Abstract
Radioligand therapy (RLT) with lutetium (177Lu) oxodotreotide is an approved therapy in combination with somatostatin analogues (SSAs) for patients with advanced, well-differentiated G1–G2, gastro-entero-pancreatic neuroendocrine tumours (GEP-NETs) that progress on SSAs. We conducted a series of round table meetings throughout Italy to identify issues related to RLT delivery to patients with GEP-NETs. Four key issues were identified: (1) the proper definition of tumour progression prior to RLT initiation; (2) the impact of RLT in patients with bone metastases and/or high hepatic tumour burden; (3) the optimal follow-up protocol after RLT; and (4) organisational issues related to RLT use and managerial implications. This article reviews the literature relating to the aforementioned issues and makes recommendations based on available evidence and Italian NET experts’ opinions. In particular, the group recommends the development of a diagnostic–therapeutic care pathway (DTCP) for patients undergoing RLT which provides systematic guidance but can still be individualised for each patient’s clinical and psychosocial needs. A DTCP may clarify the diagnostic, therapeutic and post-treatment monitoring process, and improve communication and the coordination of care between hub and spoke centres. The DTCP may also contribute to changes in the care process related to the 2013/59/EURATOM Directive and to the definition of costs when planning for future or updated reimbursement of RLT in Italy.
Similar content being viewed by others
Radioligand therapy [RLT; e.g. lutetium (177Lu) oxodotreotide (Lutathera®)] is an established treatment option for progressive, well-differentiated, grade 1–2 gastro-entero-pancreatic neuroendocrine tumours (GEP-NETs). | |
In clinical practice, however, RLT is underutilised, and the optimal sequence of treatment is undefined; successful treatment of GEP-NETs requires clear practical guidance on managing the patient therapeutic journey and optimisation of RLT. | |
In this article, we analyse four key areas where (in the opinion of Italian experts) practical clarification of RLT guidelines is needed, including: (1) defining tumour progression prior to RLT; (2) RLT impact on bone metastases and/or high hepatic tumour burden; (3) optimal protocols for monitoring tumour response; and (4) organisational issues related to RLT use. | |
The development of a diagnostic-therapeutic care pathway (DTCP) is recommended in order to provide systematic guidance being personalised according to clinical and psychosocial needs of each patient. | |
A DTCP may clarify the diagnostic, therapeutic and post-treatment monitoring process and improve the coordination of care in patients with GEP-NETs. |
Introduction
Radioligand therapy (RLT), also known as peptide radionuclide receptor therapy (PRRT), is now an established treatment option for progressive, well-differentiated, grade 1–2 (G1–G2) gastro-entero-pancreatic neuroendocrine tumours (GEP-NETs) [1]. RLT use is also gradually increasing as a second-line treatment for patients with GEP-NETs progressing on or after treatment with somatostatin analogues (SSAs) [2]. Lutetium (177Lu) oxodotreotide (Lutathera®) is the first authorised radiopharmaceutical for RLT in the treatment of GEP-NETs that entered the market, representing an important step forward in the management of patients with these types of tumours. In 2017, this radiopharmaceutical was designated as an orphan medicine and indicated for the treatment of unresectable locally advanced or metastatic, progressive, well-differentiated (G1–G2), somatostatin receptor (SSTR)-positive GEP-NETs in adults [3]. This indication is predominantly based on data from the phase III NETTER-1 clinical trial, in which lutetium (177Lu) oxodotreotide (also referred to as 177Lu- DOTA0-Tyr3–octreotate) plus label-dose long-acting repeatable (LAR) octreotide were compared with high-dose octreotide LAR [60 mg every 4 weeks (q4w)] in 229 patients with advanced, SSTR-positive midgut NETs who had progressed on octreotide LAR 20–30 mg every 3–4 weeks within a time frame of up to 3 years [4]. The estimated rate of progression-free survival (PFS) at month 20 was 65.2% [95% confidence interval (CI), 50.0–76.8] with lutetium (177Lu) oxodotreotide and 10.8% (95% CI 3.5–23.0) with high-dose octreotide LAR [4]. The risk of disease progression or death was 79.0% lower in the group receiving lutetium (177Lu) oxodotreotide plus octreotide LAR at standard dose compared with the control group receiving high-dose octreotide LAR [4]. The extension to treat all GEP-NETs was also based on data from a previously published patient series [5,6,7].
While these results indicate a clinically relevant improvement of PFS with lutetium (177Lu) oxodotreotide compared with high-dose octreotide LAR, RLT is underutilised in clinical practice [6]. In addition, several therapeutic options are available for patients with GEP-NET and the optimal sequence of these treatments has yet to be clearly defined [8]. In this setting, several factors need to be taken into account for decision-making, including the treatment goal, tumour characteristics (i.e. SSTR status, functioning/non-functioning tumour, primary site, tumour morphology and grading), patient profile (i.e. performance status, comorbidities and quality of life) and treatment characteristics (i.e. safety profile and schedule) [1, 8].
These issues make adopting this promising therapy into clinical practice a major challenge that requires extensive coordination of different specialists within a NET-dedicated multidisciplinary team (MDT). The challenge is compounded by the fact that clinical outcomes depend on an appropriately designed and adequately managed patient therapeutic journey, including accurate disease characterisation, identification of the best treatment candidates, and appropriate therapy administration and monitoring. Therefore, physicians wishing to optimise RLT need practical guidance on implementing this treatment in clinical practice.
This article aims to critically analyse four key areas where (in the opinion of Italian experts) practical interpretation and clarification of guideline recommendations related to RLT are needed. These four areas are: (1) the definition of tumour progression prior to RLT initiation; (2) the impact of RLT in patients with bone metastases and/or high hepatic tumour burden; (3) the optimal follow-up protocol to monitor tumour response to RLT; and (4) organisational issues related to RLT use and managerial implications.
Materials and Methods
To identify the most relevant issues related to RLT in Italy and formulate recommendations, the authors (Scientific Committee) met and convened a series of 24 local round table meetings with other oncology practitioners throughout Italy between 12 May 2021 and 22 February 2022 (see ‘Round table discussion’ in Electronic Supplementary Material).
Before carrying out these round table meetings, the Scientific Committee conducted various systematic literature searches [9] using the topics and keywords identified by working groups at a primary meeting (see below). Relevant publications identified via searches were presented at a second meeting to guide scientific discussions. Moreover, in May 2021, an initial survey on the multidisciplinary management of patients with GEP-NETs in Italy was administered to 90 physicians who treat such patients (see ‘Survey Results’ and ‘Supplementary Fig. 1’ in Electronic Supplementary Material).
Literature search results were presented using a narrative approach to discuss the available evidence and report the authors’ viewpoints. Arguments and topics of interest for the discussion were defined using PICO, i.e. patient/population (e.g. patients with progressing GEP-NETs, bone metastases and/or high hepatic tumour burden), intervention (RLT), comparators (SSAs), and outcomes (efficacy, safety, optimal follow-up procedures, economic burden, organisational issues and managerial implications) [10].
The literature search was conducted in April 2021 on PubMed and Scopus using keywords generated from collegial discussions and brainstorming processes [11], during the first round table meeting. Titles and/or abstracts containing the following keywords were included in the search: GEP-net patient treatment, GEP-net tumour progression, GEP-net bone metastases, high hepatic tumour burden, RLT, RLT initiation, RLT use, SSA initiation, SSA use, efficacy outcome, safety outcome, GEP-net follow-up protocols, RLT economic aspect, RLT organisational issue, GEP-net organisational issue.
The article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Definition of Baseline Tumour Progression
According to the United States Food and Drug Administration and European Medicine Agency guidelines, tumour progression must be identified before initiating lutetium (177Lu) oxodotreotide treatment [3]. However, these guidelines do not provide a specific definition of tumour progression; it is still unclear if progression should be based on imaging and/or clinical behaviour and/or an increase in circulating biomarkers. Notably, recommendations on imaging in patients with NETs failed to reach a consensus on the type of imaging to be used to monitor tumour response [12].
In the NETTER-1 study [4], tumour progression was defined according to the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1 criteria [13], using either computed tomography (CT) or magnetic resonance imaging (MRI) for monitoring treatment response (Table 1). Other major phase III studies of various SSAs used the World Health Organization (WHO) criteria [14] (e.g. the PROMID study with octreotide LAR [15)] or RECIST version 1.0 criteria [16] (e.g. CLARINET study with lanreotide autogel [17)] to assess tumour progression during treatment (Table 1). Despite the well-established role of RECIST in clinical research, these criteria have drawbacks that limit their application in clinical practice. For example, they do not guide the choice of target lesions or imaging technique and identifying reliable extrahepatic target lesions in GEP-NETs can be difficult [18]. In addition, the usually low proliferation rate in GEP-NETs means that the magnitude of change defined by RECIST criteria may not reflect clinically meaningful changes in tumour size or density [19, 20].
In daily clinical practice, progressive disease (PD) may follow different criteria than those utilised for pivotal clinical trials. Specifically, PD can be determined by evidence of tumour progression via imaging, even when the classical WHO/RECIST criteria are not met. Moreover, tumour progression can be considered a composite concept that includes hybrid imaging-based characterisation and clinical assessment; some patients may have radiologically stable tumours, yet simultaneously show clinical/biochemical signs of PD. Such non-radiological signs of progression can include worsening of a clinical/biochemical syndrome and increases in the levels of a circulating biomarker (e.g. chromogranin A [CgA)].
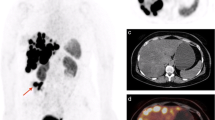
In the case of GEP-NETs, the recommended functional imaging modality is 68gallium (68Ga)-DOTA-SSA-positron emission tomography (PET) [12]. However, with respect to functional imaging, there are no clear criteria defining PD [21], and there is no standardisation in the interpretation of, for example, the appearance of new lesions or an increase in maximum standardised uptake value (SUVmax). The increase in lesion uptake from 68Ga-DOTA-SSA-PET indicates an increase in SSTR expression and lesion uptake should be higher than the background liver uptake [21]. However, there is no evidence that an increase in SUVmax with 68Ga-DOTA-SSA-PET is a sign of PD, since there is a lack of standardised imaging protocols, and, therefore, this parameter should not be interpreted as PD. On the other hand, functional imaging assessed with 18fluorodeoxyglucose (18FDG)-PET provides different information, since the presence of a ‘new lesion’ on PET imaging in patients with radiographically stable disease and without clinical/biochemical signs of PD might be sufficient to consider that the disease is progressing.
The lack of strict criteria for defining PD allows physicians the flexibility to determine patient eligibility for RLT using a broad clinical context. We recommend that a NET-dedicated MDT determines the identification of PD prior to RLT. The MDT should consider the presentation on complete morphological imaging (i.e. CT or MRI), the patient’s clinical and biochemical profile, and/or functional imaging results. MDTs play a key role in adjudicating ambiguous evidence of PD in, for example, patients with ‘slow’ radiological PD, who may benefit from closer monitoring and adjustment of their SSA treatment schedule rather than initiating RLT.
If the patient is a potential candidate for RLT, blood tests, including haematology and renal and hepatic function, should be conducted at least once 2–4 weeks prior to initiating RLT (Table 2) [21], as well as shortly before administration [3]. The results of these tests should be used to guide decisions about eligibility and eventually to adjust the administered doses.
RLT in Patients with High Bone and/or Hepatic Tumour Burden
Currently, there is a lack of clarity regarding the role and value of RLT in patients with high bone and/or hepatic tumour burden. Therefore, clinical criteria are needed to define which of these patients may benefit from RLT.
Bone Metastases
GEP-NETs are much less likely to metastasise to bone than to liver [22]. Nevertheless, patients with bone metastases have worse clinical outcomes and shorter PFS and overall survival (OS) compared with patients without bone metastases [23]. Regarding RLT, bone metastases raise concerns about radioligand penetration into bone and the risk of treatment-related myelosuppression caused by the accumulation of radioactivity in skeletal segments rich in bone marrow.
In clinical practice, the superior sensitivity and specificity of 68Ga-DOTA-SSA-PET/CT compared with conventional imaging and radiological evaluation enable earlier identification of bone metastases [24]. Some MRI techniques can be considered in addition to 68Ga-DOTA-SSA-PET/CT.
From the discussions at the round table meetings, two major concerns, related to RLT use in patients with bone metastases, were apparent: (1) the effective ability of the radioligand to penetrate bone and reach metastatic sites; and (2) the potential increased risks of myelotoxicity and haematological adverse events, after RLT administration, in patients with significant skeletal metastasis. Generally, RLT appears effective in patients with bone metastases, and treated patients typically show a good prognosis and a low probability of experiencing skeletal events [25, 26]. Researchers from Germany reported a median OS of 51.0 months in patients treated with RLT with GEP-NETs and bone metastases, and a median OS of 56.0 months in those with a measurable bone response [25, 26]. Factors associated with a significantly worse prognosis were neuron-specific enolase (NSE) > 15.0 ng/mL, Ki67 index > 10.0% at baseline and blood CgA > 600.0 ng/mL. In contrast, age, performance status and the number of lesions were not significant predictors [25, 26]. Many patients with bone metastases or bone marrow involvement experienced symptomatic improvement after RLT, including complete or partial bone pain relief, performance status improvement and better self-reported quality of life [25, 26]. Overall, preliminary data indicate that RLT can be effective even in patients with diffuse bone metastases [27]. The incidence of significant haematological toxicity is generally low (10.2% in the study described above [25)] and reversible, possibly because of the low expression of SSTRs in bone marrow [28]. Among six patients with GEP-NETs and bone marrow involvement who received RLT, the only haematological adverse event was grade 1 anaemia in one patient [29]. The myelotoxicity of RLT seems related to the relative extent of irradiation received by red bone marrow from adjacent organs largely involved by NETs rather than to the presence of bone metastases [30, 31]
In patients with NETs, there is no evidence of RLT-related toxicity in healthy bone tissue. Lutetium (177Lu) oxodotreotide has a beta emission [3], with a mean range penetration in the bone of 0.16 mm, which is lower than most other beta emitters currently used for therapeutic purposes [32, 33]. Regarding a possible effect of RLT on osteoblasts, one expert mentioned that there is no evidence that RLT affects healthy bone (endosteum) but is focused on the bone marrow. Dosimetry does not lead to precise doses to the endosteum, but the dose of 177Lu released to healthy bone is much lower than the dose given by external beam radiotherapy.
Bone metastases are not common in NETs, affecting 4.0–12.0% of patients [24], although their prevalence may be underestimated [23]. However, they represent a negative prognostic factor, usually because they are a marker of more extensive metastatic spread [34]. Based on the abovementioned clinical results in patients with metastatic GEP-NETs [25, 26, 29], RLT is an effective treatment for those with bone metastases. Although some patients may experience haematological toxicity, it is generally manageable through dose interruption or supportive measures [27]. Because of potential issues in accurately imaging bone metastases, we recommend assessing the response to RLT using a combination of clinical, functional and radiological parameters.
Patients with High Hepatic Tumour Burden
The liver is the most common metastatic site in patients with GEP-NETs [22]. Patients with high hepatic tumour burden are likely to benefit from RLT, similarly to patients with low hepatic tumour burden. A post hoc analysis of data from the NETTER-1 study showed that PFS after RLT was similar in patients with a high hepatic tumour burden (i.e. > 50.0% of liver involvement on CT or MRI) as in those with moderate (25.0–50.0%) or low (< 25.0%) hepatic tumour burden; the same pattern was seen in patients with elevated or normal alkaline phosphatase levels at baseline [35]. The rates of grade 3–4 hepatic toxicities were low in all groups in the NETTER-1 post hoc analysis, so no statistical comparison was undertaken; there was, however, no evidence of increased risk of liver enzyme abnormalities in those with greater versus smaller hepatic involvement [35]. A Polish study of 42 patients receiving RLT [39 (93.0%) with liver metastases] reported small but statistically significant reductions in albumin and alanine aminotransferase levels and an increase in bilirubin in the 2 days after each treatment. However, all hepatic parameters stayed within the normal range [36].
Optimal Follow-up Protocol After RLT
While it is important to define the optimal approach to follow-up during and after RLT (in relation to the type and timing of tests), follow-up should also be tailored to each patient’s circumstances because “one size does not fit all”. We believe current guidelines do not offer sufficient guidance for a standardised approach to patient follow-up after RLT.
In the NETTER-1 study, patients were monitored every 2–4 weeks during RLT with tests for haematology, biochemistry and renal function [4]. We recommend defining the strategy for monitoring tumour response to RLT based on the morphological and functional characteristics of the tumour, degree of malignancy and the capabilities of the clinical centre (e.g. availability of imaging modalities and MDTs). Patients undergoing RLT provide blood samples regularly for the detection of adverse reactions [3], so other tests (e.g. urinary 5-hydroxyindoleacetic acid in patients with carcinoid syndrome-associated GEP-NETs) can be undertaken at the same time. Imaging assessment should not be performed during RLT treatment unless PD is suspected. CgA may be a useful adjunct assessment but should not be considered a surrogate marker for defining response.
When developing a strategy for tumour monitoring, it is important to balance the need for early detection of PD against the risks (radiation exposure and use of contrast media) and the costs of monitoring stable patients [19]. Imaging patients with NETs can be extremely complex because of high tumour heterogeneity. Table 3 summarises our recommendations for using CT, MRI and ultrasound in the follow-up of patients with GEP-NETs, based on current recommendations and evidence [37,38,39,40]. PET plays only a marginal role during prolonged follow-up because of the cost. On the other hand, liver ultrasound has an important role, because of its long-term safety during repeated use.
In addition to the type of imaging modality, the timing of imaging assessments must also be considered. In the NETTER-1 study, patients were followed up every 12 weeks after completing the last treatment cycle, starting 2 months after the fourth cycle using CT or MRI [4]. No specific follow-up intervals after RLT are described in the European Society for Medical Oncology guidelines. However, these guidelines do recommend imaging assessments every 3 months for patients with G2 NETs and Ki67 > 5.0% (i.e. candidates for RLT), extending to every 1–2 years over time [1]. Similarly, the Spanish consensus recommendations suggest assessments every 3 months for 2 years when following up patients with metastatic G1–G2 GEP-NETs, then every 6 months if patients are stable [19]. Once PD is detected, these guidelines recommend restarting assessments every 3 months [19]. The European Neuroendocrine Tumour Society (ENETS) recommendations specify different follow-up intervals based on tumour site, size and type (e.g. type 1, 2 and 3 stomach NEC/NETs, gastrinoma or insulinoma); however, in most G1–G2 GEP-NETs, the recommended interval is 3–6 months [41].
Among the existing guidelines, only those by the North American Neuroendocrine Tumor Society (NANETS) and Society of Nuclear Medicine and Molecular Imaging (SNMMI) provide guidance on follow-up after RLT completion (Table 4) [21]. These guidelines recommend laboratory assessments, clinical evaluations, and imaging at specific intervals; however, tumour marker assays should be determined by the patient’s cancer team. Similarly, they note that the follow-up protocol should be modified according to the patient’s clinical presentation, symptoms, or sequelae [21], consistent with our recommendation for tailoring the follow-up schedule according to the patient’s characteristics and the unit’s facilities.
Survival after a diagnosis of well-differentiated GEP-NETs in Italy is high, with 5-year survival rates of 75.0–85.0% for well-differentiated functional or non-functional tumours [42], so follow-up will be lifelong in most patients. We recommend follow-up every 3–6 months for the first 2–3 years and annually thereafter. This follow-up should include clinical assessment, blood tests, imaging (using ultrasound, MRI, and triple-phase CT with contrast for an accurate study of the liver) and endoscopy as indicated. When recurrence or PD is suspected, functional imaging using 68Ga-DOTA-SSA- or 18FDG-PET/CT should be integrated with morphological imaging. Prolonged follow-up has a significant economic impact, with the costs of diagnostic tests, such as PET/CT, making a substantial contribution. Follow-up should be tailored to the individual patient according to the aggressiveness of the patient’s NET, the stage at diagnosis, the site(s) of the tumour and all available prognostic parameters and modified as needed according to any changes in their clinical or personal circumstances.
While survival is the major goal of cancer treatment, it brings its own challenges, including long-term physical and functional treatment effects (which may be particularly relevant in patients who have received radiation), worse quality of life, fatigue, psychological impacts (e.g. anxiety, fear of recurrence, post-traumatic stress disorder and depression), effects on sleep and impact on the patient’s ability to return to work [43,44,45,46]. Since not all centres have sophisticated imaging modalities, some patients must travel to a tertiary centre for assessment, contributing to the economic burden and potentially to their distress. Therefore, follow-up of patients with GEP-NETs must be multifactorial and include not only assessment for recurrence. Some patients appear particularly vulnerable to psychological distress, including elderly patients and those who do not have a spousal partner [43, 47]. Survivorship is not a “one size fits all” experience, with each patient having a different physical and psychological reaction to cancer treatment [48]. This highlights the importance of developing a systematic and comprehensive approach to the follow-up of patients with GEP-NETs after RLT that encompasses all the patient’s needs (i.e. clinical, psychosocial and financial) and ensures effective communication between all stakeholders, including the patient’s primary care team and their family/support network [43, 44]. If possible, the follow-up protocol for each patient should be developed by an MDT.
Organisational Issues
The complexity of the diagnostic–therapeutic care pathway (DTCP), particularly that related to RLT treatment, requires standardised management of each phase, which can optimise both patient access to the treatment and clinical outcomes, as well as maximising the efficiency and potential benefits of overall DTCP management. Multiple biological tests are required to monitor the patient’s condition and adapt the therapeutic protocol as required, including the dose, infusion interval or the number of infusions [3]. Our round table meetings identified several issues related to the organisation and delivery of RLT services, including difficulties in accessing the services needed to define PD at smaller centres (e.g. advanced imaging techniques or NET-dedicated MDTs). Other issues included difficulties in coordinating treatment between different centres, poor recognition of the value of RLT due to a lack of training in peripheral centres, and difficulties in referring patients from smaller centres to RLT centres. We have identified several actions that will help to organise the DTCP better and optimise RLT from a hospital perspective, as well as improve the patient journey and experience.
Organisational Model
RLT delivery in Italy should be based on a “hub-and-spoke” model, where patients are referred from smaller centres (spokes) and receive treatment at high-volume expert centres (hubs). Hubs need to receive feedback on waiting times and their ability to provide services to investigate how closely real-world practice aligns with forecasts made at a regional level. Ideally, there should be an ongoing monitoring process to identify the difficulties in providing services within defined deadlines. Feedback should inform how care can be better delivered and identify performance indicators that can be used to highlight specific needs and barriers.
To optimise the DTCP, training needs to be developed around a core curriculum of skills to address knowledge gaps. While the core curriculum should define key learnings for both hub and spoke centres, the training itself should be tailored to each type of centre to ensure that personnel receive the information that is most relevant for them, specifically based on their knowledge gaps (e.g. referral criteria and post-treatment monitoring at spoke centres versus RLT procedures in hub centres).
There is also a need to define the entire DTCP more comprehensively for patients with GEP-NET who are candidates for RLT. The DTCP should explicitly define the timing and sequence of tasks involved and the clinical team/discipline responsible for each task [49]. This can be performed through specific management tools, such as the Responsible, Accountable, Consulted and Informed (RACI) matrix [50], defining responsibilities in patient management at all stages of the RLT process. The RACI matrix should be aligned with performance indicators identified during the research and monitoring phases and include care quality indicators. These indicators should cover a range of outcomes: clinical (e.g. response and recurrence), organisational (e.g. follow-up visits), managerial (e.g. costs) and patient-related (e.g. quality of life, satisfaction, and perceptions of the treatment experience). Because of disease and patient heterogeneity, a single DTCP is unlikely to be suitable for all patients with GEP-NET, who will need to be stratified and specific pathways developed based on patients’ health and social needs and characteristics. These DTCPs would help clarify the process within a single centre and aid in the organisation/coordination of care between hub and spoke centres. Moreover, they can potentially improve efficiency and optimise the overall clinical pathway from the hospital and the patient’s perspectives.
Furthermore, the proper development of a DTCP for RLT could support the identification of a specific reimbursement tariff devoted to RLT administration. This is important in Italy, where the public healthcare system provides reimbursement based on a single healthcare service, which complicates reimbursement for complex treatment protocols, such as RLT. To achieve this, scientific societies and clinical communities should collaborate to show the policymakers that a DTCP could provide an economic advantage by avoiding the unnecessary repetition of examinations and assessments. Another advantage of a DTCP is to foster a network mindset among healthcare personnel for managing patients with GEP-NETs and develop a more collaborative framework to streamline processes and reduce the risk of repetition and errors arising from poor communication.
Impact of new EURATOM Regulations
The Council Directive 2013/59/EURATOM defined basic safety standards for ionising radiation exposure in a medical setting and was implemented in Italian law in 2020 as statute 101/2020 [51], although several issues around radioprotection, optimisation and the dosimetric approach are yet to be addressed [52].
Under this legislation, lutetium (177Lu)-based treatments could be administered in a day-hospital setting if the necessary safety protocols are in place, whereas, previously, all RLT had to be administered in an inpatient setting. Day-hospital treatment has pros and cons from a clinical and organisational perspective. Although day-hospital administration may not suit all eligible patients, this organisational model could potentially reduce hospital costs and increase the number of centres that can offer RLT, thus improving overall patient access to care. Alternatively, day-hospital administration of lutetium (177Lu)-based treatments could be risky for patients with a high tumour burden or highly functional tumours. In addition, it will be difficult to manage adverse events occurring after discharge, since a ‘radioactive’ patient cannot simply access emergency services or provide samples for assessment without protections being implemented. Therefore, proper characterisation and stratification of patients, as part of the DTCP described above, could help identify those who are potential candidates for day-hospital RLT administration.
We strongly recommend DTCPs, operative procedures and continuous training for day-hospitals to limit the exposure to and risk of radiation contamination of hospital staff (i.e. involved in post-discharge roles and treatment optimisation) and caregivers (i.e. at-home contamination). A personalised, dosimetry-based approach is advisable.
Innovative Medicine Funding and Drug Reporting
In Italy, the fund for innovative oncological drugs (FIO) provided coverage for RLT as a new cancer treatment for the first 36 months after it became available; however, the period for FIO funding of lutetium (177Lu) oxodotreotide ended in March 2022.
In the short term, properly evaluating the number of patients who access RLT each year is mandatory to define budgetary needs. Pharmacists need to be involved in this process to guarantee adequate resources and ensure that this therapy, supported by strong evidence of efficacy and safety, is administered to all patients who can benefit from it. A forecast analysis can be developed from this information, along with accurate budget estimates.
The funding of hospital treatments in Italy is based on diagnosis-related groups (DRGs). Currently, RLT services are coded as DRG409, which is arguably inappropriate for the range of diagnostic, monitoring and treatment modalities involved in this form of therapy, particularly if RLT may be administered in the day-hospital setting.
We recommend that Scientific Societies collaborate for the development of cost mapping and cost-absorption analyses, as well as for the formulation of appropriate DRG codes for RLT at Italian centres.
Discussion and Conclusions
RLT is an effective and well-tolerated treatment option for patients with SSTR-positive progressive G1–G2 GEP-NETs. However, it requires expertise to monitor patients before each administration, during treatment and in the subsequent months or years. We have shared several recommendations based on our experience and expertise as Italian clinicians across various disciplines and have critically reviewed the literature (Table 5). These recommendations do not consider off-label applications of RLT (i.e. using RLT as first-line treatment, retreatment in patients with relapsing GEP-NETs, etc.) because they are not approved by European and Italian agencies and are classified as “investigational” when used in clinical practice.
These recommendations highlight the mandatory role of MDTs in patient selection for RLT. Educating MDTs on RLT is also important and educational initiatives must be appropriate for the whole care team, especially when it is expected that other radioligands will be approved and the use of RLT will rapidly increase. There is a general trend in Europe, supported by ENETS and the European Reference Network on Rare Adult Solid Cancers (EURACAN), that the role of expert centres is to treat patients with rare diseases exclusively. Among the centres conducting RLT in this survey in Italy, six centres are monitored and certified by ENETS, with few exceptions that are hub-and-spoke linked. Their MDTs generally act independently to decide on patient eligibility and diagnostic and therapeutic pathways of patients admitted to RLT. This includes handling of side effects, choice of drugs, protocols before administration in symptomatic patients, use of SSAs during the RLT cycles, use of corticosteroids and/or mannitol in patients with CNS lesions, and eventual imaging modalities and/or other tests.
Conversely, the following options are decided by the nuclear medicine physician: imaging post-RLT for dosimetry, the use of doses lower than the scheduled 740 GBq of 177Lu Lutathera to provide clinical evidence (i.e. renal impairment, haematological toxicity, etc.), as well as the administration of corticosteroids and amino acids before radioligand administration to minimise possible side effects (nausea, vomiting, etc.) and to reduce the delivered dose to the kidneys.
Patients with high bone and/or hepatic tumour burden should not immediately be considered ineligible for RLT but should be carefully assessed within the NET-dedicated MDT focusing on the extent of the disease, the previous therapies and the presence of metastases negative for the expression of SSTR (mismatch results among PET/CT with 68Ga-DOTA-SSA, CT with contrast enhancement or 18FDG-PET/CT).
In Italy, the clinical utilisation of RLT and its funding will benefit from developing a DTCP that can clarify the diagnostic, therapeutic and post-treatment monitoring process and improve care coordination between hub and spoke centres. RLT delivery can also be improved by comprehensive training at both hub and spoke centres. The availability of RLT as an outpatient therapy (i.e. through day-hospitals) is now possible due to the recent 2013/59/EURATOM Directive, which is likely to continue improving access to treatment. However, RLT as outpatient therapy must be carefully planned for patients with risk factors (e.g. comorbidities, high tumour burden and functioning NETs). Another urgent need in the Italian setting is the development of a proper reimbursement tariff devoted to RLT, since funding through the FIO is no longer available. We recommend that Scientific Societies collaborate with policymakers on cost-mapping and reimbursement procedures (e.g. choice of DRG) to ensure that RLT is available for all Italian patients with GEP-NETs who may benefit from this treatment.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
References
Pavel M, Oberg K, Falconi M, et al. Gastroenteropancreatic neuroendocrine neoplasms: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31:844–60.
Roll W, Weckesser M, Seifert R, Bodei L, Rahbar K. Imaging and liquid biopsy in the prediction and evaluation of response to PRRT in neuroendocrine tumors: implications for patient management. Eur J Nucl Med Mol Imaging. 2021;48:4016–27.
European Medicines Agency. Summary of product characteristics - Lutathera. 2017. European Medicines Agency. https://www.ema.europa.eu/en/documents/product-information/lutathera-epar-product-information_en.pdf. Accessed 29 Apr 2022.
Strosberg J, El-Haddad G, Wolin E, et al. Phase 3 trial of 177Lu-Dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376:125–35.
Kwekkeboom DJ, de Herder WW, Kam BL, et al. Treatment with the radiolabeled somatostatin analog [177Lu-DOTA 0, Tyr3]octreotate: toxicity, efficacy, and survival. J Clin Oncol. 2008;26:2124–30.
Merkel C, Whicher CH, Bomanji J, et al. Realising the potential of radioligand therapy: policy solutions for the barriers to implementation across Europe. Eur J Nucl Med Mol Imaging. 2020;47:1335–9.
Severi S, Grassi I, Nicolini S, Sansovini M, Bongiovanni A, Paganelli G. Peptide receptor radionuclide therapy in the management of gastrointestinal neuroendocrine tumors: efficacy profile, safety, and quality of life. Onco Targets Ther. 2017;10:551–7.
Bartolomei M, Berruti A, Falconi M, et al. Clinical management of neuroendocrine neoplasms in clinical practice: a formal consensus exercise. Cancers (Basel). 2022;14(10):2501.
Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr Med. 2006;5:101–17.
Eriksen MB, Frandsen TF. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. J Med Libr Assoc. 2018;106:420–31.
Osborn A. Applied imagination: principles and procedures of creative problem solving. New York: Charles Scribner’s Sons; 1953.
Ambrosini V, Kunikowska J, Baudin E, et al. Consensus on molecular imaging and theranostics in neuroendocrine neoplasms. Eur J Cancer. 2021;146:56–73.
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
World Health Organization. WHO handbook for reporting results of cancer treatment. 1979. Geneva, Switzerland. https://apps.who.int/iris/bitstream/handle/10665/37200/WHO_OFFSET_48.pdf?sequence=1&isAllowed=y. Accessed 29 July 2022.
Rinke A, Muller HH, Schade-Brittinger C, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol. 2009;27:4656–63.
Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European organization for research and treatment of cancer, national cancer institute of the United States, national cancer institute of Canada. J Natl Cancer Inst. 2000;92:205–16.
Caplin ME, Pavel M, Cwikla JB, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371:224–33.
de Mestier L, Dromain C, d’Assignies G, et al. Evaluating digestive neuroendocrine tumor progression and therapeutic responses in the era of targeted therapies: state of the art. Endocr Relat Cancer. 2014;21:R105–20.
Merino-Casabiel X, Aller J, Arbizu J, et al. Consensus document on the progression and treatment response criteria in gastroenteropancreatic neuroendocrine tumors. Clin Transl Oncol. 2018;20:1522–8.
Rozenblum L, Mokrane FZ, Yeh R, et al. Imaging-guided precision medicine in non-resectable gastro-entero-pancreatic neuroendocrine tumors: a step-by-step approach. Eur J Radiol. 2020;122: 108743.
Hope TA, Abbott A, Colucci K, et al. NANETS/SNMMI procedure standard for somatostatin receptor-based peptide receptor radionuclide therapy with 177Lu-DOTATATE. J Nucl Med. 2019;60:937–43.
Riihimaki M, Hemminki A, Sundquist K, Sundquist J, Hemminki K. The epidemiology of metastases in neuroendocrine tumors. Int J Cancer. 2016;139:2679–86.
Cives M, Pelle E, Rinzivillo M, et al. Bone metastases in neuroendocrine tumors: molecular pathogenesis and implications in clinical practice. Neuroendocrinol. 2021;111:207–16.
Altieri B, Di Dato C, Martini C, et al. Bone metastases in neuroendocrine neoplasms: from pathogenesis to clinical management. Cancers (Basel). 2019;11(9):1332.
Sabet A, Khalaf F, Haslerud T, et al. Bone metastases in GEP-NET: response and long-term outcome after PRRT from a follow-up analysis. Am J Nucl Med Mol Imaging. 2013;3:437–45.
Ezziddin S, Sabet A, Heinemann F, et al. Response and long-term control of bone metastases after peptide receptor radionuclide therapy with 177Lu-octreotate. J Nucl Med. 2011;52:1197–203.
Sabet A, Khalaf F, Yong-Hing CJ, et al. Can peptide receptor radionuclide therapy be safely applied in florid bone metastases? A pilot analysis of late stage osseous involvement. Nuklearmedizin. 2014;53:54–9.
Unger N, Ueberberg B, Schulz S, Saeger W, Mann K, Petersenn S. Differential expression of somatostatin receptor subtype 1–5 proteins in numerous human normal tissues. Exp Clin Endocrinol Diabetes. 2012;120:482–9.
Basu S, Ranade R, Thapa P. Metastatic neuroendocrine tumor with extensive bone marrow involvement at diagnosis: evaluation of response and hematological toxicity profile of PRRT with 177Lu-DOTATATE. World J Nucl Med. 2016;15:38–43.
Bergsma H, Konijnenberg MW, Kam BLR, et al. Subacute haematotoxicity after PRRT with 177Lu-DOTA-octreotate: prognostic factors, incidence and course. EJNMMI. 2016;43:453–63.
Baum RP, Kulkarni HR, Singh A, et al. Results and adverse events of personalized peptide receptor radionuclide therapy with 90Yttrium and 177Lutetium in 1048 patients with neuroendocrine neoplasms. Oncotarget. 2018;9:16932–50.
Guerra Liberal FDC, Tavares AAS, Tavares J. Palliative treatment of metastatic bone pain with radiopharmaceuticals: a perspective beyond strontium-89 and samarium-153. Appl Radiat Isot. 2016;110:87–99.
Bouchet LG, Bolch WE, Goddu SM, Howell RW, Rao DV. Considerations in the selection of radiopharmaceuticals for palliation of bone pain from metastatic osseous lesions. J Nucl Med. 2000;41:682–7.
Scopel M, De Carlo E, Bergamo F, et al. Bone metastases from neuroendocrine tumors: clinical and biological considerations. Endocr Connect. 2022;11(7): e210568.
Strosberg J, Kunz PL, Hendifar A, et al. Impact of liver tumour burden, alkaline phosphatase elevation, and target lesion size on treatment outcomes with 177Lu-Dotatate: an analysis of the NETTER-1 study. Eur J Nucl Med Mol Imaging. 2020;47:2372–82.
Bober B, Saracyn M, Zareba K, et al. Early complications of radioisotope therapy with lutetium-177 and yttrium-90 in patients with neuroendocrine neoplasms-a preliminary study. J Clin Med. 2022;11(4):919.
Neri E, Bali MA, Ba-Ssalamah A, et al. ESGAR consensus statement on liver MR imaging and clinical use of liver-specific contrast agents. Eur Radiol. 2016;26:921–31.
Hayoz R, Vietti-Violi N, Duran R, Knebel JF, Ledoux JB, Dromain C. The combination of hepatobiliary phase with Gd-EOB-DTPA and DWI is highly accurate for the detection and characterization of liver metastases from neuroendocrine tumor. Eur Radiol. 2020;30:6593–602.
Malla S, Kumar P, Madhusudhan KS. Radiology of the neuroendocrine neoplasms of the gastrointestinal tract: a comprehensive review. Abdom Radiol (NY). 2021;46:919–35.
Dietrich CF, Nolsoe CP, Barr RG, et al. Guidelines and good clinical practice recommendations for contrast-enhanced ultrasound (CEUS) in the liver-update 2020 WFUMB in cooperation with EFSUMB, AFSUMB, AIUM, and FLAUS. Ultrasound Med Biol. 2020;46:2579–604.
Knigge U, Capdevila J, Bartsch DK, et al. ENETS Consensus Recommendations for the standards of care in neuroendocrine neoplasms: follow-up and documentation. Neuroendocrinol. 2017;105:310–9.
Airtum Working Group, Busco S, Buzzoni C, et al. Italian cancer figures–Report 2015: the burden of rare cancers in Italy. Epidemiol Prev. 2016;40:1–120.
Gusani NJ, Schubart JR, Wise J, et al. Cancer survivorship: a new challenge for surgical and medical oncologists. J Gen Intern Med. 2009;24(Suppl 2):S456–8.
Shapiro CL. Cancer survivorship. N Engl J Med. 2018;379:2438–50.
Aaronson NK, Mattioli V, Minton O, et al. Beyond treatment - psychosocial and behavioural issues in cancer survivorship research and practice. EJC Suppl. 2014;12:54–64.
Simard S, Thewes B, Humphris G, et al. Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv. 2013;7:300–22.
Horick NK, Manful A, Lowery J, et al. Physical and psychological health in rare cancer survivors. J Cancer Surviv. 2017;11:158–65.
Ratcliff C, Naik AD, Martin LA, Moye J. Examining cancer survivorship trajectories: exploring the intersection between qualitative illness narratives and quantitative screening instruments. Palliat Support Care. 2018;16:712–8.
Campbell H, Hotchkiss R, Bradshaw N, Porteous M. Integrated care pathways. BMJ. 1998;316:133–7.
Jacka JM, Keller PJ. RACI Matrices. In: Jacka JM, Keller PJ, editors. Business process mapping: improving customer satisfaction. 2nd ed. Hoboken, NJ, USA: John Wiley & Sons; 2009. p. 255–76.
European Union. Council Directive 2013/59/Euratom of 5 December 2013 laying down basic safety standards for protection against the dangers arising from exposure to ionising radiation, and repealing Directives 89/618/Euratom, 90/641/Euratom, 96/29/Euratom, 97/43/Euratom and 2003/122/Euratom. 2013. EUR-Lex. https://eur-lex.europa.eu/eli/dir/2013/59/oj. Accessed 2 Mar 2023.
Chiesa C, Strigari L, Pacilio M, et al. Dosimetric optimization of nuclear medicine therapy based on the Council Directive 2013/59/EURATOM and the Italian law N. 101/2020. Position paper and recommendations by the Italian national Associations of Medical Physics (AIFM) and Nuclear Medicine (AIMN). Phys Med. 2021;89:317–26.
Medical Writing, Editorial and Other Assistance.
Editorial assistance in the preparation of this article was provided by Andrea Govender and Catherine Rees, who wrote the outline and first draft of this manuscript, respectively, on behalf of Springer Healthcare Communications. Support for this assistance was funded by Sentrix/VMLY&Rx.
Authorship.
All listed authors have made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; drafted the work or revised it critically for important intellectual content; approved the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy of integrity of any part of the work are appropriately investigated and resolved.
Funding
Sponsorship for this study, medical writing assistance and the Rapid Service and Open Access Fee were funded by Sentrix/VMLY&Rx.
Author information
Authors and Affiliations
Contributions
Nicola Fazio, Massimo Falconi, Emanuela Foglia and Secondo Lastoria conceptualised the manuscript and, together with Mirco Bartolomei, Alfredo Berruti, Mirko D’Onofrio, Diego Ferone, Alessandro Giordano, Franco Grimaldi, Massimo Milione, Francesco Panzuto, Monica Santimaria, Orazio Schillaci, Ettore Seregni, Michele Stasi and Marco Volante. All authors contributed to the study conception and material preparation and commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Nicola Fazio has received fees for public speaking and advisory board activities from Novartis, Advanced Accelerator Applications, Ipsen, Sanofi, Hutchmed, Merck and MSD. Mirco Bartolomei has received fees for advisory board activities from Advanced Accelerator Applications. Diego Ferone has received fees for public speaking and advisory board activities from Advanced Accelerator Applications, Ipsen, Sandoz, Recordati and Camurus. Emanuela Foglia has received educational grants and advisory boards fees from Advanced Accelerator Applications, Ethicon, Astellas Pharma and Werfen—Instrumentation Laboratories. Franco Grimaldi has received fees from Advanced Accelerator Applications, Novo Nordisk, Boehringer Ingelheim, Ipsen, Merck, Eisai and Roche. Marco Volante has received fees for advisory board activities from Advanced Accelerator Applications. Secondo Lastoria has received fees for advisory board activities from Advanced Accelerator Applications. Massimo Falconi, Alfredo Berruti, Mirko D’Onofrio, Alessandro Giordano, Massimo Milione, Francesco Panzuto, Monica Santimaria, Orazio Schillaci, Ettore Seregni, and Michele Stasi declare that they have no competing interests.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Fazio, N., Falconi, M., Foglia, E. et al. Optimising Radioligand Therapy for Patients with Gastro-Entero-Pancreatic Neuroendocrine Tumours: Expert Opinion from an Italian Multidisciplinary Group. Adv Ther 41, 113–129 (2024). https://doi.org/10.1007/s12325-023-02714-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02714-8