Abstract
The ongoing coronavirus disease 2019 (COVID-19) crisis is having a large impact on acute and chronic cardiac care. Due to public health measures and the reorganisation of outpatient cardiac care, traditional centre-based cardiac rehabilitation is currently almost impossible. In addition, public health measures are having a potentially negative impact on lifestyle behaviour and general well-being. Therefore, the Working Group of Cardiovascular Prevention and Rehabilitation of the Dutch Society of Cardiology has formulated practical recommendations for the provision of cardiac rehabilitation during the COVID-19 pandemic, by using telerehabilitation programmes without face-to-face contact based on current guidelines supplemented with new insights and experiences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the coronavirus disease 2019 (COVID-19) pandemic many elective and outpatient healthcare activities have been cancelled or postponed. Also, a decline in admissions due to cardiac disease has been observed [1]. In many Dutch hospitals and specialised rehabilitation clinics, cardiac rehabilitation (CR) programmes have been shut down partially or even completely. In particular, group-based exercise training interventions and exercise testing are hardly possible. In addition, the public health measures implemented during the COVID-19 pandemic, above all quarantine and isolation, have been shown to be associated with anxiety, anger and stress, which is associated with unhealthy lifestyle behaviour, including a reduction in physical activity and an unhealthy diet [2]. Therefore, there is an urgent need for upscaling and reorganisation of CR and secondary prevention services. Recently, the Working Group of Cardiovascular Prevention and Rehabilitation of the Dutch Society of Cardiology has formulated practical recommendations for CR during the COVID-19 pandemic. These recommendations are partly based on a recent statement from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology [3], supplemented with insights from the recently published Dutch Telerehabilitation guidelines [4] and practical experiences from the largest Dutch CR centres. The importance of continuing the delivery of (cardiac) rehabilitation during the COVID-19 pandemic by means of telerehabilitation programmes without face-to-face contact is emphasised by the prompt reimbursement of these programmes by the Netherlands Health Institute (NZa) and with support from the Netherlands Health Institute (ZiN).
General recommendations
-
Support acute cardiac wards in providing summarised but highlighted important information/recommendations on secondary prevention (not forgetting physical activity and mental impact) before hospital discharge.
-
In the case of shortened CR programmes, concentrate efforts on the main core components (i.e. lifestyle risk management, psychosocial support, medical advice, education) with an individualised approach based on psychological symptoms, residual cardiac risk and lifestyle assessment.
-
Replace face-to-face sessions by remote assessment and monitoring/guiding, according to local equipment and expertise (telephone, text messaging, e‑mails, video consultations, web-based platforms and applications).
-
Perform patient assessment and risk stratification with an exercise test whenever possible. If not possible, use other tools to assess the cardiovascular risk and physical fitness in order to provide personalised exercise advice and to guide telerehabilitation (see Tab. 1).
-
For COVID-19-positive patients, postpone the exercise programme if fever, symptoms or other signs of COVID-19 infection are present [3]. Evaluate exercise resumption on an individual basis. In general, in patients with light-to-moderate symptoms, gradually restart the exercise programme after a fever-free period of 1 week and a symptom-free period of 48 h. Whenever possible, do not postpone all other CR components but provide them remotely (see Tab. 1).
-
For general safety and hygiene measures take into account the recommendations of the Dutch National Institute for Public Health and the Environment (Rijksinstituut voor Volksgezondheid en Milieu,RIVM) and the Dutch Federation of Medical Specialists (Federatie Medisch Specialisten, FMS) [5, 6].
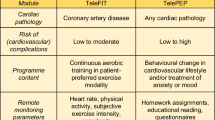
Specific recommendations are presented in Tab. 1.
References
De Rosa S, Spaccarotella C, Basso C, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41(22):2083–8.
Mattioli AV, Ballerini Puviani M, Nasi M, et al. COVID-19 pandemic: the effects of quarantine on cardiovascular risk. Eur J Clin Nutr. 2020;74:852–5.
Committee for Cardiovascular Prevention and Cardiac Rehabilitation of the Netherlands Society of Cardiology, Landelijk Multidisciplinair Overleg Hartrevalidatie. Addendum telerevalidatie in multidisciplinaire richtlijn hartrevalidatie. 2018. https://www.nvvc.nl/Kwaliteit/Richtlijnen/Addendum%20richtlijn%20hartrevalidatie%20-1-.pdf.
https://www.rivm.nl/coronavirus-covid-19/professionals/buiten-ziekenhuis/veelgestelde-vragen.
https://www.demedischspecialist.nl/nieuws/leidraad-persoonlijke-bescherming-de-poliklinische-setting.
Netherlands Society of Cardiology/Netherlands Heart Foundation. Multidisciplinary guidelines for cardiac rehabilitation. 2011. https://www.nvvc.nl/Richtlijnen/Multidisciplinaire%20Richtlijn%20Hartrevalidatie%202011%2023052011.pdf.
Committee for Cardiovascular Prevention and Cardiac Rehabilitation of the Netherlands Society of Cardiology, Landelijk Multidisciplinair Overleg Hartrevalidatie. Beslisboom Poliklinische Indicatiestelling Hartrevalidatie 2012. 2012. https://www.nvvc.nl/Richtlijnen/Beslisboom%20Hartrevalidatie%202012%20-website.pdf.
Nes BM, et al. Estimating VO2peak from a nonexercise prediction model: the HUNT Study, Norway. Med Sci Sports Exerc. 2011;43(11):2024–30.
Bohannon RW, Crouch RH. Two-minute step test of exercise capacity: systematic review of procedures, performance, and clinimetric properties. J Geriatr Phys Ther. 2019;42(2):105–12.
Committee for Cardiovascular Prevention and Cardiac Rehabilitation of the Netherlands Society of Cardiology, Landelijk Multidisciplinair Overleg Hartrevalidatie. NVVC Practice guidelines for cardiac rehabilitation. 2011. https://www.nvvc.nl/Richtlijnen/Geautoriseerde%20NVVC%20Praktijkrichtlijn%20Hartrevalidatie%20maart%202011.pdf.
Ambrosetti M, Abreu A, Corrà U, et al. Secondary prevention through comprehensive cardiovascular rehabilitation: from knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2020; https://doi.org/10.1177/2047487320913379.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
H.M.C. Kemps, R.W.M. Brouwers, M.J. Cramer,H.T. Jorstad, E.P. de Kluiver, R.A. Kraaijenhagen, P.M.J.C. Kuijpers, M.R. van der Linde, E. de Melker, S.F. Rodrigo, R.F. Spee, M. Sunamura, T. Vromen and M.E. Wittekoek declare that they have no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kemps, H.M.C., Brouwers, R.W.M., Cramer, M.J. et al. Recommendations on how to provide cardiac rehabilitation services during the COVID-19 pandemic. Neth Heart J 28, 387–390 (2020). https://doi.org/10.1007/s12471-020-01474-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12471-020-01474-2