Abstract
Introduction
VEIN STEP was conducted to collect international data on the management of chronic venous disease (CVD) and to assess the effectiveness of conservative treatments for the relief of CVD signs and symptoms.
Methods
This international, observational, prospective, longitudinal, cohort study recruited adult outpatients consulting for symptomatic CVD. The primary objective was the effectiveness of conservative treatments on symptoms, signs and quality of life in a real-life setting assessed using a range of patient-reported outcome measures: 10-cm Visual Analog and Patient Global Impression of Change scales for symptoms; Venous Clinical Severity Score for physician assessment of signs; and 14-item ChronIc Venous Insufficiency Questionnaire (CIVIQ-14) for quality of life. At inclusion, patients were prescribed conservative treatment according to the physicians’ usual practice. Follow-up visits took place at weeks 2 and 4, with an optional week 8 visit.
Results
The analysis set comprised 6084 subjects (78% female) from nine countries with a mean age of 50.6 ± 13.8 years and BMI of 28.0 ± 4.9 kg/m2. The most common CEAP classifications were C1 (23.0%), C2 (31.6%), and C3 (30.7%). Conservative therapy consisted of oral venoactive drugs (VADs; 95.8% of subjects) including micronized purified flavonoid fraction (MPFF 75.5%) and diosmin (18.8%), compression (52.0%), and topicals (31.5%). Conservative therapy led to global symptom improvement in 89% of patients after 2 weeks and 96% at 4 weeks. Pain, leg heaviness, cramps, and sensation of swelling were improved in 82%, 71%, 45.5%, and 46% of patients, respectively. Conservative therapy was associated with a decrease over time in patient-assessed global symptom intensity: – 2.37 ± 1.73 (P < 0.001) and physician-assessed disease severity – 1.83 ± 2.82 (P < 0.001). Among the VADs, MPFF-based conservative therapy was associated with the greatest reduction in symptom and sign intensity. Improvements in CIVIQ-14 were observed with all treatments but were greatest for MPFF.
Conclusion
In this prospective study conducted in the real-world setting, treatment with conservative therapy, in particular MPFF, was associated with meaningful improvements in the clinical signs and symptoms of disease as well as in quality of life in patients with CVD.
Trial Registration
ClinicalTrials.gov identifier NCT04574375.
Plain Language Summary
The VEIN STEP study aimed to gather global data on managing chronic venous disease (CVD) and evaluate the usefulness of conservative (non-surgical) treatments for improving CVD signs and symptoms.
AbstractSection MethodsPersons included in the study group had symptomatic CVD and were visiting outpatient clinics. The main aim was to measure how well treatments improved symptoms, physical signs of the illness, and quality of life. Different methods were used to measure these aspects, such as rating symptoms on a 10-point scale and using questionnaires completed by patients and doctors.
AbstractSection Study Findings6084 participants from nine countries joined the study. They were mostly women (78%) with an average age of around 50. Common symptoms included leg pain and leg heaviness. Treatments consisted mainly of drugs active on vein function, like MPFF and diosmin, along with compression stockings and creams. Conservative treatment led to symptom improvement in 89% of patients after 2 weeks and 96% at 4 weeks. Pain and leg heaviness improved in most patients (82% and 71% over the same period) while cramps, and swelling showed improvement in 45.5% and 46% of patients, respectively. Patients reported a significant decrease in symptom intensity, and doctors observed a reduction in disease severity. MPFF was associated with the highest reduction in symptom intensity. Improvements in quality of life were observed with all treatments but were greatest for MPFF.
AbstractSection ConclusionThe study highlights that conservative treatments, especially MPFF, are associated with significant improvements in the clinical signs and symptoms of patients with CVD as well as in their quality of life.
Similar content being viewed by others
Why carry out this study? |
To ensure optimal treatment practices and outcomes of chronic venous disease (CVD), there is a need to assess the characteristics of the disease in representative samples of the general population and to examine the way it is managed in everyday clinical practice. |
VEIN STEP is an international, observational, prospective study assessing the effectiveness of different conservative treatments for the relief of CVD symptoms, and their impact on quality of life (QoL). |
VEIN STEP used a range of patient-reported outcomes to assess symptom severity and improvement with treatment. |
What was learned from the study |
Treatment with conservative therapy, mainly in the form of venoactive drugs, is effective in real-world settings for improving CVD-associated symptoms and QoL, and is associated with high patient and physician satisfaction. |
Among the venoactive drugs, micronized purified flavonoid fraction (MPFF) was the most widely prescribed agent. |
Introduction
Chronic venous disease (CVD) is a progressive condition with a growing global burden associated with aging populations, increasing levels of obesity, and a more sedentary lifestyle [1]. Prevalence rates determined at general practitioners’ (GP) consultations range from 52% in Asia, 62% in Western Europe, 68% in Latin America, to 70% in Eastern Europe [2]. While CVD pathophysiology is complex and involves genetic susceptibility and environmental factors [3], it is commonly caused by venous hypertension, inflammation, and valvular incompetence [4,5,6]. These pathogenetic mechanisms are self-reinforcing and involved in all stages of CVD.
A wide spectrum of progressive signs then develops ranging in severity from telangiectasias to venous ulcers [7]. Pain, heaviness, itching, and burning symptoms can be present from the outset, before any clinical signs become evident [8, 9]. The condition is gradually progressive, with 5% of patients experiencing more advanced symptoms every year [10]. Quality of life can be impacted, at both the physical and the psychological levels, at all stages of the condition [11,12,13]. CVD also places a heavy burden on healthcare systems, representing up to 3% of total healthcare budgets in developed countries [14,15,16,17].
The diagnosis of CVD is predominantly clinical. Initial evaluation consists of a thorough history and physical examination, with clinical classification of disease according to the Clinical Etiology Anatomy Pathophysiology (CEAP) criteria [7]. Treatment aims to improve both venous function as well as the signs and symptoms of CVD. In parallel, quality of life (QoL) is viewed as an important outcome measure as it correlates strongly with disease severity and treatment-induced improvements [18].
CVD represents a large, under-estimated healthcare need, and, in order to ensure optimal treatment practices and outcomes, there is a need to assess the characteristics of CVD in large samples of the general population worldwide, and to examine the way it is managed in everyday clinical practice. Observational studies are able to address the utility of a therapy as it is actually employed in practice, in a real-world environment, and are invaluable for providing information on effectiveness and health-related QoL.
The VEIN STEP observational study was conducted to obtain wide-scale, international information on the management of CVD in daily clinical practice, and on the effectiveness of conservative treatments on CVD signs and symptoms as well as on health-related QoL. Findings from the Moroccan arm of the study were published in 2021 [19]. The current publication presents findings for the global VEIN STEP population in nine countries.
Methods
Between June 2020 and March 2022, GPs, phlebologists, dermatologists, and surgeons in hospitals, clinics, or private practice were asked to select consecutive patients whenever possible who met the following set of inclusion criteria: aged ≥ 18 years; consulting spontaneously or referred for treatment of symptomatic CVD; diagnosis of CVD according to physician’s judgement; and informed patient consent. Non-inclusion criteria comprised: current treatment for CVD either with a venoactive drug or compression therapy; lower limb arterial disease; presence of concomitant disease or treatment that may interfere with lower limb pain or edema; any procedure or surgery planned during the study for CVD; and pregnancy or breastfeeding. Investigators were instructed to continue management and treatment of participants according to their usual practice, but, prior to commencing the study, a full training kit was provided, highlighting the main diagnosis principle with respect to the CEAP classification. Cost of treatment was the responsibility of the patient, and, in countries where treatment was not reimbursed, this incurred out-of-pocket expenses for the patient.
Using a combination of patient-reported outcomes and physician assessments, the primary objective of the study was to evaluate, in a real-life setting, the effectiveness of conservative treatments on CVD symptoms [visual analog scale (VAS), 4-point scale, Patient Global Impression of Change (PGIC)] and signs [Venous Clinical Severity Score (VCSS)]. Quality of life was assessed using the validated 14-item ChronIc Venous Insufficiency Questionnaire (CIVIQ-14). Secondary objectives included assessment of patient and physician satisfaction regarding the treatment prescribed, and the determination of the characteristics and of the management of the disease in real-life settings.
At the initial inclusion visit [Visit 0 (V0)], demographic characteristics, medical history, lifestyle behaviors, and current medications potentially interfering with study outcomes were recorded. After routine clinical examination of the lower limbs, patients were assigned a CEAP clinical classification [7]. Patients were asked to indicate the global intensity of their symptoms as well as intensity of each symptom (pain, heaviness, cramps, sensation of swelling) with the use of a 10-cm VAS. The intensity of paresthesia (tingling), itching, and burning sensation symptoms were assessed using a 4-point scale. Patient QoL was assessed using CIVIQ-14 [20]. The 14 items of this questionnaire cover three dimensions: pain (3 items), physical (5 items), and psychological (6 items), and are scored on a Likert scale from 1 (no symptom, sensation or trouble) to 5 (highest intensity or frequency). The questionnaire has been psychometrically and linguistically validated, and has proven to be a reliable and sensitive instrument for reporting QoL in patients with CVD [20,21,22].
Following the patient examination, physicians completed the VCSS [23, 24]. The VCSS includes ten clinical descriptors (pain, varicose veins, venous edema, skin pigmentation, inflammation, induration, number of active ulcers, duration of active ulceration, size of ulcer, and compressive therapy use), graded by severity (None = 0, Mild = 1, Moderate = 2, Severe = 3) for a total possible score of 30.
At V0, patients could be prescribed conservative treatment according to the physicians’ usual practice. This could include pharmacological or non-pharmacological treatment, such as compression therapy, oral VAD, painkillers, topical treatment. Provision of lifestyle advice was optional and dependent on the physician’s usual practice.
Follow-up visit 1 (V1) took place approximately 2 weeks later by telephone. Global symptom improvement was determined by questioning the patient and completing the PGIC questionnaire. PGIC is a 7-point scale depicting a patient’s rating of overall improvement. Patients rate their change as ‘very much improved,’ ‘much improved,’ ‘minimally improved,’ ‘no change,’ ‘minimally worse,’ ‘much worse,’ or ‘very much worse.’ For the purpose of this study, the three ‘improved’ ratings and the three ‘worsened’ ratings were grouped so that results could be presented as ‘improved’, ‘no change’, or ‘worse.’ Patients were also questioned on which symptom(s) were improved at V1 and the time to improvement. Additionally, patients were questioned about adherence to therapy.
Follow-up visit 2 (V2) took place approximately 4 weeks after inclusion to assess global and individual symptom intensity (VAS or 4-point scale), symptom improvement (PGIC), QoL (CIVIQ-14), and physician-reported symptom severity (VCSS). Patients’ and physicians’ satisfaction with treatment was a secondary endpoint and was assessed at V2 using a 5-item scale (very unsatisfied, unsatisfied, neutral, satisfied, very satisfied). An additional, optional telephone follow-up visit 3 (V3) could be conducted around 8 weeks after inclusion to assess PGIC.
Patients were questioned about adherence to treatment and lifestyle recommendations and about adverse events at each contact with the physician. A summary of the assessments performed at each visit is provided in Table 1.
VEIN STEP was a non-interventional study according to the European Regulation EU No. 536/2014. Physicians were instructed to continue management and treatment of participants according to their usual practice. No specific investigations or therapies were prescribed as part of this study, and, therefore, patient care was not influenced. The study was conducted in accordance with the principles of the Declaration of Helsinki. All patients provided written informed consent to participate in the study. The study was registered (NCT04574375) and approved by local institutional ethics committees.
Statistical Analysis
Continuous variables are described using arithmetic mean ± standard deviation (SD), and median [interquartile range (IQR)], and 95% two-sided confidence intervals (CI) were calculated when appropriate using the standard method (standard normal distribution). Categorical variables are presented using number and percentages. Missing data were not replaced. Within-group differences were evaluated by a paired t test or Wilcoxon signed-rank test for continuous variables with normal or skewed distribution, respectively. McNemar's test or Cochran’s Q test were used for categorical variables, according to the number of modalities of the variable.
Effectiveness parameters of the most commonly used treatments, MPFF and diosmin, either as monotherapy or in combination with compression, were compared using ranked ANCOVA, and Quade's method was used to transform the rank of the response variable and the covariate (baseline). The model was adjusted for country, CEAP class and baseline characteristics with a statistically significant between-group difference.
Statistical significance was assumed when P < 0.05 (2-sided). All statistical analyses were performed with the SAS® software version 9.4 or higher.
Results
Baseline Demographic and Patient Characteristics
Physician and Patient Characteristics
A total of 250 investigators (56.4% female) participated in VEIN STEP with a mean time in clinical practice of 19.5 ± 10.8 years. The majority of the investigators were GPs (68.3%), but other specialties were represented including vascular surgeons, dermatologists, general surgeons, angiologists, and phlebologists. Investigators enrolled 6236 subjects. The analysis set comprised 6084 (97.6%) subjects with available data for the main variables and at least one follow-up visit. Subjects were recruited from the following countries: China (n = 293); Morocco (n = 3425); Romania (n = 1000); Mexico (n = 794); Central America (Honduras, Costa Rica, Panama, Dominican Republic) (n = 87); and Ukraine (n = 485).
A visual examination was performed in 5861 participants (96.3%) and was combined with additional diagnostic techniques in 1166 (19.2%) including: Doppler in 883 (75.7%); duplex sonography in 311 (26.7%); and other in 24 (2.1%). Doppler was performed most frequently in severe classes (C5–C6) and duplex sonography was mostly used in early stages (C0–C1).
A total of 5534 (91.0%) subjects attended visit V1, 5863 (96.4%) V2, and 3434 (56.4%) the optional 8-week follow-up visit (V3). Attendance at visits V0–V2 was reported for 5324 (87.5%) subjects, and attendance at visits V0–V3 for 3320 (54.6%). A decision to undergo an interventional procedure was a reason for study withdrawal and concerned a total of 12 (0.2%) patients: 2 patients at V1, 6 patients at V2, and 4 patients at V3. The CEAP classifications of the patients undergoing an interventional procedure ranged from C1 to C5. No data were collected after patient withdrawal or after the end of the study.
Mean age of participants was 50.6 ± 13.8 years and mean body mass index was 28.0 ± 4.9 kg/m2. In the overall population, there was a higher proportion of women than men (78% vs. 22%), Patients’ baseline and demographic characteristics by CEAP class are shown in Table 2.
Among the women in the study, two-thirds (69.9%) were multiparous, and the mean number of births was 2.8 ± 1.7, with a mean time since last delivery of 20.8 ± 13.7 years; 17.1% of the female population were taking birth control pills, and 1.8% estrogen replacement therapy.
A sedentary lifestyle was reported for 40.0% of patients, 28.6% reported their occupation required spending more than 5 h standing per day, and 15.8% more than 5 h sitting. A family history of CVD was reported in 35.1%. In 27.1%, the first signs or symptoms of CVD had appeared before the age of 30 years. Hypertension was present in 20.2%, diabetes (type 1 or type 2) in 13.3%, and dysthyroidism in 3.7%. Current smokers comprised 11.7% of the study population, and 82.6% had never smoked.
A small proportion of patients also suffered from other venous disorders including deep vein thrombosis (1.7%), post-thrombotic syndrome (0.7%), and pelvic congestion syndrome (0.3%); hemorrhoidal disease was reported by 15.9% of participants. A quarter (27.4%) had received previous treatment for venous leg disorders: 82.9% had received an oral agent (78.2% VAD, 34.2% analgesic, 7.1% other), 55.4% had received a topical agent, and 29.9% a prescription for compression therapy (27.5% bandages, 75.1% stockings). The proportion who had received previous treatment ranged from 22.2% of C0 patients to 66.3% of C6 patients. Only 253 (4.2%) patients had previously undergone a procedure/surgery for venous disease.
The use of non-CVD concomitant treatments that could influence leg edema was reported for 336 (5.5%) patients and included diuretics, calcium channel blockers, and thyroid hormone supplements. A total of 662 (10.9%) patients were taking a painkiller for a reason other than their CVD.
CEAP Clinical Classification, CVD Signs and Symptoms and QoL at Baseline
Leg signs of CVD were frequently reported by the patients. Leg telangiectases, reticular veins, or spider veins were reported by 76.0% of patients, varicose veins by 69.1%, edema by 66.7%, erythema by 16.4%, trophic disorders by 15.2%, and leg ulcers by 3.9%.
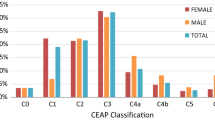
Most patients, with roughly equal numbers of men and women, were classed as C2 (varicose veins) or C3 (edema) (Fig. 1). A greater proportion of women than men were classed as C1 (telangiectasies or reticular veins), whereas more men than women were classed as C4a (pigmentation or eczema). Higher CEAP classifications were less frequent, but affected a greater number of men than women.
CVD symptoms were prevalent across all CEAP classes, including C0. At V0, the overall proportion of patients with pain, leg heaviness, cramps, and sensation of swelling was 94.4%, 93.8%, 83.6%, and 87.3%, respectively. Other symptoms commonly reported included paresthesia (65.5%), burning sensation (63.2%), and itching (55.2%). The mean number of symptoms across CEAP classes was 5.4 ± 1.7 with a gradual increase with each successive CEAP class. Mean global symptom intensity across the CEAP classes assessed with a 10-cm VAS was 5.17 ± 2.24, but increased in intensity across the classes from 4.47 ± 2.94 (C0) to 7.26 ± 2.13 (C6). Mean pain rating on the VAS was 4.83 ± 2.30; patients in higher CEAP classes experienced greater pain severity.
Across CEAP classes, symptoms were more likely to be experienced after prolonged standing or at the end of the day (29.5% and 33.2%, respectively). In classes C4b and above, around a third of patients experienced symptoms all of the time.
CIVIQ-14 mean global index score at baseline was 32.9 ± 20.3. QoL varied across CEAP classes, having a moderate impact in patients with a classification of C0 to C3 (mean global index score ranging from 23.5 to 36.0), and high impact from CEAP C4b to C6 (mean global score ranging from 51.4 to 56.3).
Lifestyle Advice and Conservative Treatments Prescribed at Baseline
At V0, 95.2% of patients received lifestyle advice. This included recommendations to exercise regularly and lose weight if necessary, avoid periods of prolonged standing or sitting, wear comfortable footwear, improve venous return by leg elevation, regular leg movement, and massage, and the importance of skin hygiene.
Nearly all patients were prescribed at least one conservative treatment for their CVD at V0. Oral VAD were the most common, prescribed to 95.8% of patients, either as monotherapy (25.5% of patients) or in combination (Fig. 2). Among the VADs, MPFF was the most widely prescribed agent [75.5% of which 20.6% as monotherapy (n = 1235 patients)]; other VADs included diosmin (18.8%), ruscus extract (0.9%), proanthocyanidins (0.6%), and sulodexide (0.4%). Other conservative treatments were: compression (52%), topical treatment (31.5%), and analgesic (34.4%), which were very rarely prescribed as monotherapy. Conservative treatments differed according to CEAP classification. Among C0–C3 patients, the most commonly prescribed agents were VADs with or without compression. VAD monotherapy was prescribed in 47.6% of C1 patients and in 9.8% of C4b–C6 patients.
In higher CEAP classes, the proportion of patients receiving three or more conservative treatments increased to include topical treatments in addition to VADs and compression (Fig. 3).
Treatment Effectiveness
Patient-Reported Outcomes: Evolution over Time
Global Symptom Improvement Assessed with Patient Global Impression of Change
For all subjects combined, regardless of conservative treatment prescribed, improvement was already noted in 89.4% at V1 (week 2) and had increased to 96.0% by V2 (week 4). Further improvement after V2 was noted for 95.2% of patients at the optional 8-week follow-up visit (V3). Improvements were observed across all CEAP classes.
At V1, in the whole population, the symptoms that improved the most by conservative therapy were: pain (improved in 82.1% patients), heaviness (improved in 71.1%), cramps (improved in 45.5%), and sensation of swelling (improved in 46.4%). Reductions in these symptoms were observed within a mean of 8.0 ± 3.0 days.
Global Symptom Intensity Assessed with Visual Analogue Scale
VAS-assessed global symptom intensity improved following 4 weeks of conservative treatment, from a mean of 5.17 ± 2.24 at V0 to 2.82 ± 1.78 at V2 (P < 0.001). VAS improvement was observed whether VAD treatments were used as monotherapy or in combination with compression therapy, analgesics, or topical treatment (Fig. 4). Improvements were greatest in CEAP classes C4b and above, which also had the highest VAS score at baseline (worse symptom intensity). However, improvements were significant in all CEAP classes (P < 0.001).
When pain, leg heaviness, cramps, and sensation of swelling were analyzed individually, significant reductions in intensity were again achieved after 4 weeks across all CEAP classes and whether VADs were used as monotherapy or in combination (P < 0.001) (Fig. 5). The percentage of patients with paresthesia, itching, and burning sensation was also reduced at V2 compared with V0 across all CEAP classes (P < 0.001).
Quality of Life Assessed with CIVIQ-14
Conservative treatment was also associated with a significant improvement in patients’ QoL after 4 weeks assessed using CIVIQ-14. This was observed across all three CIVIQ-14 dimensions (pain, physical, and psychological) (P < 0.001) in the overall population, and in patients who received treatment with VADs, either as monotherapy or in combination with compression or topical therapy.
Patient-Reported Outcomes: MPFF Versus Diosmin
Analysis of VAS global symptom intensity scores showed that MPFF monotherapy was associated with greater reductions in intensity compared with diosmin monotherapy (– 2.46 ± 1.63 vs. – 1.91 ± 1.86; P < 0.001) (Fig. 6A). Similar findings were observed when comparing MPFF plus compression versus diosmin plus compression (Fig. 6B).
A Change in mean global symptom severity score for MPFF monotherapy versus diosmin monotherapy, and B MPFF plus compression versus diosmin plus compression. Change in mean intensity of individual symptoms between baseline and 4 weeks for C MPFF monotherapy versus diosmin monotherapy, and D MPFF plus compression versus diosmin plus compression
When symptoms were analyzed individually, reductions in intensity were significantly greater for MPFF monotherapy versus diosmin monotherapy for pain (P = 0.002), leg heaviness (P < 0.001), and sensation of swelling (P = 0.008) (Fig. 6C). There was no significant difference in the reduction in cramp intensity between monotherapy treatment groups. Reductions in intensity were significantly greater for MPFF plus compression compared with diosmin plus compression for each symptom (Fig. 6D).
PGIC analysis by treatment group revealed the greatest improvements in patients receiving MPFF, either as monotherapy or in combination with compression therapy. At V1, improvements in pain, leg heaviness, cramps and sensation of swelling were observed in 71.2%, 67.6%, 41.8%, and 40.0% of patients, respectively, receiving diosmin. Respective improvements for MPFF monotherapy were: 82.1%, 73.7%, 46.4%, and 42.8%.
Improvements in QoL assessed by CIVIQ-14 were observed with all treatments. Mean change in CIVIQ-14 global score was – 9.04 ± 6.66 for MPFF monotherapy compared with – 7.21 ± 9.52 for diosmin monotherapy (P < 0.001) (Fig. 7A). Significantly greater improvements in QoL were also achieved for the combination of MPFF and compression therapy compared with diosmin and compression (– 7.66 ± 7.96 and – 5.82 ± 6.00, respectively; P = 0.027) (Fig. 7B).
Physician Reported Outcome: VCSS
As expected, there was a strong association between the severity of CVD measured by the VCSS and the CEAP clinical classification, with median baseline scores ranging from 2 for C0 and C1 to 17 for C6. Regardless of CEAP clinical class at V0, conservative treatment led to a significant decrease in VCSS at V2 (week 4) (P < 0.001).
VCSS improvements with MPFF monotherapy were significantly greater than diosmin monotherapy (P = 0.034).
Patient and Physician Satisfaction with Treatment Prescribed
Overall, 88.5% of the subjects and 89.1% of physicians were satisfied or very satisfied with the treatment prescribed. The proportions of patients and physicians ‘satisfied’ or ‘very satisfied’ with diosmin monotherapy were 85.2% and 89.6%, respectively, and 90.2% and 92.9%, respectively, for MPFF monotherapy. High rates of satisfaction were observed whether VAD treatment, including MPFF, was prescribed as monotherapy or in combination with other conservative therapy.
Adherence to Conservative Treatment
At V2, adherence to lifestyle advice was 96.2%. Adherence to VADs was high at 97.6%, and was lower for compression (84.1%). A total of 11.1% using compression did not wear it as prescribed. The main reasons for non-adherence to compression were described as discomfort with the hosiery (41.9%), difficult to put on (23.5%), sweating (23.1%), and skin irritation including itching (18.1%).
Discussion
VEIN STEP has provided up-to-date wide-scale international data on CVD patients presenting symptoms and their management with conservative therapy in daily clinical practice. CVD affects a large proportion of the working population: in the current study, 70% of patients were aged 35–65 years of age with a median age of 50 years. The most represented CEAP classes were C1 (23.0%), C2 (31.6%), and C3 (30.7%), in line with other studies [9, 25].
Patients were mainly seen by GPs, who mostly diagnosed the disease by visual examination (96.3%). Additional examinations were performed in only 19.2% of patients, mainly Doppler in severe stages and duplex sonography in early stages. Duplex ultrasound is recommended by CVD guidelines [18] and can be used to diagnose the source of venous reflux and plan treatment. Expanded use of this modality in routine examinations would also enhance epidemiological data, for which significant heterogeneity currently exists in published studies.
More women than men were found to have lower CEAP grades, possibly because women may have been more likely to report varices or seek medical attention for this condition compared to men. Conversely, men were more likely than women to present with the most severe grades, which may reflect delayed medical consultation among men. Men have also been found to present with a higher clinical class of CVD in other studies [9, 26].
At baseline, CVD symptoms were reported by 89.6% of subjects and were present across all CEAP clinical classes. The most common reported symptoms were pain, leg heaviness, sensation of swelling, and cramps. The overall global severity of symptoms assessed with a 10-cm VAS was 5.17, indicating a relatively high level of discomfort. Intensity was high for all symptoms, even in the C0 class, and particularly at the end of the day and after prolonged standing. Despite this, only a quarter (27.4%) of patients had received previous treatment for venous leg disorders.
There is a progressive deterioration in QoL from CEAP class C0s–C6 [21]. These results are in line with previous data showing that QoL can be affected by even ‘mild’ or ‘moderate’ intensity CVD symptoms [12]. In contrast, the progressive increase in symptom severity, such as pain in patients with more advanced disease observed in our study, is controversial, since a relationship between CEAP and VAS pain scores is not consistently reported across studies [27]. Nevertheless, this highlights the importance of an early CVD diagnosis and treatment initiation in order to reduce symptoms and prevent progression to more severe forms of the disease [18].
Guidelines recommend initial treatment of CVD involving conservative measures, with lifestyle advice, VAD, and compressive stockings forming the mainstay of management [18]. In addition to lifestyle advice, nearly all patients in VEIN STEP were prescribed at least one conservative treatment for their CVD: oral VAD (95.8%), compression therapy (52%), analgesic (34.4%), and topical treatment (31.5%). Among the VADs, MPFF was the most widely prescribed agent (75.5%), followed by diosmin (18.8%); all VADs were associated with a high level of adherence. Compression therapy to decrease ambulatory venous hypertension is very effective, and was widely used in combination with VADs, but poor adherence is well-documented with rates ranging from 12 to 52% [9, 28,29,30]. In comparison, adherence rates in VEIN STEP were relatively good, with only around 1 in 10 patients not wearing their compression as prescribed.
VEIN STEP used a range of patient-reported outcomes to assess symptom severity and improvement with treatment. These outcomes provide unique information on the impact of a medical condition and its treatment from the patient’s perspective, and are increasingly recognized by regulators, clinicians, and patients as valuable tools to collect patient-centered data. The results showed that all conservative treatments were effective at improving CVD symptoms. Global symptom improvement assessed with PGIC revealed that 89% of patients had already noted improvement after 2 weeks. This had increased to 96% at 4 weeks, with 95% of patients noting continued improvement at the optional 8-week visit. At each time point, improvements were observed across all CEAP classes. PGIC revealed that treatments were particularly effective at reducing pain and leg heaviness, with improvements observed in 82% and 71% of patients, respectively. Consistent with these results, global symptom intensity analyzed using a VAS was halved from a median of 5.0 at baseline to 2.5 at V2, with significant improvements again occurring in all CEAP classes. According to VAS, significant reductions in intensity were observed for each of the main CVD symptoms individually (pain, leg heaviness, cramps, and sensation of swelling). Reductions in symptom severity also translated into improved patient QoL, both overall and across the three CIVIQ-14 dimensions of pain, physical and psychological.
While this was not a head-to-head study, it was of interest to look at study endpoints for patients treated with the two most widely prescribed VADs: MPFF and diosmin. A recent review of randomized-controlled trials comparing the two reported a significant decrease in CVD symptom intensity and global patient satisfaction after 1–6 months of treatment, without statistical differences between the two diosmin forms [31]. In the current review, we compared MPFF and diosmin with or without add-on compression after adjustment for CEAP class and baseline characteristics. Patient-reported outcome measures consistently demonstrated greater improvements in global symptom intensity and individual symptom intensity with MPFF, either as monotherapy or as part of a combination treatment with compression, which led to more pronounced improvements in QoL. Similar findings have been previously demonstrated in a randomized, double-blind trial of MPFF and diosmin in patients with CVD [32]. Furthermore, animal models of CVD have shown that MPFF treatment prevents capillary rarefaction and initiation of the venous inflammatory cascade to a significantly greater extent than diosmin alone [33, 34]. It is hypothesized that MPFF may be more effective than its isolated constituents because of a synergistic beneficial effect between the diosmin and the active flavonoid fraction of MPFF [33, 34].
Physicians used VCSS to assess treatment effectiveness and noted a reduction in CVD severity following conservative treatment, with significant improvements in VCSS scores after 4 weeks. Satisfaction with conservative treatment, particularly VADs, was high for both patients and physicians. This was the case whether VAD treatment, including MPFF, was prescribed as monotherapy or in combination with other conservative therapy. Similar findings have been observed in a smaller-scale real-world study, in which MPFF was added to conservative therapy for 6 months [35].
The results of this observational study indicate that treatment with a VAD, either as monotherapy or combined with other conservative treatments, is effective in real-world settings, and that the majority of CVD patients as well as physicians were satisfied with the treatment results. MPFF was associated with significantly greater improvements in symptoms and patient QoL when compared with diosmin. A meta-analysis of randomized clinical trials investigating the effects of MPFF on CVD signs and symptoms, and QoL, has shown that it substantially and significantly improves leg symptoms, including pain, heaviness, feeling of swelling, cramps, and functional discomfort, as well as objective signs such as edema and skin changes [36]. The number of patients who needed to be treated with MPFF to observe improvement in one patient was less than five for any symptom. Furthermore, in a recently published umbrella review of systematic literature reviews, MPFF was found to have the most comprehensive evidence base of clinical use in both randomized-controlled trials and real-world observational studies for effectiveness on QoL at all stages of CVD [37].
In successive international guidelines for CVD management [38,39,40,41], MPFF has the highest number of grade A and B level of evidence, and it is currently considered as the reference treatment among venoactive drugs [41]. It is also the only VAD with the highest level of recommendation (Grade A evidence) for improvement of QoL.
VEIN STEP complements and expands on data from other large international observational studies in CVD such as VEIN CONSULT [2, 25] and VEIN ACT [9]. It differs from VEIN ACT by providing a greater focus on the effectiveness of current CVD management from both the patient’s and the physician’s perspective, encompassing QoL assessments, PGIC, and satisfaction assessments. These aspects provide a more holistic understanding of the impact of treatments on patients' well-being and satisfaction. Moreover, while VEIN ACT covers fewer symptoms and lacks frequency information for each symptom, the results from VEIN STEP provide a more detailed understanding of symptom prevalence and impact. VEIN STEP is also set apart from earlier studies such as VEIN CONSULT, conducted 15 years ago, by its greater geographical scope, use of electronic Case Report Forms, and evolution of medical practices. It is also important to note that Vein Consult included a single visit and was cross-sectional in nature, thus lacking the evaluation of treatment effectiveness over time. Thus, while previous studies have laid the foundation, VEIN STEP builds upon this knowledge by offering a more comprehensive and contemporary evaluation of CVD management, addressing for the first time a broader spectrum of factors that influence patient outcomes and experiences. Large-scale studies such as this are necessary to supplement findings from clinical trials, and in particular to provide comparative data for available treatments.
Study Limitations
The results obtained during this study may be biased through selection of the treating physicians in each country and representativeness of the study population compared with the general population. Moreover, therapeutic options and follow-up of patients may also depend on management practices at participating sites and the qualifications of the treating physician. Investigators were instructed to continue management and treatment of participants according to their usual practice, but, prior to commencing the study, a full training kit was provided, highlighting the main diagnosis principle with respect to the CEAP classification. Duplex ultrasonography is the imaging method of choice to evaluate the venous system for the management of CVD, but nevertheless was not widely used, which may have led to a lack of objectively confirmed CVD cases. Adherence to treatment was very high in this study, despite the out-of-pocket expense of purchasing the medication in some countries. Reliance on patient self-reported data may have led to an overestimation of the true adherence level, but more accurate methods of assessing treatment adherence such as pill counts or electronic monitoring are not feasible outside the setting of a clinical trial. Other potential sources of bias include the non-randomized allocation of treatments, short duration of follow-up, focus on conservative treatments rather than interventions such as ultrasound-guided foam sclerotherapy or other endovascular procedures, possibility of incomplete survey response data, inaccuracy of self-reported behavior, and the fact that data were only collected from subjects consulting spontaneously for CVD-related complaints in daily clinical practice. VEIN STEP was an observational study and, while comparisons have been made between MPFF and diosmin, the data should be interpreted with caution. This was not a head-to-head, randomized comparison and, while adjustments were made for CEAP class and baseline characteristics, there was no control of other variables such as dose and length of therapy, which could have led to important biases. VEIN STEP included a wide geographic spread of patients from four continents, but the results may not reflect the divergence in clinical practices in countries and regions beyond those encompassed by the study.
The results of this observational research nevertheless capture important, large-scale, international data on the management of patients with CVD in daily clinical practice. The real-life setting is an asset, as highly selected clinical trial populations may not reflect actual daily practice. Attendance was high throughout the study (91% at 2 weeks and 96% at 4 weeks), and over half the study population also took part in the optional 8-week follow-up. The results therefore provide accurate and up-to-date data on global management of CVD with conservative therapies and their effectiveness. Further research with extended periods of follow-up is now warranted to provide a more comprehensive understanding of the long-term effects of conservative interventions in the management of CVD.
Conclusion
Large-scale data from clinical practice show that CVD is prevalent across all age groups and both sexes. Symptoms can be present from the outset and have a major impact on QoL. The present prospective, international, real-world study confirmed that treatment with VADs, primarily MPFF, as monotherapy or in combination with other treatments, is associated with significant improvements in CVD symptoms and signs, and in quality of life.
Change history
29 April 2024
A Correction to this paper has been published: https://doi.org/10.1007/s12325-024-02857-2
23 November 2023
A Correction to this paper has been published: https://doi.org/10.1007/s12325-023-02722-8
References
Davies AH. The seriousness of chronic venous disease: a review of real-world evidence. Adv Ther. 2019;36(Suppl 1):5–12.
Vuylsteke ME, Colman R, Thomis S, Guillaume G, Van Quickenborne D. An epidemiological survey of venous disease among general practitioner attendees in different geographical regions on the globe: the final results of the Vein Consult Program. Angiology. 2018;69(9):779–85.
Ortega MA, Fraile-Martínez O, García-Montero C, Álvarez-Mon MA, Chaowen C, Ruiz-Grande F, et al. Understanding chronic venous disease: a critical overview of its pathophysiology and medical management. J Clin Med. 2021;10(15):3239.
Ono T, Bergan JJ, Schmid-Schönbein GW, Takase S. Monocyte infiltration into venous valves. J Vasc Surg. 1998;27(1):158–66.
Takase S, Schmid-Schönbein G, Bergan JJ. Leukocyte activation in patients with venous insufficiency. J Vasc Surg. 1999;30(1):148–56.
Bergan JJ, Pascarella L, Schmid-Schönbein GW. Pathogenesis of primary chronic venous disease: Insights from animal models of venous hypertension. J Vasc Surg. 2008;47(1):183–92.
Lurie F, Passman M, Meisner M, Dalsing M, Masuda E, Welch H, et al. The 2020 update of the CEAP classification system and reporting standards. J Vasc Surg Venous Lymphat Disord. 2020;8(3):342–52.
Benigni JP, Bihari I, Rabe E, Uhl JF, Partsch H, Cornu-Thenard A, Jawien A, UIP-Union Internationale de Phlébologie. Venous symptoms in C0 and C1 patients: UIP consensus document. Int Angiol. 2013;32(3):261–5.
Bogachev V, Arribas JMJ, Baila S, Ulloa Dominguez J, Walter J, Maharaj D, Marin A. Management and evaluation of treatment adherence and effectiveness in chronic venous disorders: results of the international study VEIN Act Program. Drugs & Therapy Perspec. 2019;35:396–404.
Lee AJ, Robertson LA, Boghossian SM, Allan PL, Ruckley CV, Fowkes FG, et al. Progression of varicose veins and chronic venous insufficiency in the general population in the Edinburgh Vein Study. J Vasc Surg Venous Lymphat Disord. 2015;3:18e26.
Carradice D, Mazari FA, Samuel N, Allgar V, Hatfield J, Chetter IC. Modelling the effect of venous disease on quality of life. Br J Surg. 2011;98(8):1089–98.
Branisteanu DE, Feodor T, Baila S, Mitea IA, Vittos O. Impact of chronic venous disease on quality of life: results of Vein Alarm study. Exp Ther Med. 2019;17(2):1091–6.
Santiago FR, Ulloa J, Régnier C, Peudon T, Braund E, Fradet-Aubignat C, Gianesini S. The impact of lower limb chronic venous disease on quality of life: patient and physician perspectives. J Comp Eff Res. 2022;11(11):789–803.
Kuet ML, Lane TR, Anwar MA, Davies AH. Comparison of disease-specific quality of life tools in patients with chronic venous disease. Phlebology. 2014;29(10):648–53.
Launois R. Health-related quality-of-life scales specific for chronic venous disorders of the lower limbs. J Vasc Surg Venous Lymphat Disord. 2015;3(2):219–27.
Rabe E, Pannier F. Societal costs of chronic venous disease in CEAP C4, C5, C6 disease. Phlebology. 2010;25(Suppl 1):64–7.
Kim Y, Png CYM, Sumpio BJ, DeCarlo CS, Dua A. Defining the human and health care costs of chronic venous insufficiency. Semin Vasc Surg. 2021;34(1):59–64.
De Maeseneer MG, Kakkos SK, Aherne T, et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2022 Clinical Practice Guidelines on the Management of Chronic Venous Disease of the Lower Limbs. Eur J Vasc Endovasc Surg. 2022;63(2):184–267.
Tazi Mezalek Z, Ulloa JH. VEIN STEP: Chronic venous disorders management and treatment effectiveness evaluation in chronic venous disease, an international observational prospective study. Results from Morocco. Phlebolymphology. 2021;28(2):68–71.
Launois R, Le Moine JG, Lozano FS, Mansilha A. Construction and international validation of CIVIQ-14 (a short form of CIVIQ-20), a new questionnaire with a stable factorial structure. Qual Life Res. 2012;21(6):1051–8.
Radak DJ, Vlajinac HD, Marinković JM, Maksimović MŽ, Maksimović ZV. Quality of life in chronic venous disease patients measured by short Chronic Venous Disease Quality of Life Questionnaire (CIVIQ-14) in Serbia. J Vasc Surg. 2013;58(4):1006–13.
Le Moine JG, Fiestas-Navarrete L, Katumba K, Launois R. Psychometric validation of the 14 items ChronIc Venous Insufficiency Quality of Life Questionnaire (CIVIQ-14): confirmatory factor analysis. Eur J Vasc Endovasc Surg. 2016;51(2):268–74.
Rutherford RB, Padberg FT Jr, Comerota AJ, Kistner RL, Meissner MH, Moneta GL. Venous severity scoring: an adjunct to venous outcome assessment. J Vasc Surg. 2000;31(6):1307–12.
Vasquez MA, Rabe E, McLafferty RB, Shortell CK, Marston WA, Gillespie D, American Venous Forum Ad Hoc Outcomes Working Group, et al. Revision of the venous clinical severity score: venous outcomes consensus statement: special communication of the American Venous Forum Ad Hoc Outcomes Working Group. J Vasc Surg. 2010;52(5):1387–96.
Rabe E, Guex JJ, Puskas A, Scuderi A, Fernandez Quesada F, VCP Coordinators. Epidemiology of chronic venous disorders in geographically diverse populations: results from the Vein Consult Program. Int Angiol. 2012;31(2):105–15.
Kavousi Y, Al Adas Z, Karamanos E, Kennedy N, Kabbani LS, Lin JC. Men present with higher clinical class of chronic venous disease before endovenous catheter ablation. J Vasc Surg Venous Lymphat Disord. 2018;6(6):702–6.
Orhurhu V, Chu R, Xie K, Kamanyi GN, Salisu B, Salisu-Orhurhu M, Urits I, Kaye RJ, Hasoon J, Viswanath O, Kaye AJ, Karri J, Marshall Z, Kaye AD, Anahita D. Management of lower extremity pain from chronic venous insufficiency: a comprehensive review. Cardiol Ther. 2021;10(1):111–40.
Raju S, Hollis K, Neglen P. Use of compression stockings in chronic venous disease: patient compliance and efficacy. Ann Vasc Surg. 2007;21(6):790–5.
Moffatt CJ, Franks PJ, Doherty DC, Smithdale R, Steptoe A. Psychological factors in leg ulceration: a case-control study. Br J Dermatol. 2009;161(4):750–6.
Finlayson K, Edwards H, Courtney M. The impact of psychosocial factors on adherence to compression therapy to prevent recurrence of venous leg ulcers. J Clin Nurs. 2010;19(9–10):1289–97.
Cazaubon M, Benigni JP, Steinbruch M, Jabbour V, Gouhier-Kodas C. Is there a difference in the clinical efficacy of diosmin and micronized purified flavonoid fraction for the treatment of chronic venous disorders? Review of available evidence. Vasc Health Risk Manag. 2021;17:591–600.
Cospite M, Dominici A. Double blind study of the pharmacodynamic and clinical activities of 5682 SE in venous insufficiency. Advantages of the new micronized form. Int Angiol. 1989;8(4 Suppl):61–5.
Paysant J, Sansilvestri-Morel P, Bouskela E, Verbeuren TJ. Different flavonoids present in the micronized purified flavonoid fraction (Daflon 500 mg) contribute to its anti-hyperpermeability effect in the hamster cheek pouch microcirculation. Int Angiol. 2008;27(1):81–5.
das Graças C, de Souza M, Cyrino FZ, de Carvalho JJ, Blanc-Guillemaud V, Bouskela E. Protective effects of micronized purified flavonoid fraction (MPFF) on a novel experimental model of chronic venous hypertension. Eur J Vasc Endovasc Surg. 2018;55(5):694–702.
Bogachev V, Boldin B, Turkin P, Samenkov A, Dzhenina O. Micronized purified flavonoid fraction-based conservative treatment of chronic venous disease in a real-world setting. Future Cardiol. 2022;18(10):777–85.
Kakkos SK, Nicolaides AN. Efficacy of micronized purified flavonoid fraction (Daflon®) on improving individual symptoms, signs and quality of life in patients with chronic venous disease: a systematic review and meta-analysis of randomized double-blind placebo-controlled trials. Int Angiol. 2018;37(2):143–54.
Mansilha A, Gianesini S, Ulloa JH, Lobastov K, Wang J, Freitag A, Schaible KR, Martin M, Yaltirik P, Nicolaides AN. Pharmacological treatment for chronic venous disease: an umbrella review of systematic reviews. Int Angiol. 2022;41(3):249–57.
Nicolaides AN, Allegra C, Bergan J, Bradbury A, Cairols M, Carpentier P, et al. Management of chronic venous disorders of the lower limbs: guidelines according to scientific evidence. Int Angiol. 2008;27(1):1–59.
Gloviczki P, Comerota AJ, Dalsing MC, Eklof BG, Gillespie DL, Gloviczki ML, Society for Vascular Surgery; American Venous Forum, et al. American Venous Forum The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011;53(5 Suppl):2S-48S.
Wittens C, Davies AH, Bækgaard N, Broholm R, Cavezzi A, Chastanet S, et al. Editor’s choice—management of chronic venous disease: clinical practice guidelines of the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg. 2015;49(6):678–737.
Nicolaides A, Kakkos S, Baekgaard N, Comerota A, de Maeseneer M, Eklof B, et al. Management of chronic venous disorders of the lower limbs. Guidelines according to scientific evidence. Part I. Int Angiol. 2018;37(3):181–254.
Acknowledgements
The authors thank all participants who took part in this study.
Author Contribution
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. Zoubida Tazi Mezalek, Toni Feodor, Larisa Chernukha, Zhong Chen, Ana Rueda, Ignacio Escotto Sanchez, Alejandro José Ochoa, Joanna Chirol, Vanessa Blanc-Guillemaud, Caroline Lohier-Durel, and Jorge Hernando Ulloa contributed to the concept and design of the study, were involved in the analysis and interpretation of the data, and contributed to the drafting of the paper and approval of the final submitted version.
Funding
The study was sponsored by Servier Affaires Médicales who funded the journal's rapid service fee and the open access fee.
Medical Writing/Editorial Assistance
Editorial assistance for this paper was provided by Jenny Grice and funded by Servier Affaires Médicales.
Data Availability
Data is available from corresponding author on reasonable request.
Ethical Approval
The study was conducted in accordance with the principles of the Declaration of Helsinki. All patients provided written informed consent to participate in the study. The study was registered (NCT04574375) and approved by local institutional ethics committees. The ethics committees are listed in the supplementary material.
Conflict of Interest
Zoubida Tazi Mezalek has received research grants from Servier and has received a speaker honorarium from Servier. Ignacio Escotto has received research grants and honoraria as a speaker from Servier. Alejandro Ochoa has received honoraria from Servier during the conduct of the study, and a grant from Alfasigma outside of the submitted work. Joanna Chirol, Vanessa Blanc-Guillemaud, and Caroline Lohier-Durel are Servier employees. Toni Feodor, Ana Rueda, Larisa Chernukha, Zhong Chen, and Jorge Ulloa have no competing interests related to this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original online version of this article was revised due to update in Figure 7A.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Mezalek, Z.T., Feodor, T., Chernukha, L. et al. VEIN STEP: A Prospective, Observational, International Study to Assess Effectiveness of Conservative Treatments in Chronic Venous Disease. Adv Ther 40, 5016–5036 (2023). https://doi.org/10.1007/s12325-023-02643-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02643-6