et al. Cardiovascular malformations caused by NOTCH1 mutations do not keep left: data on 428 probands with left-sided CHD and their families. Genet Med. 2016;18:914–23.
Basu M, Zhu JY, LaHaye S, Majumdar U, Jiao K, Han Z, et al. Epigenetic mechanisms underlying maternal diabetes-associated risk of congenital heart disease. JCI Insight. 2017;2:e95085.
Terada R, Warren S, Lu JT, Chien KR, Wessels A, Kasahara H. Ablation of Nkx2-5 at mid-embryonic stage results in premature lethality and cardiac malformation. Cardiovasc Res. 2011;91:289–99.
Schott JJ, Benson DW, Basson CT, Pease W, Silberbach GM, Moak JP, et al. Congenital heart disease caused by mutations in the transcription factor NKX2-5. Science. 1998;281:108–11.
Ouyang P, Saarel E, Bai Y, Luo C, Lv Q, Xu Y, et al. A de novo mutation in NKX2.5 associated with atrial septal defects, ventricular noncompaction, syncope and sudden death. Clin Chim Acta. 2011;412:170–5.
Zhao M, Diao J, Huang P, Li J, Li Y, Yang Y, et al. Association of maternal diabetes mellitus and polymorphisms of the NKX2.5 gene in children with congenital heart disease: a single centre-based case-control study. J Diabetes Res. 2020;2020:3854630.
Bohuslavova R, Skvorova L, Sedmera D, Semenza GL, Pavlinkova G. Increased susceptibility of HIF-1alpha heterozygous-null mice to cardiovascular malformations associated with maternal diabetes. J Mol Cell Cardiol. 2013;60:129–41.
Souza BM, Assmann TS, Kliemann LM, Gross JL, Canani LH, Crispim D. The role of uncoupling protein 2 (UCP2) on the development of type 2 diabetes mellitus and its chronic complications. Arq Bras Endocrinol Metabol. 2011;55:239–48.
de Souza BM, Brondani LA, Boucas AP, Sortica DA, Kramer CK, Canani LH, et al. Associations between UCP1 -3826A/G, UCP2 -866G/A, Ala55Val and Ins/Del, and UCP3 -55C/T polymorphisms and susceptibility to type 2 diabetes mellitus: case-control study and meta-analysis. PLoS One. 2013;8:e54259.
Hou G, Jin Y, Liu M, Wang C, Song G. UCP2-866G/A polymorphism is associated with prediabetes and type 2 diabetes. Arch Med Res. 2020;51:556–63.
Xu L, Chen S, Zhan L. Association of uncoupling protein-2 -866G/A and Ala55Val polymorphisms with susceptibility to type 2 diabetes mellitus: a meta-analysis of case-control studies. Medicine (Baltimore). 2021;100:e24464.
Luo L, Huang P, Wang TT, Zhao LJ, Ye ZW, Zhang SM, et al. Association of maternal diabetes mellitus and UCP2 gene polymorphisms with congenital heart disease in offspring: a case-control study. Zhongguo Dang Dai Er Ke Za Zhi. 2020;22:1092–9 (in Chinese).
Takahashi M, Arita Y, Yamagata K, Matsukawa Y, Okutomi K, Horie M, et al. Genomic structure and mutations in adipose-specific gene, adiponectin. Int J Obes Relat Metab Disord. 2000;24:861–8.
Sun P, Liu L, Chen J, Chen Y, Shi L, Imam MU, et al. The polymorphism of rs266729 in adiponectin gene and type 2 diabetes mellitus: a meta-analysis. Medicine (Baltimore). 2017;96:e8745.
Cui M, Gao Y, Zhao Y, Pang H, Chen L, Wang Z, et al. Association between adiponectin gene polymorphism and environmental risk factors of type 2 diabetes mellitus among the Chinese population in Hohhot. Biomed Res Int. 2020;2020:6383906.
Cai Y, Zeng T, Chen L. Association of adiponectin polymorphisms with the risk of diabetic nephropathy in type 2 diabetes: a meta-analysis. J Diabetes. 2015;7:31–40.
Carvajal HG, Brar AK, Eghtesady P. Maternal gut virome in pregestational diabetes-possible cause of congenital heart disease? Open Forum Infect Dis. 2020;7:ofaa013.
Sharma V, Goessling LS, Brar AK, Joshi CS, Mysorekar IU, Eghtesady P. Coxsackievirus B3 infection early in pregnancy induces congenital heart defects through suppression of fetal cardiomyocyte proliferation. J Am Heart Assoc. 2021;10:e017995.
Wook Kim K, Allen DW, Briese T, Couper JJ, Barry SC, Colman PG, et al. Distinct gut virome profile of pregnant women with type 1 diabetes in the ENDIA study. Open Forum Infect Dis. 2019;6:ofz025.
Lin SF, Kuo CF, Chiou MJ, Chang SH. Maternal and fetal outcomes of pregnant women with type 1 diabetes, a national population study. Oncotarget. 2017;8:80679–87.
Wahabi HA, Alzeidan RA, Bawazeer GA, Alansari LA, Esmaeil SA. Preconception care for diabetic women for improving maternal and fetal outcomes: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2010;10:63.
Bishop KC, Harris BS, Boyd BK, Reiff ES, Brown L, Kuller JA. Pharmacologic treatment of diabetes in pregnancy. Obstet Gynecol Surv. 2019;74:289–97.
Bergel R, Hadar E, Toledano Y, Hod M. Pharmacological management of gestational diabetes mellitus. Curr Diab Rep. 2016;16:118.
Toledano Y, Hadar E, Hod M. Safety of insulin analogues as compared with human insulin in pregnancy. Expert Opin Drug Saf. 2016;15:963–73.
Lv S, Wang J, Xu Y. Safety of insulin analogs during pregnancy: a meta-analysis. Arch Gynecol Obstet. 2015;292:749–56.
Wyatt JW, Frias JL, Hoyme HE, Jovanovic L, Kaaja R, Brown F, et al. Congenital anomaly rate in offspring of mothers with diabetes treated with insulin lispro during pregnancy. Diabet Med. 2005;22:803–7.
Rowan JA, Hague WM, Gao W, Battin MR, Moore MP, MiG trial investigators. Metformin versus insulin for the treatment of gestational diabetes. N Engl J Med. 2008;358:2003–15.
Guo L, Ma J, Tang J, Hu D, Zhang W, Zhao X. Comparative efficacy and safety of metformin, glyburide, and insulin in treating gestational diabetes mellitus: a meta-analysis. J Diabetes Res. 2019;2019:9804708.
Kusuyama J, Alves-Wagner AB, Makarewicz NS, Goodyear LJ. Effects of maternal and paternal exercise on offspring metabolism. Nat Metab. 2020;2:858–72.
Zheng J, Zhou LY, Xiao XH. Maternal exercise and its beneficial effects on glucose metabolism in offspring. Chin Med J (Engl). 2020;133:863–7.
Barakat R, Pelaez M, Cordero Y, Perales M, Lopez C, Coteron J, et al. Exercise during pregnancy protects against hypertension and macrosomia: randomized clinical trial. Am J Obstet Gynecol. 2016;214:e1-8.
May LE, Scholtz SA, Suminski R, Gustafson KM. Aerobic exercise during pregnancy influences infant heart rate variability at one month of age. Early Hum Dev. 2014;90:33–8.
Acknowledgements
We thank Yan-Qiu Chen for her expert assistance with the image processing technology.
Funding
This work was supported by Sichuan Vocational College of Health and Rehabilitation (No. CWKY-2020Z-02), the Department of Science and Technology of Sichuan Province (No. 2019YJ0079), and the National Natural Science Foundation of China (No. 81900283).
Author information
Authors and Affiliations
Contributions
CZY contributed to conceptualization and writing of the original draft. MSF and GLH contributed to validation. QJ and YLX contributed to software. LY contributed to reviewing and editing, and funding acquisition. All authors have made substantial contributions to the conception and design of the study, drafting the article, or revising it critically for important intellectual content. All authors have provided approval for the final version to be submitted and published. Each author has agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Conflict of interest
No financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, ZY., Mao, SF., Guo, LH. et al. Effect of maternal pregestational diabetes mellitus on congenital heart diseases. World J Pediatr 19, 303–314 (2023). https://doi.org/10.1007/s12519-022-00582-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-022-00582-w