Abstract
Background
Palmoplantar pustulosis (PPP) is a chronic inflammatory condition characterized by sterile pustules on the palms and soles. This study evaluated the epidemiology of PPP using claims and electronic health record (EHR) databases.
Methods
Patients coded for PPP in the United States (US) and Japan from 2016 to 2020 were identified. Several PPP definitions were evaluated; the specific definition (≥ 2 visits coded for PPP, the second 31–730 days after diagnosis) was chosen for characterizing PPP epidemiology. Baseline characteristics and pre- and post-diagnosis treatments were summarized. Prevalence and incidence rates were analyzed by calendar year, sex, age, and database.
Results
Prevalence and incidence of PPP were higher in Japan than the US. PPP prevalence increased over time. PPP occurred predominantly in adulthood and was more common among women. Features of metabolic syndromes, anxiety, and depression were more common among US PPP patients. Consistently high baseline use of anti-bacterial, anti-inflammatory/anti-rheumatic, and obstructive airway disease treatments was observed among PPP patients. Potential miscoding or misclassification of PPP limited this analysis. Prevalence estimates from databases may differ from field- and population-based approaches.
Conclusions
The burden of PPP was greater in Japan than in the US. Additional studies are needed to further elucidate PPP epidemiology worldwide.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Palmoplantar pustulosis (PPP) prevalence and incidence of PPP were an order of magnitude higher in Japan than the United States (US); prevalence of disease increased over time in both countries. |
PPP occurred predominantly in adulthood and was more common among women. |
This analysis provides insight into characteristics associated with PPP and highlights the greater burden of disease in Japan versus the US. |
Introduction
Palmoplantar pustulosis (PPP) is a rare, chronic, and debilitating inflammatory skin condition characterized by recurrent crops of sterile pustules on the palms and soles [1, 2]. The categorization of PPP is evolving; whether it represents a subtype of palmoplantar psoriasis, a localized type of pustular psoriasis, or a separate condition is unclear [3]. PPP may present as a primary condition, in association with plaque psoriasis or paradoxical psoriasis (tumor necrosis factor [TNF]-induced psoriasis/psoriasiform dermatitis), or as a feature of auto-inflammatory syndromes, such as synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome [3, 4]. Although insights into the potential roles of the interleukin (IL)-17, IL-36, and TNF pathways have been gained, the pathogenesis of PPP remains unknown [3, 5, 6].
Because PPP is designated by a single International Classification of Disease version 10 (ICD-10) diagnostic code, health insurance claims and electronic health record (EHR) databases may be used to study the epidemiology of PPP. Using national claims data, Kubota et al. reported a prevalence for PPP of 0.12% in Japan [7]; however, the reported prevalence of PPP was lower (0.001–0.08%) using data from the United States (US) and Europe (Denmark, Germany, and Sweden) [8, 9]. Nonetheless, all these studies found PPP to be more prevalent among women than men and, in studies that included age-specific estimates, PPP was very rare among patients < 18 years of age [7, 9].
Our study sought to further characterize the epidemiology of PPP using claims and EHR databases, specifically in the US and Japan. The study evaluated PPP prevalence and incidence, baseline patient characteristics, and treatments initiated after PPP diagnosis. In addition, we propose novel definitions of PPP to explore approaches for optimizing criteria for identifying PPP patients in claims and EHR databases.
Methods
Study Population
The ICD-10 code for PPP (L40.3), adopted in Japan in 1994 and the US in 2015, was used to identify patients. Consequently, this analysis was restricted to patients diagnosed with PPP from 2016 to 2020. Three PPP definitions were chosen for consideration: a sensitive definition based on one visit with a PPP diagnostic code; a specific definition requiring ≥ 2 visits with a PPP code (the second 31–730 days after the first); and a hybrid definition consisting of the specific definition or a single PPP code from a dermatology setting. During evaluation of these definitions, search queries identified infants with post-scabetic acral pustules who were misdiagnosed/misclassified as having PPP. Therefore, patients of any age who were diagnosed with scabies (infestation by Sarcoptes scabiei var. hominis) or the related condition, acropustulosis of infancy, and/or those prescribed scabies treatments were excluded from the sensitive definition. The specific and hybrid definitions inherently excluded cases of misdiagnosed PPP in infants.
The study population included patients of all ages. For the purposes of epidemiology characterization, the primary analysis was based on the specific PPP definition.
Databases
This study included four claims databases from the US [IBM®MarketScan® Commercial Database (CCAE), Optum’s de-identified Clinformatics® DataMart Database (Optum SES), IBM®MarketScan® Multi-State Medicaid Database (MDCD), and IBM®MarketScan® Medicare Supplemental Database (MDCR)], one claims database from Japan [Japan Medical Data Center (JMDC©)], and one US EHR database [Optum® de-identified Electronic Health Record Dataset (Optum EHR)]. CCAE, Optum SES, and Optum EHR represent privately insured patients across the US. MDCR represents patients with private insurance and supplemental Medicare insurance, whereas MDCD represents patients with public insurance (Medicaid). MDCR is generally limited to patients ≥ 65 years of age. JMDC included claims for employed patients and their dependents, and is limited to enrollees < 65 years of age. Data from all the databases were converted to the Observational Medical Outcome Partnership Common Data Model, Version 5.3.1 [10, 11].
Statistical Analysis
For all definitions, the index date was defined by the first diagnosis code. Index dates could be adjusted to account for potential misclassification if PPP-associated signs and symptoms occurred within 30 days of the initial PPP diagnosis. Baseline characteristics were summarized using data from the year before the index date. Pre- and post-index assessments examined PPP treatments prescribed in the years prior to and after the index date.
Consistent with the period prevalence methodology outlined by the Centers for Disease Control [12], annual prevalence estimates were calculated using the number of patients diagnosed with PPP during or prior to a given calendar year divided by the number of patients in the database on July 1 (mid-interval population). Incidence rate estimates were calculated as patients/1000 person-years, excluding patients with PPP prior to the index date. Prevalence and incidence rates were analyzed by calendar year, sex, age, and database. Analyses were performed using a web-based, interactive, Observational Health Data Sciences and Informatics (OHDSI)-developed Cohort Diagnostics application (Version 2.2.4; https://ohdsi.github.io/CohortDiagnostics/).
Results
Identified PPP Patients
Fewer patients with PPP were identified using the specific versus the sensitive PPP definition (Table 1). The primary analysis, reported here, focused on patients identified using the specific definition.
Using the specific definition, more PPP patients were identified in JMDC (n = 6376) than in the US databases; the fewest PPP cases were identified in MDCD (n = 578) and MDCR (n = 195; Table 1). Most patients in the specific PPP cohort were ≥ 18 years of age. Index dates were adjusted for misclassification in 10–20% of patients across the databases. Counts and characteristics may be viewed interactively at https://data.ohdsi.org/PPPCohortDiagnostics.
Prevalence and Incidence of PPP
PPP was rare across all the databases, although the prevalence of PPP was an order of magnitude higher in JMDC (Supplementary Information Fig. 1) versus US databases (Fig. 1). For example, in 2020, the prevalence/100,000 people was 89.35 in Japan versus 8.68, 7.43, and 6.41 for Optum EHR, Optum SES, and CCAE, respectively (Supplementary Information Table 1). Higher prevalence of PPP among women versus men was observed across databases (Supplementary Information Tables 1, 2, 3, 4, 5). With each year, the prevalence of PPP increased across all databases, except for a slight decline in 2020 in MDCR (Supplementary Information Table 1), which may reflect disruption in non-urgent services associated with the COVID-19 pandemic. This increase in PPP prevalence was primarily driven by patients ≥ 18 years of age; PPP prevalence was limited among pediatric patients (Supplementary Information Tables 2, 3, 4). Based on US data, the estimated PPP prevalence/100,000 population in 2020 was ≤ 1.28 and ≤ 2.37 among patients ≤ 11 years of age and 12–17 years of age, respectively. In contrast, the estimated PPP prevalence for 2020 using data from Japan was 14.51 for patients ≤ 11 years of age and 27.25 for those 12–17 years of age. PPP incidence rates were generally consistent with patterns of PPP prevalence. Incidence of PPP was greater in Japan than the US, and higher among women than men. However, unlike prevalence, PPP incidence rates were generally stable over time (Fig. 2; Supplementary Information Fig. 2).
Prevalence using the specific PPP definition by database, aage, and sex. aOnly US databases are shown; see Fig. 2 for prevalence based on the specific PPP definition in JMDC. MDCR includes only adults ≥ 65 years of age; thus, data from MDCR were excluded from the figure to facilitate interpretability of the graphs. PPP palmoplantar pustulosis, EHR Optum® de-identified Electronic Health Record Database, SES Optum’s Clinformatics® de-identified Data Mart Database, CCAE IBM® MarketScan® Commercial Database, MDCD IBM® MarketScan® Multi-State Medicaid Database, MDCR IBM® MarketScan® Medicare Supplemental Database, US United States
Incidence rates using the specific PPP definition by database, age, and sex. PPP palmoplantar pustulosis, JMDC Japan Medical Data Center, EHR Optum® de-identified Electronic Health Record Database, SES Optum’s Clinformatics® de-identified Data Mart Database, CCAE IBM® MarketScan® Commercial Database, MDCD IBM® MarketScan® Multi-State Medicaid Database, MDCR IBM® MarketScan® Medicare Supplemental Database, US United States
Characteristics of PPP Patients
Among patients identified using the specific PPP definition, PPP occurred predominantly in adulthood and was more common among women across databases (Table 2). A higher proportion of women with PPP was seen in the US databases (67–79%) versus JMDC (57%; Table 2). In MDCD, 3% of patients with PPP were Hispanic/Latino, 32% were Black/African American, and 52% were White. Compared with MDCD, Optum EHR and Optum SES had fewer PPP patients who were Black/African American (9–11%) and more patients who were White (75–84%); a similar proportion was Hispanic/Latino (4–7%).
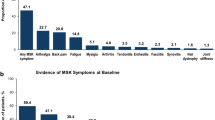
Comorbidities associated with metabolic syndrome (e.g., diabetes) were consistently more common among US versus Japanese PPP patients, as were anxiety and depression (Table 3). Most autoimmune or inflammatory conditions (e.g., atopic dermatitis) occurred in PPP patients with varying frequency across databases, with some exceptions; hidradenitis suppurativa, idiopathic arthritis, and psoriatic arthritis were less common in JMDC than US databases, and atopic dermatitis was more common in JMDC. Across databases, acute respiratory disease and visual system disorders were commonly associated with PPP (≥ 40% in JMDC; ≥ 30% in ≥ 1 US database).
Consistently high baseline use of anti-bacterial (46–71%), obstructive airway disease (56–76%), and anti-inflammatory/anti-rheumatic (28–51%) treatments was observed. Higher rates of anti-malarial treatment use were seen in the US (2–3% pre-diagnosis; 1–2% post-diagnosis, where estimates were available) compared with Japan, where anti-malarial treatment was rare (< 0.1% pre- and post-diagnosis). At baseline, treatments for conditions associated with metabolic syndromes and mental health conditions were more commonly prescribed for PPP patients in the US than Japan, mirroring the frequency of their corresponding comorbidities.
Use of retinoids (5–7%), mostly acitretin, was observed in the post-diagnosis period in the US; however, evidence for their use was rare (≤ 1%) in Japan. Pre-diagnosis treatment with anti-TNFα agents was more frequent in US databases than in JMDC (4–13% and 0.8%, respectively, Supplementary Information Table 6), a pattern that was also seen 31–365 days post-diagnosis (6–16% and 0.8%, respectively; Supplementary Information Table 7). In the US, adalimumab (4–10%), secukinumab (3%), and ustekinumab (2–3%) were the most frequently prescribed post-diagnosis biologics. Post-diagnosis use of biologics was rare (≤ 1%) in Japan; however, post-diagnosis use of phototherapy was more common in Japan than in the US. This observation is consistent with common clinical practice since patients in Japan typically must fail to respond to phototherapy and/or topical corticosteroids before treatment with biologics is considered.
Discussion
Through analysis of several available health insurance claims and EHR databases, this study sought to characterize the epidemiology of PPP in the US and Japan. Our findings identified an order of magnitude greater burden (by prevalence and incidence) of PPP in Japan versus the US. Despite this striking cross-national difference, results from both countries indicated PPP is more common among women and is rarely seen in patients < 25 years of age. In both countries, prevalence of PPP increased over time, which may reflect improvements in recognizing and reporting the condition. In all evaluated US databases, the prevalence and incidence of PPP were low and would meet the US Food and Drug Administration’s criteria for rare disease [13].
Multiple factors may contribute to the differences in prevalence and incidence of PPP observed between Japan and the US in this study. Recognition of PPP as a disorder distinct from other psoriatic conditions may be inconsistent across different medical communities. Familiarity with PPP diagnostic coding may be another factor, particularly since ICD-10 (which introduced the code for PPP) was implemented earlier in Japan than the US. Genetic and environmental factors may also contribute to the differences in PPP prevalence and incidence between countries.
Our study estimated the prevalence of PPP/100,000 population in 2020 to be 89.4 in Japan, based on JMDC, and 8.7, 7.4, and 6.4 in the US based on Optum EHR, Optum SES, and CCAE, respectively. Research derived from nationwide claims data in Japan from 2010–2011 reported a PPP prevalence of 120/100,000 [7]. Nationwide data from Sweden reported a prevalence of 20–26/100,000 [9]. Another analysis reported prevalence estimates of 9, 5, and 80/100,000 based on databases from the US, Demark, and Germany, respectively; the authors postulated that the higher PPP prevalence in Germany may be attributed to inter-country differences in healthcare access, diagnosis, or coding [8]. Nonetheless, consistent with our findings, each of these studies found that PPP was more common among women and, where analyzed, was rare in pediatric patients.
US-based rates in our study were consistent with estimates from Denmark, but not Sweden or Germany. There are several possible reasons for these differences. First, other studies of PPP employed a variety of different approaches to define PPP [7,8,9, 14, 15]. Our analysis required two visits with PPP diagnostic codes, the second occurring 31–730 days after the first. This more stringent definition is likely to yield lower, but potentially more accurate, prevalence estimates compared to less restrictive definitions. Second, the databases may reflect diversity in healthcare systems and the patient populations they serve in different countries (nationwide single-payer systems in Japan, Sweden, Demark, and Germany; a subset of insurance for employed individuals and their dependents in JMDC; private, commercial insurance [e.g., CCAE] and public insurance [e.g., MDCD] in the US). Lastly, variability in the methods used to estimate prevalence (e.g., specifying the denominator) may have contributed to divergent results.
We found significant comorbidity, particularly components of metabolic syndrome, among patients with PPP. The presence of such comorbidities was more pronounced in patients from the US than Japan. This may reflect country-specific differences in factors such as lifestyle and/or diet, or differences in approach to treatment of these comorbidities. Mental health conditions such as anxiety and depression, while more common in the US, were notably prevalent among PPP patients in both countries, and may, in part, reflect the debilitating nature of PPP and its impact on quality of life [2].
Although it may seem paradoxical, anti-TNFα treatment may exacerbate or lead to development of de novo psoriasiform palmoplantar skin lesions [6, 16, 17]. Approximately 10% of US-based patients in our study had an anti-TNFα treatment in the year prior to diagnosis, whereas use of TNFα inhibitors was less common (< 1%) among Japanese PPP patients. This disparity in use of anti-TNFα agents may account for the greater incidence of anti-TNFα–induced PPP in the US. Alternatively, anti-TNFα-induced palmoplantar disease may be misclassified as PPP in the US or there may be a higher prevalence of idiopathic PPP in Japan. In our analysis of US data, the occurrence of anti-TNFα–induced PPP was more common among women, a finding consistent with prior research [6]. Data regarding other risk factors, such as smoking, were not systematically collected and could not be assessed; however, potential proxies, such as prevalence of chronic obstructive lung disease and treatment for obstructive airway diseases were common among PPP patients in both countries.
This analysis developed and evaluated strategies to identify PPP cases in claims and EHR data, resulting in three candidate definitions for PPP. Consideration of different criteria to identify PPP patients was a strength of our approach. Ultimately, we chose the specific definition for this epidemiological analysis to minimize capturing data from misdiagnosed and/or non-PPP patients. Nonetheless, further studies using chart review approaches and/or manual curation of narrative text from EHRs may help validate the specific definition. Such studies may provide additional insights into the value of the hybrid PPP definition, including whether this definition should be considered for future analyses. Furthermore, future studies may evaluate alternative PPP definitions (e.g., excluding plaque psoriasis and/or dyshidrotic eczema [or pompholyx]) or assess impacts on inter-country prevalence, incidence estimates, and baseline characteristics. Lastly, our study analyzed data from two countries and several different types of databases, capturing PPP data in a variety of patient populations, which we believe is a strength.
Nonetheless, this study has limitations inherent to the observational nature of the data. There may be biases in the validity of claims codes for both PPP and the baseline comorbidities that we assessed, as some codes may be subject to miscoding/misclassification. In addition, as the databases reflect information collected during patient interactions across various healthcare systems, prevalence estimates from these claims and EHR databases may differ from field- and population-based approaches that systematically assess disease occurrence through surveys. Despite these limitations, we believe this analysis contributes to better understand the overall epidemiology of PPP.
Conclusion
In this cross-national study based on claims and EHR data, we examined the epidemiology of PPP and confirmed a greater burden of PPP in Japan than the US. Although rare, PPP is a debilitating condition with high unmet medical need and increasing prevalence. Further research is needed to identify factors that contribute to patterns of PPP epidemiology and disease severity, particularly using data from other sources, settings, and geographic locations.
Data Availability
The data sharing policy of Janssen Pharmaceutical Companies of Johnson and Johnson is available at http://www.janssen.com/clinical-trials/transparency. These data were made available by Optum and used under license for the current study and are not publicly available. Other researchers should contact Optum.
References
Yamamoto T. Clinical characteristics of Japanese patients with palmoplantar pustulosis. Clin Drug Investig. 2019;39(3):241–52.
Misiak-Galazka M, Wolska H, Rudnicka L. What do we know about palmoplantar pustulosis? J Eur Acad Dermatol Venereol. 2017;31(1):38–44.
Murakami M, Terui T. Palmoplantar pustulosis: current understanding of disease definition and pathomechanism. J Dermatol Sci. 2020;98(1):13–9.
Benzaquen M, Flachaire B, Rouby F, Berbis P, Guis S. Paradoxical pustular psoriasis induced by ustekinumab in a patient with Crohn’s disease-associated spondyloarthropathy. Rheumatol Int. 2018;38(7):1297–9.
Misiak-Galazka M, Zozula J, Rudnicka L. Palmoplantar pustulosis: recent advances in etiopathogenesis and emerging treatments. Am J Clin Dermatol. 2020;21(3):355–70.
Shmidt E, Wetter DA, Ferguson SB, Pittelkow MR. Psoriasis and palmoplantar pustulosis associated with tumor necrosis factor-alpha inhibitors: the Mayo Clinic experience, 1998 to 2010. J Am Acad Dermatol. 2012;67(5):e179-185.
Kubota K, Kamijima Y, Sato T, et al. Epidemiology of psoriasis and palmoplantar pustulosis: a nationwide study using the Japanese national claims database. BMJ Open. 2015;5(1): e006450.
Andersen YMF, Augustin M, Petersen J, et al. Characteristics and prevalence of plaque psoriasis in patients with palmoplantar pustulosis. Br J Dermatol. 2019;181(5):976–82.
Lofvendahl S, Norlin JM, Schmitt-Egenolf M. Prevalence and incidence of palmoplantar pustulosis in Sweden: a population-based register study. Br J Dermatol. 2021. https://doi.org/10.1111/bjd.20087.
Overhage JM, Ryan PB, Reich CG, Hartzema AG, Stang PE. Validation of a common data model for active safety surveillance research. J Am Med Inform Assoc. 2012;19(1):54–60.
Voss EA, Makadia R, Matcho A, et al. Feasibility and utility of applications of the common data model to multiple, disparate observational health databases. J Am Med Inform Assoc. 2015;22(3):553–64.
Centers for Disease Control. Morbidity Frequency Measures in Principles of Epidemiology in Public Health Practice, Third Edition. Accessed 9 Feb 2022. https://www.cdc.gov/csels/dsepd/ss1978/lesson3/section2.html
US Food and Drug Administration. FDA Insight: Rare Diseases and Orphan Products. Interview. Updated 12/01/2020. Accessed 7 Mar 2022. https://www.fda.gov/news-events/fda-insight/fda-insight-rare-diseases-and-orphan-products
Miyazaki C, Sruamsiri R, Mahlich J, Jung W. Treatment patterns and healthcare resource utilization in palmoplantar pustulosis patients in Japan: a claims database study. PLoS One. 2020;15(5): e0232738.
Hanna ML, Singer D, Valdecantos WC. Economic burden of generalized pustular psoriasis and palmoplantar pustulosis in the United States. Curr Med Res Opin. 2021;37(5):735–42.
Ko JM, Gottlieb AB, Kerbleski JF. Induction and exacerbation of psoriasis with TNF-blockade therapy: a review and analysis of 127 cases. J Dermatolog Treat. 2009;20(2):100–8.
Collamer AN, Battafarano DF. Psoriatic skin lesions induced by tumor necrosis factor antagonist therapy: clinical features and possible immunopathogenesis. Semin Arthritis Rheum. 2010;40(3):233–40.
Medical Writing and Editorial Assistance
The authors gratefully acknowledge Shawn Black and Hillary Van valkenburgh for their contributions to early interpretation of this analysis. Medical writing support was provided by Erica S. Chevalier-Larsen, PhD, of Janssen Scientific Affairs, LLC, under the direction of the authors and in accordance with Good Publication Practice guidelines (DeTora LM, et al. Ann Intern Med. 2022;175(9):1298–1304).
Funding
This study was supported by Janssen Research & Development, LLC, including support for journal and their Rapid Service and Open Access fees for this publication.
Author information
Authors and Affiliations
Contributions
Darmendra Ramcharran, Bruce Strober, Kenneth Gordon, Cynthia M.C. DeKlotz, Steven Fakharzadeh, Ya-Wen Yang, Joel Swerdel, Jill Hardin, Sridhar Dronavalli and Amy Paller contributed to the study design. Darmendra Ramcharran, Joel Swerdel and Jill Hardin analysed the data and all authors participated in interpretation of the data. Darmendra Ramcharran wrote the first draft of the manuscript and all authors provided critical review and revisions of the manuscript. All authors attest to the completeness and accuracy of the data.
Corresponding author
Ethics declarations
Conflict of Interest
At the time the research was conducted, Darmendra Ramcharran was an employee of Janssen Research & Development; he is currently an employee of GSK. Bruce Strober served as a consultant (honoraria) and/or speaker and/or investigator for AbbVie, Almirall, Amgen, Arcutis, Arena, Aristea, Asana, Boehringer Ingelheim, Bristol Myers Squibb, Cara, Connect Biopharma, CorEvitas Psoriasis Registry, Dermavant, Dermira, Eli Lilly, EPI Health, Evelo Biosciences, Immunic Therapeutics, Incyte, Janssen, LEO Pharma, Maruho, Meiji Seika Pharma, Mindera Health, Novartis, Ono, Pfizer, Regeneron, Sanofi-Genzyme, Sun Pharma, UCB Pharma, Union Therapeutics, Ventyxbio, and vTvt Therapeutics; served as co-Scientific Director (consulting fee) of CorEvitas (formerly Corrona) Psoriasis Registry and Editor-in-Chief (honorarium) of Journal of Psoriasis and Psoriatic Arthritis. Kenneth Gordon received research/grant support from AbbVie, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly, Janssen, Novartis, and UCB Pharma, and honoraria for consultation from AbbVie, Amgen, Boehringer Ingelheim, Celgene, Dermira, Eli Lilly, Janssen, Novartis, and UCB Pharma. Amy Paller has been an investigator for AbbVie, Dermavant, Eli Lilly, Incyte, Janssen, Krystal, and UCB; a consultant with honorarium for Aegerion Pharma, Azitra, BioCryst, Boehringer Ingelheim, Bristol Myers Squibb, Castle Creek, Eli Lilly, Janssen, Krystal, LEO Pharma, Novartis, Regeneron, Sanofi/Genzyme, Seanergy, TWI Biotechnology, and UCB; and is on data safety monitoring boards for AbbVie, Abeona, Catawba, Galderma, and InMed. Cynthia DeKlotz, Joel Swerdel, and Jill Hardin are employees of Janssen Research & Development and Steven Fakharzadeh and Ya-Wen Yang are employees of Immunology Global Medical Affairs, Janssen Pharmaceutical Companies of Johnson & Johnson; employees may own stock in Johnson & Johnson, of which Janssen is a subsidiary. Sridhar Dronavalli has no conflicts to disclose.
Ethical Approval
The Optum and IBM MarketScan databases used in this study were reviewed by the New England Institutional Review Board (IRB) and were determined to be exempt from broad IRB approval, as this research project did not involve human subject research. Based on Ethical Guidelines for Epidemiological Research issued by the Japanese Ministry of Health, Labor and Welfare, ethics approval and informed consent for the JMDC database were not applicable for this study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ramcharran, D., Strober, B., Gordon, K. et al. The Epidemiology of Palmoplantar Pustulosis: An Analysis of Multiple Health Insurance Claims and Electronic Health Records Databases. Adv Ther 40, 5090–5101 (2023). https://doi.org/10.1007/s12325-023-02669-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02669-w