Abstract
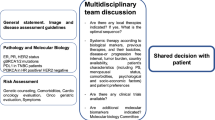
The tumor biology of human epidermal growth factor receptor 2 (HER2)-positive breast cancer (BC) promotes the development of central nervous system (CNS) metastases, with 25% of patients with HER2-positive BC developing CNS metastases. Furthermore, the incidence of HER2-positive BC brain metastases has increased in the last decades, likely because of the improved survival with targeted therapies and better detection methods. Brain metastases are detrimental to quality of life and survival and represent a challenging clinical problem, particularly in elderly women, who comprise a substantial proportion of patients diagnosed with BC and often have comorbidities or an age-related decline in organ function. Treatment options for patients with BC brain metastases include surgical resection, whole-brain radiation therapy, stereotactic radiosurgery, chemotherapy, and targeted agents. Ideally, local and systemic treatment decisions should be made by a multidisciplinary team, with input from several specialties, based on an individualized prognostic classification. In elderly patients with BC, additional age-associated conditions, such as geriatric syndromes or comorbidities, and the physiologic changes associated with aging, may impact their ability to tolerate cancer therapy and should be considered in the treatment decision-making process. This review describes the treatment options for elderly patients with HER2-positive BC and brain metastases, focusing on the importance of multidisciplinary management, the different points of view from the distinct disciplines, and the role of oncogeriatric and palliative care in this vulnerable patient group.

Similar content being viewed by others
References
Lei S, Zheng R, Zhang S, et al. Global patterns of breast cancer incidence and mortality: a population-based cancer registry data analysis from 2000 to 2020. Cancer Commun (Lond). 2021;41(11):1183–94.
National Cancer Institute: Surveillance Epidemiology and End Results Programm (SEER). Cancer Stat Facts: Female Breast Cancer. 2022. https://seer.cancer.gov/statfacts/html/breast.html. Accessed Nov 25, 2022.
Soerjomataram I, Bray F. Planning for tomorrow: global cancer incidence and the role of prevention 2020–2070. Nat Rev Clin Oncol. 2021;18(10):663–72.
Muss HB. Coming of age: breast cancer in seniors. Oncologist. 2011;16(Suppl 1):79–87.
Wolff AC, Hammond ME, Hicks DG, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. Arch Pathol Lab Med. 2014;138(2):241–56.
Laird-Fick HS, Gardiner JC, Tokala H, Patel P, Wei S, Dimitrov NV. HER2 status in elderly women with breast cancer. J Geriatr Oncol. 2013;4(4):362–7.
Jenkins EO, Deal AM, Anders CK, et al. Age-specific changes in intrinsic breast cancer subtypes: a focus on older women. Oncologist. 2014;19(10):1076–83.
Escriva-de-Romani S, Arumi M, Bellet M, Saura C. HER2-positive breast cancer: current and new therapeutic strategies. Breast. 2018;39:80–8.
Duchnowska R, Biernat W, Szostakiewicz B, et al. Correlation between quantitative HER-2 protein expression and risk for brain metastases in HER-2+ advanced breast cancer patients receiving trastuzumab-containing therapy. Oncologist. 2012;17(1):26–35.
Pestalozzi BC, Zahrieh D, Price KN, et al. Identifying breast cancer patients at risk for central nervous system (CNS) metastases in trials of the International Breast Cancer Study Group (IBCSG). Ann Oncol. 2006;17(6):935–44.
Zimmer AS, Van Swearingen AED, Anders CK. HER2-positive breast cancer brain metastasis: a new and exciting landscape. Cancer Rep (Hoboken). 2022;5(4): e1274.
Bryan S, Witzel I, Borgmann K, Oliveira-Ferrer L. Molecular mechanisms associated with brain metastases in HER2-positive and triple negative breast cancers. Cancers (Basel). 2021;13(16):4137.
Wang XY, Rosen MN, Chehade R, et al. Analysis of rates of brain metastases and association with breast cancer subtypes in Ontario, Canada. JAMA Netw Open. 2022;5(8): e2225424.
Che W, Wang Y, Wang X, Lyu J. Association between age and the presence and mortality of breast cancer synchronous brain metastases in the United States: a neglected SEER analysis. Front Public Health. 2022;10:1000415.
Hedayatizadeh-Omran A, Rafiei A, Alizadeh-Navaei R, et al. Role of HER2 in brain metastasis of breast cancer: a systematic review and meta-analysis. Asian Pac J Cancer Prev. 2015;16(4):1431–4.
Hurvitz SA, O’Shaughnessy J, Mason G, et al. Central nervous system metastasis in patients with HER2-positive metastatic breast cancer: patient characteristics, treatment, and survival from systHERs. Clin Cancer Res. 2019;25(8):2433–41.
Brufsky AM, Mayer M, Rugo HS, et al. Central nervous system metastases in patients with HER2-positive metastatic breast cancer: incidence, treatment, and survival in patients from registHER. Clin Cancer Res. 2011;17(14):4834–43.
Swain SM, Baselga J, Miles D, et al. Incidence of central nervous system metastases in patients with HER2-positive metastatic breast cancer treated with pertuzumab, trastuzumab, and docetaxel: results from the randomized phase III study CLEOPATRA. Ann Oncol. 2014;25(6):1116–21.
Sundquist M, Brudin L, Tejler G. Improved survival in metastatic breast cancer 1985–2016. Breast. 2017;31:46–50.
Vaz-Luis I, Ottesen RA, Hughes ME, et al. Impact of hormone receptor status on patterns of recurrence and clinical outcomes among patients with human epidermal growth factor-2-positive breast cancer in the National Comprehensive Cancer Network: a prospective cohort study. Breast Cancer Res. 2012;14(5):R129.
Gori S, Rimondini S, De Angelis V, et al. Central nervous system metastases in HER-2 positive metastatic breast cancer patients treated with trastuzumab: incidence, survival, and risk factors. Oncologist. 2007;12(7):766–73.
Le Rhun E, Guckenberger M, Smits M, et al. EANO-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up of patients with brain metastasis from solid tumours. Ann Oncol. 2021;32(11):1332–47.
Gennari A, Andre F, Barrios CH, et al. ESMO Clinical Practice Guideline for the diagnosis, staging and treatment of patients with metastatic breast cancer. Ann Oncol. 2021;32(12):1475–95.
Curigliano G, Castelo-Branco L, Gennari A, et al. ESMO metastatic breast cancer living guidelines, v1.0.0 May 2022. https://www.esmo.org/living-guidelines/esmo-metastatic-breast-cancer-living-guideline. Accessed Feb 21, 2023.
Ramakrishna N, Anders CK, Lin NU, et al. Management of Advanced Human Epidermal Growth Factor Receptor 2–Positive Breast Cancer and Brain Metastases: ASCO Guideline Update. J Clin Oncol. 2022;40(23):2636–55.
Cacho-Díaz B, Lorenzana-Mendoza NA, Reyes-Soto G, Ávila-Funes JA, Navarrete-Reyes AP. Neurologic manifestations of elderly patients with cancer. Aging Clin Exp Res. 2019;31(2):201–7.
Yardley DA, Tripathy D, Brufsky AM, et al. Long-term survivor characteristics in HER2-positive metastatic breast cancer from registHER. Br J Cancer. 2014;110(11):2756–64.
McKee MJ, Keith K, Deal AM, et al. A multidisciplinary breast cancer brain metastases clinic: the University of North Carolina experience. Oncologist. 2016;21(1):16–20.
Sperduto PW, Kased N, Roberge D, et al. The effect of tumor subtype on the time from primary diagnosis to development of brain metastases and survival in patients with breast cancer. J Neurooncol. 2013;112(3):467–72.
Sperduto PW, Kased N, Roberge D, et al. Summary report on the graded prognostic assessment: an accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol. 2012;30(4):419–25.
Subbiah IM, Lei X, Weinberg JS, et al. Validation and development of a modified breast graded prognostic assessment as a tool for survival in patients with breast cancer and brain metastases. J Clin Oncol. 2015;33(20):2239–45.
Gil-Gil MJ, Martinez-Garcia M, Sierra A, et al. Breast cancer brain metastases: a review of the literature and a current multidisciplinary management guideline. Clin Transl Oncol. 2014;16(5):436–46.
Puts M, Strohschein F, Oldenmenger W, et al. Position statement on oncology and cancer nursing care for older adults with cancer and their caregivers of the International Society of Geriatric Oncology Nursing and Allied Health Interest Group, the Canadian Association of Nurses in Oncology Oncology & Aging Special Interest Group, and the European Oncology Nursing Society. J Geriatr Oncol. 2021;12(7):1000–4.
Pal SK, Hurria A. Impact of age, sex, and comorbidity on cancer therapy and disease progression. J Clin Oncol. 2010;28(26):4086–93.
Tjong MC, Menjak I, Trudeau M, et al. The perceptions and expectations of older women in the establishment of the Senior Women’s Breast Cancer Clinic (SWBCC): a needs assessment study. J Cancer Educ. 2017;32(4):850–7.
Morrow ES, Dolan RD, Doughty J, Stallard S, Lannigan A, Romics L. Variation in the management of elderly patients in two neighboring breast units is due to preferences and attitudes of health professionals. Breast Cancer (Dove Med Press). 2019;11:179–88.
Zavaroni M, Oudé-Engberink A, Antoine V. French general practitioners’ attitude towards breast cancer in older women: a qualitative study. J Geriatr Oncol. 2021;12(7):1076–84.
Maltoni R, Ravaioli S, Bronte G, et al. Chronological age or biological age: what drives the choice of adjuvant treatment in elderly breast cancer patients? Transl Oncol. 2022;15(1): 101300.
Kirkhus L, SaltyteBenth J, Rostoft S, et al. Geriatric assessment is superior to oncologists’ clinical judgement in identifying frailty. Br J Cancer. 2017;117(4):470–7.
Sagara Y, Mori M, Yamamoto S, et al. Current status of advance care planning and end-of-life communication for patients with advanced and metastatic breast cancer. Oncologist. 2021;26(4):e686–93.
Nassif EF, Arsène-Henry A, Kirova YM. Brain metastases and treatment: multiplying cognitive toxicities. Expert Rev Anticancer Ther. 2019;19(4):327–41.
Angarita FA, Hoppe EJ, Ko G, Lee J, Vesprini D, Hong NJL. Why do older women avoid breast cancer surgery? A qualitative analysis of decision-making factors. J Surg Res. 2021;268:623–33.
Flannery MA, Culakova E, Canin BE, Peppone L, Ramsdale E, Mohile SG. Understanding treatment tolerability in older adults with cancer. J Clin Oncol. 2021;39(19):2150–63.
Bringuier M, Carton M, Levy C, et al. Enrollment of older metastatic breast cancer patients in first-line clinical trials: 9-year experience of the large-scale real-life multicenter French ESME cohort. Breast Cancer Res Treat. 2022;191(3):577–87.
Rostoft S, O’Donovan A, Soubeyran P, Alibhai SMH, Hamaker ME. Geriatric assessment and management in cancer. J Clin Oncol. 2021;39(19):2058–67.
Leone JP, Haraldsson B, Mott SL, McDowell BD, Chrischilles EA. Treatment patterns and survival of elderly patients with breast cancer brain metastases. Am J Clin Oncol. 2019;42(1):60–6.
Vyas A, Mantaian T, Kamat S, Kurian S, Kogut S. Association of guideline-concordant initial systemic treatment with clinical and economic outcomes among older women with metastatic breast cancer in the United States. J Geriatr Oncol. 2021;12(7):1092–9.
Borelli E, Bigi S, Potenza L, et al. Changes in cancer patients’ and caregivers’ disease perceptions while receiving early palliative care: a qualitative and quantitative analysis. Oncologist. 2021;26(12):e2274–87.
Bischoff K, O’Riordan DL, Marks AK, Sudore R, Pantilat SZ. Care planning for inpatients referred for palliative care consultation. JAMA Intern Med. 2018;178(1):48–54.
Park YH, Park MJ, Ji SH, et al. Trastuzumab treatment improves brain metastasis outcomes through control and durable prolongation of systemic extracranial disease in HER2-overexpressing breast cancer patients. Br J Cancer. 2009;100(6):894–900.
National Comprehensive Cancer Network. NCCN guidelines for patients with breast cancer, version 3.2023 - March 3, 2023. 2023. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1419. Accessed Mar 17, 2023.
Hurria A, Browner IS, Cohen HJ, et al. Senior adult oncology. J Natl Compr Canc Netw. 2012;10(2):162–209.
Balducci L, Extermann M. Management of cancer in the older person: a practical approach. Oncologist. 2000;5(3):224–37.
Mohile SG, Magnuson A, Pandya C, et al. Community oncologists’ decision-making for treatment of older patients with cancer. J Natl Compr Canc Netw. 2018;16(3):301–9.
Ommundsen N, Wyller TB, Nesbakken A, et al. Frailty is an independent predictor of survival in older patients with colorectal cancer. Oncologist. 2014;19(12):1268–75.
Droz JP, Balducci L, Bolla M, et al. Management of prostate cancer in older men: recommendations of a working group of the International Society of Geriatric Oncology. BJU Int. 2010;106(4):462–9.
Extermann M, Aapro M, Bernabei R, et al. Use of comprehensive geriatric assessment in older cancer patients: recommendations from the task force on CGA of the International Society of Geriatric Oncology (SIOG). Crit Rev Oncol Hematol. 2005;55(3):241–52.
Hamaker ME, Te Molder M, Thielen N, van Munster BC, Schiphorst AH, van Huis LH. The effect of a geriatric evaluation on treatment decisions and outcome for older cancer patients—a systematic review. J Geriatr Oncol. 2018;9(5):430–40.
Biganzoli L, Battisti NML, Wildiers H, et al. Updated recommendations regarding the management of older patients with breast cancer: a joint paper from the European Society of Breast Cancer Specialists (EUSOMA) and the International Society of Geriatric Oncology (SIOG). Lancet Oncol. 2021;22(7):e327–40.
Torregrosa-Maicas MD, Del Barco-Berrón S, Cotes-Sanchís A, Lema-Roso L, Servitja-Tormo S, Gironés-Sarrió R. Expert consensus to optimize the treatment of elderly patients with luminal metastatic breast cancer. Clin Transl Oncol. 2022;24(6):1033–46.
Kiderlen M, van de Velde CJH, Liefers GJ, group Fs. Targeted therapy in older women with breast cancer - what’s the target? Eur J Surg Oncol. 2017;43(5):944–8.
Noordijk EM, Vecht CJ, Haaxma-Reiche H, et al. The choice of treatment of single brain metastasis should be based on extracranial tumor activity and age. Int J Radiat Oncol Biol Phys. 1994;29(4):711–7.
Patchell RA, Tibbs PA, Walsh JW, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med. 1990;322(8):494–500.
Vecht CJ, Haaxma-Reiche H, Noordijk EM, et al. Treatment of single brain metastasis: radiotherapy alone or combined with neurosurgery? Ann Neurol. 1993;33(6):583–90.
Bindal RK, Sawaya R, Leavens ME, Lee JJ. Surgical treatment of multiple brain metastases. J Neurosurg. 1993;79(2):210–6.
Salvati M, Tropeano MP, Maiola V, et al. Multiple brain metastases: a surgical series and neurosurgical perspective. Neurol Sci. 2018;39(4):671–7.
Heimann M, Schafer N, Bode C, et al. Outcome of elderly patients with surgically treated brain metastases. Front Oncol. 2021;11: 713965.
Weng H-H, Noll KR, Johnson JM, et al. Accuracy of presurgical functional MR imaging for language mapping of brain tumors: a systematic review and meta-analysis. Radiology. 2018;286(2):512–23.
Bizzi A, Blasi V, Falini A, et al. Presurgical functional MR imaging of language and motor functions: validation with intraoperative electrocortical mapping. Radiology. 2008;248(2):579–89.
Haddad AF, Young JS, Berger MS, Tarapore PE. Preoperative applications of navigated transcranial magnetic stimulation. Front Neurol. 2020;11: 628903.
Leclercq D, Duffau H, Delmaire C, et al. Comparison of diffusion tensor imaging tractography of language tracts and intraoperative subcortical stimulations. J Neurosurg. 2010;112(3):503–11.
Berman JI, Berger MS, Chung SW, Nagarajan SS, Henry RG. Accuracy of diffusion tensor magnetic resonance imaging tractography assessed using intraoperative subcortical stimulation mapping and magnetic source imaging. J Neurosurg. 2007;107(3):488–94.
Sanmillan JL, Fernández-Coello A, Fernández-Conejero I, Plans G, Gabarrós A. Functional approach using intraoperative brain mapping and neurophysiological monitoring for the surgical treatment of brain metastases in the central region. J Neurosurg. 2017;126(3):698–707.
Wang JL, Elder JB. Techniques for open surgical resection of brain metastases. Neurosurg Clin N Am. 2020;31(4):527–36.
Rossi M, Sciortino T, Conti Nibali M, et al. Clinical pearls and methods for intraoperative motor mapping. Neurosurgery. 2021;88(3):457–67.
Obermueller T, Schaeffner M, Shiban E, et al. Intraoperative neuromonitoring for function-guided resection differs for supratentorial motor eloquent gliomas and metastases. BMC Neurol. 2015;15(1):211.
Ellmore TM, Beauchamp MS, O’Neill TJ, Dreyer S, Tandon N. Relationships between essential cortical language sites and subcortical pathways. J Neurosurg. 2009;111(4):755–66.
Lee S-J, Hwang S-C, Im SB, Kim B-T. Surgical resection of non-glial tumors in the motor cortex. Brain Tumor Res Treat. 2016;4(2):70–6.
Siam L, Bleckmann A, Chaung HN, et al. The metastatic infiltration at the metastasis/brain parenchyma-interface is very heterogeneous and has a significant impact on survival in a prospective study. Oncotarget. 2015;6(30):29254–67.
Baumert BG, Rutten I, Dehing-Oberije C, et al. A pathology-based substrate for target definition in radiosurgery of brain metastases. Int J Radiat Oncol Biol Phys. 2006;66(1):187–94.
Yoo H, Kim YZ, Nam BH, et al. Reduced local recurrence of a single brain metastasis through microscopic total resection. J Neurosurg. 2009;110(4):730–6.
Lee CH, Kim DG, Kim JW, et al. The role of surgical resection in the management of brain metastasis: a 17-year longitudinal study. Acta Neurochir (Wien). 2013;155(3):389–97.
Agboola O, Benoit B, Cross P, et al. Prognostic factors derived from recursive partition analysis (RPA) of Radiation Therapy Oncology Group (RTOG) brain metastases trials applied to surgically resected and irradiated brain metastatic cases. Int J Radiat Oncol Biol Phys. 1998;42(1):155–9.
Ferguson SD, Wagner KM, Prabhu SS, McAleer MF, McCutcheon IE, Sawaya R. Neurosurgical management of brain metastases. Clin Exp Metastasis. 2017;34(6–7):377–89.
Patel AJ, Suki D, Hatiboglu MA, et al. Factors influencing the risk of local recurrence after resection of a single brain metastasis. J Neurosurg. 2010;113(2):181–9.
Patel AJ, Suki D, Hatiboglu MA, Rao VY, Fox BD, Sawaya R. Impact of surgical methodology on the complication rate and functional outcome of patients with a single brain metastasis. J Neurosurg. 2015;122(5):1132–43.
Sastry R, Bi WL, Pieper S, et al. Applications of ultrasound in the resection of brain tumors. J Neuroimaging. 2017;27(1):5–15.
Lindner D, Trantakis C, Renner C, et al. Application of intraoperative 3D ultrasound during navigated tumor resection. Minim Invasive Neurosurg. 2006;49(04):197–202.
Bayer S, Maier A, Ostermeier M, Fahrig R. Intraoperative imaging modalities and compensation for brain shift in tumor resection surgery. Int J Biomed Imaging. 2017;2017:6028645.
de Lima OM, Picarelli H, Menezes MR, Amorim RL, Teixeira MJ, Bor-Seng-Shu E. Ultrasonography during surgery to approach cerebral metastases: effect on Karnofsky index scores and tumor volume. World Neurosurg. 2017;103:557–65.
Keles GE. Intracranial neuronavigation with intraoperative magnetic resonance imaging. Curr Opin Neurol. 2004;17(4):497–500.
Schichor C, Terpolilli N, Thorsteinsdottir J, Tonn J-C. Intraoperative computed tomography in cranial neurosurgery. Neurosurg Clin N Am. 2017;28(4):595–602.
Chao JH, Phillips R, Nickson JJ. Roentgen-ray therapy of cerebral metastases. Cancer. 1954;7(4):682–9.
Li J, Brown PD. The diminishing role of whole-brain radiation therapy in the treatment of brain metastases. JAMA Oncol. 2017;3(8):1023–4.
Mehta MP, Aoyama H, Gondi V. The changing role of whole-brain radiotherapy: demise or time for selective usage? JAMA Oncol. 2017;3(8):1021–2.
Soon YY, Tham IW, Lim KH, Koh WY, Lu JJ. Surgery or radiosurgery plus whole brain radiotherapy versus surgery or radiosurgery alone for brain metastases. Cochrane Database Syst Rev. 2014;3: CD009454.
Tsao MN, Xu W, Wong RK, et al. Whole brain radiotherapy for the treatment of newly diagnosed multiple brain metastases. Cochrane Database Syst Rev. 2018;1: CD003869.
Gondi V, Pugh SL, Tome WA, et al. Preservation of memory with conformal avoidance of the hippocampal neural stem-cell compartment during whole-brain radiotherapy for brain metastases (RTOG 0933): a phase II multi-institutional trial. J Clin Oncol. 2014;32(34):3810–6.
Sun B, Huang Z, Wu S, et al. Incidence and relapse risk of intracranial metastases within the perihippocampal region in 314 patients with breast cancer. Radiother Oncol. 2016;118(1):181–6.
Roos DE, Smith JG, Stephens SW. Radiosurgery versus surgery, both with adjuvant whole brain radiotherapy, for solitary brain metastases: a randomised controlled trial. Clin Oncol (R Coll Radiol). 2011;23(9):646–51.
Nieder C, Grosu AL, Gaspar LE. Stereotactic radiosurgery (SRS) for brain metastases: a systematic review. Radiat Oncol. 2014;9:155.
Mahajan A, Ahmed S, McAleer MF, et al. Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: a single-centre, randomised, controlled, phase 3 trial. Lancet Oncol. 2017;18(8):1040–8.
Kuhnol J, Kuhnol C, Vordermark D. Radiotherapy of brain metastases from breast cancer: treatment results and prognostic factors. Oncol Lett. 2016;11(5):3223–7.
Vern-Gross TZ, Lawrence JA, Case LD, et al. Breast cancer subtype affects patterns of failure of brain metastases after treatment with stereotactic radiosurgery. J Neurooncol. 2012;110(3):381–8.
Miller JA, Kotecha R, Ahluwalia MS, et al. Overall survival and the response to radiotherapy among molecular subtypes of breast cancer brain metastases treated with targeted therapies. Cancer. 2017;123(12):2283–93.
Higuchi Y, Yamamoto M, Serizawa T, et al. Stereotactic radiosurgery in elderly patients with brain metastases: comparison with non-elderly patients using database of a multi-institutional prospective observational study (JLGK0901-Elderly). J Neurooncol. 2019;144(2):393–402.
Kerschbaumer J, Demetz M, Krigers A, Nevinny-Stickel M, Thomé C, Freyschlag CF. Risk factors for radiation necrosis in patients undergoing cranial stereotactic radiosurgery. Cancers (Basel). 2021;13(19):4736.
Chen L, Shen C, Redmond KJ, et al. Use of stereotactic radiosurgery in elderly and very elderly patients with brain metastases to limit toxicity associated with whole brain radiation therapy. Int J Radiat Oncol Biol Phys. 2017;98(4):939–47.
Minniti G, Esposito V, Clarke E, et al. Stereotactic radiosurgery in elderly patients with brain metastases. J Neurooncol. 2013;111(3):319–25.
Arvanitis CD, Ferraro GB, Jain RK. The blood-brain barrier and blood-tumour barrier in brain tumours and metastases. Nat Rev Cancer. 2020;20(1):26–41.
Tamura K, Kurihara H, Yonemori K, et al. 64Cu-DOTA-trastuzumab PET imaging in patients with HER2-positive breast cancer. J Nucl Med. 2013;54(11):1869–75.
Leung HW, Chan AL. Trastuzumab-induced cardiotoxicity in elderly women with HER-2-positive breast cancer: a meta-analysis of real-world data. Expert Opin Drug Saf. 2015;14(11):1661–71.
Eiger D, Ponde NF, Agbor-Tarh D, et al. Long-term cardiac outcomes of patients with HER2-positive breast cancer treated in the adjuvant lapatinib and/or trastuzumab treatment optimization trial. Br J Cancer. 2020;122(10):1453–60.
Kim DY, Park MS, Youn JC, et al. Development and validation of a risk score model for predicting the cardiovascular outcomes after breast cancer therapy: the CHEMO-RADIAT score. J Am Heart Assoc. 2021;10(16): e021931.
Thill M, Lüftner D, Kolberg-Liedtke C, et al. AGO recommendations for the diagnosis and treatment of patients with locally advanced and metastatic breast cancer: update 2022. Breast Care (Basel). 2022;17(4):421–9.
Rostami R, Mittal S, Rostami P, Tavassoli F, Jabbari B. Brain metastasis in breast cancer: a comprehensive literature review. J Neurooncol. 2016;127(3):407–14.
Ponde N, Brandao M, El-Hachem G, Werbrouck E, Piccart M. Treatment of advanced HER2-positive breast cancer: 2018 and beyond. Cancer Treat Rev. 2018;67:10–20.
Miles D, Baselga J, Amadori D, et al. Treatment of older patients with HER2-positive metastatic breast cancer with pertuzumab, trastuzumab, and docetaxel: subgroup analyses from a randomized, double-blind, placebo-controlled phase III trial (CLEOPATRA). Breast Cancer Res Treat. 2013;142(1):89–99.
Brain E, Caillet P, de Glas N, et al. HER2-targeted treatment for older patients with breast cancer: an expert position paper from the International Society of Geriatric Oncology. J Geriatr Oncol. 2019;10(6):1003–13.
Murthy RK, Loi S, Okines A, et al. Tucatinib, trastuzumab, and capecitabine for HER2-positive metastatic breast cancer. N Engl J Med. 2020;382(7):597–609.
Lin NU, Borges V, Anders C, et al. Intracranial efficacy and survival with tucatinib plus trastuzumab and capecitabine for previously treated HER2-positive breast cancer with brain metastases in the HER2CLIMB trial. J Clin Oncol. 2020;38(23):2610–9.
Modi S, Saura C, Yamashita T, et al. Trastuzumab deruxtecan in previously treated HER2-positive breast cancer. N Engl J Med. 2020;382(7):610–21.
Cortés J, Kim S-B, Chung W-P, et al. Trastuzumab deruxtecan versus trastuzumab emtansine for breast cancer. New Engl J Med. 2022;386(12):1143–54.
Verma S, Miles D, Gianni L, et al. Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012;367(19):1783–91.
Krop IE, Lin NU, Blackwell K, et al. Trastuzumab emtansine (T-DM1) versus lapatinib plus capecitabine in patients with HER2-positive metastatic breast cancer and central nervous system metastases: a retrospective, exploratory analysis in EMILIA. Ann Oncol. 2015;26(1):113–9.
Bartsch R, Berghoff AS, Preusser M. Breast cancer brain metastases responding to primary systemic therapy with T-DM1. J Neurooncol. 2014;116(1):205–6.
Jacot W, Pons E, Frenel JS, et al. Efficacy and safety of trastuzumab emtansine (T-DM1) in patients with HER2-positive breast cancer with brain metastases. Breast Cancer Res Treat. 2016;157(2):307–18.
Bachelot T, Romieu G, Campone M, et al. Lapatinib plus capecitabine in patients with previously untreated brain metastases from HER2-positive metastatic breast cancer (LANDSCAPE): a single-group phase 2 study. Lancet Oncol. 2013;14(1):64–71.
Lin NU, Eierman W, Greil R, et al. Randomized phase II study of lapatinib plus capecitabine or lapatinib plus topotecan for patients with HER2-positive breast cancer brain metastases. J Neurooncol. 2011;105(3):613–20.
Metro G, Foglietta J, Russillo M, et al. Clinical outcome of patients with brain metastases from HER2-positive breast cancer treated with lapatinib and capecitabine. Ann Oncol. 2011;22(3):625–30.
Lin NU, Carey LA, Liu MC, et al. Phase II trial of lapatinib for brain metastases in patients with human epidermal growth factor receptor 2-positive breast cancer. J Clin Oncol. 2008;26(12):1993–9.
Kim IA, Moughan J, Sperduto PW, et al. NRG Oncology/RTOG 119: phase II randomized study of whole brain radiotherapy/stereotactic radiosurgery with concurrent lapatinib in patients with brain metastases from HER2-positive breast cancer—a collaborative study of NRG and KROG (NCT01622868). Int J Radiat Oncol. 2020;108:S174–5.
Morikawa A, de Stanchina E, Pentsova E, et al. Phase I study of intermittent high-dose lapatinib alternating with capecitabine for HER2-positive breast cancer patients with central nervous system metastases. Clin Cancer Res. 2019;25(13):3784–92.
Hurvitz S, Singh R, Adams B, et al. Phase Ib/II single-arm trial evaluating the combination of everolimus, lapatinib and capecitabine for the treatment of HER2-positive breast cancer with brain metastases (TRIO-US B-09). Ther Adv Med Oncol. 2018;10:1758835918807339.
Saura C, Oliveira M, Feng YH, et al. Neratinib plus capecitabine versus lapatinib plus capecitabine in HER2-positive metastatic breast cancer previously treated with ≥2 HER2-directed regimens: phase III NALA trial. J Clin Oncol. 2020;38(27):3138–49.
Hurvitz SA, Saura C, Oliveira M, et al. Efficacy of neratinib plus capecitabine in the subgroup of patients with central nervous system involvement from the NALA trial. Oncologist. 2021;26(8):e1327–38.
Partridge AH, Seah DS, King T, et al. Developing a service model that integrates palliative care throughout cancer care: the time is now. J Clin Oncol. 2014;32(29):3330–6.
den Herder-van der Eerden M, van Wijngaarden J, Payne S, et al. Integrated palliative care is about professional networking rather than standardisation of care: a qualitative study with healthcare professionals in 19 integrated palliative care initiatives in five European countries. Palliat Med. 2018;32(6):1091–102.
Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733–42.
Reljic T, Kumar A, Klocksieben FA, Djulbegovic B. Treatment targeted at underlying disease versus palliative care in terminally ill patients: a systematic review. BMJ Open. 2017;7(1): e014661.
Ferrell BR, Temel JS, Temin S, et al. Integration of palliative care into standard oncology care: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2017;35(1):96–112.
Enzinger AC, Zhang B, Schrag D, Prigerson HG. Outcomes of prognostic disclosure: associations with prognostic understanding, distress, and relationship with physician among patients with advanced cancer. J Clin Oncol. 2015;33(32):3809–16.
McDonald JC, du Manoir JM, Kevork N, Le LW, Zimmermann C. Advance directives in patients with advanced cancer receiving active treatment: attitudes, prevalence, and barriers. Support Care Cancer. 2017;25(2):523–31.
Rietjens JAC, Sudore RL, Connolly M, et al. Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care. Lancet Oncol. 2017;18(9):e543–51.
Pessina F, Navarria P, Cozzi L, et al. Outcome evaluation of HER2 breast cancer patients with limited brain metastasis. Anticancer Res. 2017;37(12):7057–62.
Kim YJ, Hui D, Zhang Y, et al. Differences in performance status assessment among palliative care specialists, nurses, and medical oncologists. J Pain Symptom Manage. 2015;49(6):1050–8 (e2).
Nieder C, Norum J, Dalhaug A, Aandahl G, Pawinski A. Radiotherapy versus best supportive care in patients with brain metastases and adverse prognostic factors. Clin Exp Metastasis. 2013;30(6):723–9.
Frisk G, Tinge B, Ekberg S, et al. Survival and level of care among breast cancer patients with brain metastases treated with whole brain radiotherapy. Breast Cancer Res Treat. 2017;166(3):887–96.
Rodin D, Banihashemi B, Wang L, et al. The brain metastases symptom checklist as a novel tool for symptom measurement in patients with brain metastases undergoing whole-brain radiotherapy. Curr Oncol. 2016;23(3):e239–47.
Acknowledgements
Funding
Medical writing assistance for this mansucript and the Rapid Service Fee were funded by Roche Farma S.A.
Medical Writing, Editorial, and Other Assistance
Medical writing assistance in the preparation of this article was provided by Anabel Herrero and Catherine Rees on behalf of Springer Healthcare Communications. Editorial assistance post submission was provided by Tracy Harrison of Springer Healthcare Communications. Support for editorial assistance was funded by Roche Farma S.A.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All named authors, Elena Galve-Calvo, Alberto Alonso-Babarro, María Martínez-García, María Pi-Figueras, Gloria Villalba, Saioa Alonso, and Jorge Contreras, contributed to the literature review, evidence selection, drafting and critical revision of the article. All authors read and approved the final manuscript for publication.
Disclosures
Elena Galve reports personal fees and non-financial support from AstraZeneca, Novartis, Roche Farma, and Pfizer; and personal fees from Celgene and Pierre Fabre, outside the submitted work. Alberto Alonso-Babarro reports other fees from Roche Farma. María Martínez-García reports personal fees and non-financial support from Roche Farma; non-financial support from Pfizer; and personal fees from Celgene and Pierre Fabre, outside the submitted work. María Pi-Figueras reports personal fees and non-financial support from Roche Farma. Gloria Villalba declares no competing interests. Saioa Alonso was an employee of Roche Farma, Spain during the preparation of this manuscript, she is currently an employee of AstraZeneca. Jorge Contreras reports personal fees from Roche and Merck.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Galve-Calvo, E., Alonso-Babarro, A., Martínez-García, M. et al. Narrative Review of Multidisciplinary Management of Central Nervous Involvement in Patients with HER2-Positive Metastatic Breast Cancer: Focus on Elderly Patients. Adv Ther 40, 3304–3331 (2023). https://doi.org/10.1007/s12325-023-02538-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02538-6