Abstract
Introduction
Vosoritide is the first approved pharmacological treatment for achondroplasia and is indicated for at-home injectable administration by a trained caregiver. This research aimed to explore parents’ and children’s experience of initiating vosoritide and administering this treatment at home.
Methods
Qualitative telephone interviews were conducted with parents of children being treated with vosoritide in France and Germany. Interviews were transcribed and analysed using thematic analysis.
Results
Fifteen parents participated in telephone interviews in September and October 2022. The median age of children in this sample was 8 years old (range 3–13 years) and children had been taking treatment from 6 weeks to 13 months. Four themes document families’ experience with vosoritide: (1) awareness of vosoritide treatment, uncovering that parents first heard of vosoritide through their own research, patient advocacy groups, or through their physicians; (2) treatment understanding and decision-making, which found that their decision to take treatment is based on a desire to relieve future medical complications and increase height for improved independence, and they consider the extent to which the treatment has severe side effects; (3) training and initiation, which showed that the hospital initiation and training sessions varied considerably both across and within countries, with different treatment centres taking different approaches; and (4) managing treatment at home brings psychological and practical challenges, which are ultimately overcome with perseverance and available support.
Conclusions
Parents and children are resilient to challenges posed by a daily injectable treatment and highly motivated to improve their quality of life. Parents are prepared to overcome short-term treatment challenges for future gains in terms of health and functional independence for their children. Greater support could ensure they have the right information to initiate treatment and manage treatment at home, which will improve parents’ and children’s experience.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Vosoritide is the first approved pharmacological treatment for achondroplasia. |
This research explores parents’ experience of their child starting vosoritide and administering this treatment at home to identify future support that can be offered. |
What was learned from the study? |
Parents are motivated to initiate treatment and maintain treatment adherence due to a strong desire to improve their child’s long-term health and increase functional independence. |
They encounter psychological and administration challenges, but they develop strategies to overcome these. |
There is a need to standardise the required training and support available to all families onboarding to vosoritide to ensure they are confident to manage the treatment at home in the short and long term. |
Introduction
Achondroplasia is the most common form of dwarfism and is due to a gain-of-function pathogenic variant in the fibroblast growth factors receptor 3 (FGFR3) gene, leading to impaired endochondral ossification, which has lifelong implications [1,2,3]. Clinical indicators of achondroplasia include short stature, disproportionately short limbs, macrocephaly with frontal bossing, midfacial retrusion, short fingers, trident-shaped hands, and joint hypermobility [1,2,3,4,5]. Complications such as foramen magnum stenosis, motor milestone delays, recurrent ear infections, hearing difficulty, sleep apnoea, teeth crowding or misalignment, genu varum, and spinal stenosis are common [2,3,4,5,6]. Pain is also a prominent symptom, particularly in the back, legs, and joints [2, 3, 7]. Older children may also struggle with low stamina and be overweight or obese [2, 3, 6]. These symptoms have major implications for children’s physical, social, and emotional development [2, 8], inhibiting children’s ability to participate fully in school activities, keep up with peers [3, 9], or engage in self-care practices [2, 3, 10, 11]. These challenges mean many children are reliant on assistance or adaptive devices to carry out typical daily tasks [2, 3, 6] and often have significant social and emotional impacts. Children with achondroplasia may feel self-conscious about being different [2], frustrated by unwanted attention, stigmatisation or bullying [2, 3, 6], or may have an overall sense that life is more difficult for them [3]. However, parents and children are highly resilient, and many exhibit increased empathy for others, receiving positive attention and support from a strong community of peers [6].
Vosoritide is the first approved pharmacological treatment for achondroplasia [12] and is approved for at-home daily injectable administration by a properly trained caregiver. The introduction of this treatment requires families to make new decisions with or for their children, and navigating new experiences for their family while managing the treatment with daily life. It is known from previous research in achondroplasia that parents consider pharmacological treatment for their child in the hope of reducing functional and social barriers, increasing independence, and minimising the effects of complications [10]. However, treatment decisions require parents to balance the perceived benefits of treatment with their child’s identity as a person with achondroplasia [10]. Regardless of whether they decide to pursue treatment or not, many parents worry whether their child will in the future be content with the decisions that they have made [6].
Research in other paediatric conditions that involve at-home injections such as growth hormone treatment has demonstrated that parents face challenges with the administration process, particularly handling and injecting, resulting in apprehension for both parent and child [13]. Parents are impacted by watching their children experience fear or pain associated with an injection and worry about causing their child pain [13, 14]. Research has also shown that growth hormone treatment interfered with daily activities and overnight travel, given the need to refrigerate the treatment, ultimately impacting dose timing and late or missed injections [13,14,15,16]. Whilst parents may report challenges with at-home injectables initially, these typically lessen over time and become part of daily life [14]. Although it is not yet known if these experiences will occur for every parent administering vosoritide, addressing these factors at an early stage will help to ensure existing care pathways and support can be improved to mitigate these challenges and reduce the risk of non-adherence. Another topic which has yet to be investigated is how parents communicate with children about vosoritide, both prior to its introduction and throughout ongoing treatment. In general, there is little evidence in paediatrics about what discussions parents have with their children about at-home injectable treatment, how treatment is introduced to the child, or how this may vary in accordance with the child’s age.
Aim of the Research
Through qualitative research, our primary aim is to gain insight into parents’ experiences of treating a child with vosoritide, which have not previously been described. The current research aims to explore a parent’s experience of their child starting a new treatment for achondroplasia; specifically aiming to understand what led to the decision to start treatment, any facilitators, and barriers to starting treatment; communication strategies between parent and child regarding treatment; experience of learning to administer treatment; and day-to-day experiences and challenges of administering treatment at home and how these are overcome. These insights are expected to inform the continued development of support for families administrating vosoritide and any future pharmacological treatments for achondroplasia.
Methods
Study Design
As a result of the exploratory nature of the research questions, a semi-structured qualitative interview design was chosen for this study. Interviews were conducted via telephone with parents of children with achondroplasia prescribed vosoritide in Germany and France as, at the time of research, these two countries had the most children prescribed treatment in Europe. This research sought the feedback of parents primarily as they are the ones administering the treatment, and we anticipated a wide variation in children’s ages in the sample, with many being too young to be interviewed. This research was reviewed and approved by the Royal College of Surgeons in Ireland Research Ethics Committee (Record ID 212587255). This study is in accordance with the Declaration of Helsinki 1964 and its later amendments.
Recruitment
Parent participants were recruited through achondroplasia patient advocacy groups in France [Association des Personnes de Petitie Taille (APPT)] and Germany [Bundesverband Kleinwüchsige Menschen und ihre Familien (BKMF)], through emailing a brief description of the study to their members. The pharmaceutical company that sponsored the study was named in the study description. Interested participants contacted a research agency, Global Perspectives, where screening determined their eligibility. Participants were considered eligible if they were over 18 years of age, fluent in German or French; a parent/primary caregiver to a child with achondroplasia; and had experience of injecting their child with vosoritide at home for at least 1 month. Participants were provided with an information sheet and consent form and asked to return the signed consent form if they wished to be interviewed. Participants provided written consent to participate in the research, have the interview audio recorded, and consented to have the data published (including verbatim quotes) that were de-identified. Once signed consent forms were returned, telephone interviews were scheduled.
Data Collection
Participation involved a one-to-one telephone interview which was audio recorded (with the participant’s consent) and lasted approximately 60 min. Telephone interviews were conducted by two trained qualitative researchers in the participant’s native language and were conducted using a semi-structured interview style (see Table 1 for sample questions), guided by topics aligned with the research objectives. The German moderator was a women in her late 50s with 25 years qualitative moderation experience across many conditions. The French moderator was in his early 40s with almost 20 years of moderation experience. After completion of the interview, participants were given a payment of €75 for their participation.
Analysis
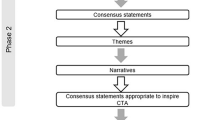
Interviews were audio recorded and transcribed into English. The transcripts were then pseudonymised (any people/place names or identifying comments were removed and transcripts were numbered). The transcripts were subsequently analysed using inductive thematic analysis [17] which involves identifying themes within and across the interviews aligned with the objectives of the research. There were two experienced qualitative analysts, both with undergraduate and postgraduate qualifications in psychology, coding and analysing the transcripts (SN & KB). MAXQDA 2022 was used to assist with coding and extraction.
Each analyst initially familiarised themselves with three randomly chosen transcripts to generate a broad understanding of the patients’ experience. After familiarisation, analysts independently developed initial codes before discussing and aligning on a common coding framework. Each analyst then independently coded the same transcript, coding every segment of text that was relevant to the objectives of the research. Afterwards, the analysts compared codes, discussed them, and amended them to ensure alignment, before dividing up the remaining transcripts and coding them independently.
Once all transcripts were coded, the analysts examined the codes together to explore patterns, similarities, and relationships that could be assigned to a particular theme. The initial themes were then reviewed and modified in the context of the data they relate to, to determine whether the data supported it sufficiently, and whether they are coherent. The analysts also examined each theme in the context of the next theme, to ensure they are relatable, but distinct from each other. The analysts finally refined and defined the essence of each theme and identified the most effective quotations to support the theme.
Results
Study Population
Fifteen parents from France (n = 7) and Germany (n = 8) participated in the research interviews. Their children ranged from ages 3 to 13 years old and had been on treatment for a median of 12 months (see Table 2 for full participant data). The sample size in this research, although representative of similar research in this field, reflects that recruitment was challenging, given that this is a new treatment. The median age of children in France was considerably higher than those in Germany as treatment in France was made available through pre-commercialisation, leading French physicians to prioritise older children for treatment to maximise potential benefit before their growth plates closed. The four themes described here follow a sequential order documenting families’ experience, from first awareness of vosoritide to decision to take treatment, training, and initiation, to managing treatment at home. See Supplementary Appendix 1 for further quotations to support the themes described.
Awareness of Vosoritide Treatment
Diagnosis of achondroplasia typically occurred prenatally or in infancy, leaving many parents concerned for their child’s future and eager to find solutions. Particularly in the case of parents of older children in the sample, when their children were infants, they were proactive in terms of searching for innovative treatment solutions through independent online research. Through this research, three parents mentioned that they became aware and learnt about vosoritide at a very early stage, in some cases whilst the drug was still in development, and monitored its progress through clinical trials, getting additional information from patient advocacy groups.
“The first time was actually already back in 2012… when my child was born. When [he] was born, we checked to see who would be the first person to contact in Germany. And then we drove to [a physician]. And, um, I think [this physician] was the one who told us about it.” (Parent of a 10-year-old, Germany)
For some parents, their physician introduced vosoritide and was a leading source of information. Specifically in France, physicians in the network of expert centres for skeletal dysplasia prioritised offering this treatment to children over the age of 7 years. Therefore, the referring expert physician systematically called eligible families to give the information and propose inclusion of the child into the vosoritide early access program. For other families, their physician may have first mentioned the treatment, but they received much of their information from the patient advocacy groups, and others reported presenting their research to their child’s physician, stressing their interest in the treatment, and repeatedly requesting they be kept informed of its development.
“I followed very closely… every 6 months or something, the news to see a bit how it was doing… so I saw the doctor who followed us… and I showed her the articles by BioMarin saying that the treatment was available since December and so… that’s it.” (Parent of an 11-year-old, France)
Patient advocacy groups typically led by parents or other family members also played a prominent role in heightening awareness of vosoritide amongst families in this sample, particularly in Germany. As with all aspects of achondroplasia, the patient advocacy groups cemented themselves as leaders in information sharing regarding vosoritide, arranging seminars from professionals and parents involved in clinical trials, and senior members of the advocacy group with experience of treating their child with vosoritide shared this experience with others. The advocacy groups also guided parents to physicians who could provide optimal care involving vosoritide and made parents aware of how to apply for treatment through pre-commercialisation routes.
“It’s always been totally dedicated to providing data and information about the study. We had numerous calls, and exchange opportunities regarding the children, and the families who participated in the study spoke, and there was even a ten-year-old who injected himself, and we could watch all that. They’re totally engaged and really also totally neutral.” (Parent of a 3-year-old, Germany)
Treatment Understanding and Decision-Making
Parents take primary responsibility for the decision to initiate treatment. Child involvement varies, with younger children not involved in the decision as parents feel their child cannot understand. For parents who have known about the treatment for several years, they considered whether they would initiate treatment at this earlier stage, even before approval. For the majority, this meant the decision to initiate treatment was made before consulting with a physician. Whilst parents may accept some input from trusted individuals such as expert physicians, patient advocacy groups, or parents with children on vosoritide, parents stressed that the decision to pursue treatment was theirs, and extended family members were often not informed until the final decision was made.
The degree to which children were involved in the treatment decision was variable across families, depending on parental certainty and the child’s age. For children that parents considered old enough (ages ranging from 6 to 13 years), parents often led the discussions with their child and provided information, sometimes shaping this information to what was important or would resonate with the child, with any concerns raised by the child alleviated by parents. Sometimes physicians or psychologists (offered as standard of care in France) talk to parents and children about treatment before a decision is made, but this is not available for every family. However, it was reported that when physicians did talk to children, they did not tailor the discussion to the child. Where the child was involved in the decision, they often had the final say.
“It involved him directly so, in any case, if he had doubts or if he hesitated… it was his decision to make. He is not 5 so….” (Parent of an 11-year-old, France)
Parents reported that child-related drivers for treatment were linked to increased height and ability to participate in valued activities as children. In this research, there was not a clear difference in motivations or concerns amongst older and younger children, as this was not directly explored. Concerns from children, where mentioned by parents, were related to needle phobia, and two children expressed concern about losing their identity as a little person.
“And so, at the beginning she flat out refused, she said she didn’t want the treatment because it scared her to… stop being a little person.” (Parent of a 12-year-old, France)
Two parents were concerned about how their child might feel about the decision in later life and did not want them to feel they had missed out on an opportunity. Similarly, parents stressed the importance of making sure children made their decision for the right reasons, e.g. not denying treatment because of needle phobia. Although parents tried their best to discuss treatment with their children, age-appropriate treatment resources were not provided, and it was raised whether their child truly understood the treatment.
Parents’ decision to initiate treatment was based on three key variables: reduction in health-related complications, gain in height to increase functional independence, and perceived side effects associated with vosoritide. With regards to complications, parents were particularly interested in reducing the need for surgery to correct bone deformity, misalignment of joints, and constriction along the spinal column. Gain in height was not important as an outcome itself but rather in relation to the reduction of height-related difficulties and increasing independence in later life. Lastly, parents also considered their decision by assessing perceived serious side effects with vosoritide. Parents felt reassured by the side effects described in the clinical trial results and, overall, they trusted the European Medicines Agency (EMA) not to approve vosoritide unless it was safe.
“During the phase III of the study, scientific publications of the results of the phase II of the study came out. They were very interesting to read, and then the approval came at some point, and I know that if something is approved, then it’s something that I trust. People who are more familiar with the matter than I have dealt with it intensively before it is approved.” (Parent of a 7-year-old, Germany)
Training and Initiation
Hospital initiation and training sessions varied considerably both across and within countries, with different treatment centres taking different approaches. These sessions varied in terms of duration, tests done, information session format, and first injection delivery. Baseline testing, including at least height, weight, X-ray, MRI, and blood tests, were typically done in the hospital; however, one parent each in France and Germany reported tests occurring in a local clinic in advance. Whilst some initiation sessions were one-to-one, the majority occurred alongside other parents and children, and who delivered this session often differed, ranging from nurses, physicians (endocrinologists, geneticists, paediatricians) or a pharmaceutical representative. In some cases, it was a combination of these disciplines delivering the session together. This difference in the sessions meant that some families did not have an opportunity to have a personalised conversation about the treatment.
Whilst first administration typically occurred in the hospital, there was variation noted in who delivered the injection and who was present in the room. Many children received the first vosoritide injection in front of other families, which was sometimes a cause for distress. Although this was often administered by a healthcare professional, parents were sometimes expected to inject their child, and reported feeling nervous in front of other families. In France, many parents just observed the first injection, as it was anticipated they would receive more hands-on training with a nurse at home, whereas in Germany, this session typically provided parents with starter kits and the opportunity to practise with saline, whilst children observed or practised on stuffed animals.
Parents in France received at-home nurse support for a period from the state to help adjust to injections for up to 30 days, a service not offered in Germany. These parents in France received at-home nurse training which taught aspects of administration which were not covered sufficiently during hospital initiation (e.g. the proper injection angle for administration and how to hold the syringe), and it was reported that parents and children were reassured by the nurse’s support and guidance. However, one parent in France felt uneasy about injecting and believed that it was the role of medical professionals to administer injections, resulting in prolonged nurse administration assistance from a private nurse as much as 12 months after initiation. Whilst two German parents suggested the opportunity for at-home feedback and training would be beneficial, most adjusted to at-home injections without additional support from a nurse. Although one-time at-home nurse support was available to German families through a pharma-sponsored patient support program (PSP), it is unclear whether the support on offer was clearly communicated as most did not avail of this service.
“I need someone who can inject and show me how to hold the needle (syringe). I know some parents locally, just had the nurse come in for the first two weeks.” (Parent of a 6-year-old, Germany)
Managing Treatment At Home
Administering vosoritide at home is a considerable psychological challenge for most parents, regardless of prior medical experience. Parents express that although the actual injection is unpleasant, the psychological challenge of injecting their own child is particularly difficult. Parents worry about hurting their child or getting the injection wrong, and the concept of breaking their child’s skin is a significant psychological barrier. Those from medical backgrounds express that whilst they may be competent in the act of injecting, the challenge of doing so to their own child is often underestimated. Whilst parents from various backgrounds reported that overcoming this barrier was difficult, most eventually did, and some parents chose to share responsibility for injecting to limit the impact on their relationship with the child.
“For the nurses when you are trained all that... I always have this feeling that for them it is all normal, you know?... But getting past the barrier of your child’s skin, all that. Actually, it’s more of that side kind of... The whole mental thing for parents” (Parent of an 11-year-old, France)
Parents face a variety of challenges when learning to inject vosoritide at home, such as air bubbles, difficulty with reconstitution, learning what angle to inject, learning which injection sites work best for their child, and broken, bent, or dropped needles. Given the challenges some parents report experiencing during the injection process, parents demonstrate tremendous perseverance and persist with treatment, and over time they discover adaptations to overcome challenges, such as using a pen to tap the syringe to remove air bubbles. Despite their resilience, parents do wish for the injection process to be simplified, with suggestions including shortening the injection process and developing a pen for children to self-administer.
“After two or three weeks, you’ve got a total lock on it. It’s very difficult at first, with these air bubbles. Knocking them out. But you get better at all that over time.” (Parent of a 13-year-old, Germany)
Whilst most children tolerated initial injections reasonably well, two children reacted poorly at first by crying, screaming, or refusing to sit still. Parents adopted a variety of strategies to help children accept and cope with injections, such as rewards, incentives, or distraction. Over time, most parents sought to establish vosoritide as a regular part of daily life, and gradually phased out the need for reinforcement, shifting instead to a focus on cuddles and family time. Many parents sought to alleviate fear by getting children involved with the injection process; however, this depended on parents’ beliefs and children’s preferences. Children of all ages were involved in the process by allowing them to help prepare the treatment or make decisions about the administration, such as injection site. Parents expressed that this was helpful in terms of giving children a sense of ownership in the process.
“I think the path there is far more important, so that she is deciding—self-determinedly—how... and when we’re going to do it... I notice that her acceptance to receive the injection is much greater when I let her co-determine this whole procedure from the beginning. That helps enormously” (Parent of a 3-year-old, Germany)
Vosoritide must be stored in a cool environment (below 30 °C for a single period up to 90 days) and be administered at approximately the same time each day, or minimally within a 12-h window [18]. Therefore, short- and long-term travel requires considerable planning and organization. Parents discuss challenges being away from home, either just for the day or for long-term travel, if it coincides with the time that the injection is required to take place. Parents need to ensure they are bringing enough treatment supply and injection materials with them, e.g. if they decide to stay longer than planned, or if a needle breaks, etc. They also need to plan that they will be able to inject at a suitable time, either back at home or while away from home. Parents also need to plan how they will keep the treatment reliably cool for the time while travelling. It was also apparent that a small number of parents have been led to believe by their physician that they cannot travel. Although parents face difficulties with travel and maintaining a consistent treatment schedule, particularly during holiday times or where children are involved in activities, this did not appear to impact adherence. Whilst some parents may have shifted the injection time slightly to accommodate activities, all reported consistently administering the injection within the allotted treatment window.
“I prefer to lose some efficiency from the treatment... by doing it sometimes 3 or 4 h later... but making the most of the moment we are living um... rather than submitting absolutely to the schedule of 19 h on holiday while we are doing something cool.” (Parent of an 8-year-old, France)
Parental persistence with treatment appears to be driven by a strong focus on outcomes, with parents willing to experience short-term difficulties if they lead to long-term quality of life benefits for their child, such as increased mobility and reduced need for surgeries. Parents and children may notice changes in height through measurement or changes in the fit of clothes and shoes, with even small increases motivating them to continue with treatment.
“When she’s walking and holding my hand, I don’t have to stretch my arm down so much, but it’s a little easier. So, something certainly has happened.” (Parent of a 13-year-old, Germany)
Discussion
This study aimed to provide insight into the experiences of parents whose children have started vosoritide treatment in France and Germany. The findings outline how families become aware of the existence of treatment, the considerations around the treatment decision, and how they learn about treatment in detail. In addition, the research provides insights into how parents are trained to administer the treatment, the challenges they encounter administering a daily injectable at home, and how they overcome these challenges.
This research showed that first awareness of treatment is driven in part by parents themselves, who proactively look for solutions early on through continuous independent research, talking to their physicians, and seeking support elsewhere if necessary. The patient advocacy groups act as advocates for others, leading, teaching, and driving awareness of how to access vosoritide. Parents were typically careful about the sources they trusted when researching achondroplasia treatments, relying mostly on clinical trial information or information shared by the patient advocacy groups. However, some parents may make their decision to initiate treatment as they explore information and attend seminars with patient advocacy groups, and not necessarily through a personalised one-to-one consultation with their physician. However, in France, parents of children older than 7 years were directly invited to initiate treatment. For parents that may not speak to a physician, it is possible that some parents could have misinterpreted or misunderstood some information, or relied on peers, raising the question of whether they had sufficient understanding when deciding whether to pursue treatment, or whether more support is needed to probe understanding or guide decision-making prior to initiation.
As in previous research, the parent’s decision to initiate treatment was driven by a desire to reduce medical complications [10] and increase height for functional independence [7, 10]. Height gain alone was not a sufficient cause to pursue treatment, and parents focused on the quality-of-life benefits that come with increased independence. Another influencing factor, not found in previous research, was the influence of findings of minimal side effects of treatment. Parents that chose the treatment were very well informed and felt as confident as they could be of the low risk of side effects. Although parents did acknowledge uncertainty about long-term outcomes, it appears that parents were making a risk–benefit assessment related to treatment, with the long-term benefits outweighing the long-term unknowns.
Previous research has highlighted the difficulty of balancing the decision to initiate treatment with the child’s identity [10]. This finding was also evident in this study, as two parents spoke of their child raising the concern of not wanting to lose their identity as a little person. Regardless of whether they did or did not decide to initiate treatment, parents were concerned that their child might question their decision, particularly for parents of younger children when parents have to make the decision for them, a finding raised previously [6]. As treatment begins to be offered to children at a younger age, more parents may have to consider this as they will not be able to ask their child for their opinion.
Parents’ approaches to child involvement vary according to the child’s age and their own beliefs about treatment. Findings suggested that parents were less likely to involve younger children in treatment decisions. For younger children, injections are positioned as something good for the child which they must do, whilst older children are given the opportunity to ask questions about treatment, and typically make the final decision. However, healthcare professionals often do not alter their explanation of treatment for children, and no child-specific information materials are currently available for families. As treatment becomes available to more parents of younger children, age-appropriate information is likely to become more critical to help parents facilitate conversations with their child if they so wish.
Parents in this sample did demonstrate concern about children’s pain and discomfort during at-home injections; however, this did not appear to lead to non-adherence. This contrasts with previous research in similar areas [14, 16]. Parents may be especially committed to persisting through challenges and identifying strategies for reducing burden to both themselves and their children given the lack of alternative treatment options [15]; however, this is a hypothesis which warrants further investigation. As in previous research, parents reported a reduction in barriers over time as the family adjusts to treatment [14]. Child refusal was not commonly mentioned in this sample, but when mentioned was typically in relation to younger children at the beginning of treatment. This may be due to young children’s (under 3 years old) inability to understand the treatment.
Parents of children treated with vosoritide experience a steep learning curve when learning to administer at-home injections, a finding which supports previous research [14]. It is important to note that families in Germany have access to a full set of vosoritide materials and a pharmaceutically sponsored PSP. However, as families in France were part of the early access program, they could only have limited access to treatment start materials or the PSP created by the pharmaceutical company. However, it should be noted that available support improved with the development of a special therapeutic workshop in late 2022.
Many parents in this sample in France were supported strongly by publicly funded home care nurses who helped to reduce the burden of multiple healthcare visits. This support may be required for vosoritide injections given the initial challenges parents can experience administering an injection to their child (and due to the need for cool storage and challenges with the injection device and reconstitution) [13, 14].
Parents also faced some challenges in terms of maintaining a consistent treatment schedule. This was especially true where parents wanted to travel, or with older children who took part in more activities evident in previous research amongst families administering growth hormone treatment [13,14,15,16]. This is something which will likely become more important in the future, as parents continue treatment over the course of years and seek to travel more and have a normal life.
The main limitations of this study centre around the participant sample. Participants were recruited through patient advocacy groups; therefore, some findings, such as the level of support from the patient advocacy groups, may not be generalisable to other families not heavily involved with them. In addition, as this research sought the opinions of parents who accepted the treatment regarding awareness and the decision to take treatment, we do not have insights from families who decided against initiating the treatment. The sample was made up of mainly mothers, which means fathers’ opinions are not well represented. The median age of children in the sample was 8 years old (see Table 1 for breakdown per country). Therefore, parents had been aware of and waiting for treatment for a long time and were potentially more well-informed compared to parents of younger children. The sample size was small, and only located in two countries, which limits the ability to generalise the findings to parents from different backgrounds and countries. However, achondroplasia is rare, and vosoritide is a new and first therapy for this condition, so it is important to capture families’ experience at this early stage. The strength of this study is that it is the first study to document, in depth, the experience of parents initiating a new treatment for achondroplasia.
Conclusion
Current awareness and information routes are driven largely by parents themselves, patient advocacy groups, and by specialist physicians in expert centres. There is an opportunity to support greater awareness through other sources, such as non-specialist physicians and other healthcare professionals caring for children with achondroplasia. Greater support to ensure parents have the right information to make a decision is needed. This research provided insight into the key aspects of decision-making: medical complications; height gain for independence; knowledge of serious side effects; and for children, loss of identity; and fear of needles. These insights can be used to frame discussions with parents and children, and tailor age-appropriate support materials to ensure that all aspects of the treatment that families have questions about can be addressed. Although all families received training, it was inconsistent and left families with some gaps in knowledge, skills, and confidence, which can impact their ability to manage treatment at home. Although parents find strategies to overcome these challenges, greater support could ensure they have the right information and support which will improve parents’ and children’s experience and the likelihood of maintaining adherence to treatment. There is an opportunity to standardise training and support materials to provide support that addresses the specific challenges patients have reported in this research.
Overall, this research has shown that parents and children are resilient to challenges and highly motivated to improve the quality of life of their children and prepared to overcome short-term treatment challenges for long-term gains in terms of health and functional independence for their children.
References
Pauli RM. Achondroplasia: a comprehensive clinical review. Orphanet J Rare Dis. 2019;14(1):1.
Pfeiffer KM, Brod M, Smith A, et al. Assessing physical symptoms, daily functioning, and well-being in children with achondroplasia. Am J Med Genet A. 2021;185(1):33–45.
Pfeiffer KM, Brod M, Smith A, Viuff D, Ota S, Charlton RW. Functioning and well-being in older children and adolescents with achondroplasia: a qualitative study. Am J Med Genet A. 2022;188(2):454–62.
Pfeiffer KM, Brod M, Smith A, Viuff D, Ota S, Charlton RW. A qualitative study of the impacts of having an infant or young child with achondroplasia on parent well-being. Orphanet J Rare Dis. 2021;16(1):351.
Pfeiffer KM, Brod M, Smith A, et al. Assessing the impacts of having a child with achondroplasia on parent well-being. Qual Life Res. 2021;30(1):203–15.
Shediac R, Moshkovich O, Gerould H, et al. Experiences of children and adolescents living with achondroplasia and their caregivers. Mol Genet Genomic Med. 2022;10(4):e1891.
Aldhouse NVJ, Kitchen H, Johnson C, et al. Key measurement concepts and appropriate clinical outcome assessments in pediatric achondroplasia clinical trials. Orphanet J Rare Dis. 2022;17(1):182.
Hoover-Fong J, Cheung MS, Fano V, et al. Lifetime impact of achondroplasia: current evidence and perspectives on the natural history. Bone. 2021;146:115872.
Lorne H, Newman CJ, Unger S. Is height important for quality of life in children with skeletal dysplasias? Eur J Med Genet. 2020;63(4): 103816.
McGraw SA, Henne JC, Nutter J, Larkin AA, Chen E. Treatment goals for achondroplasia: a qualitative study with parents and adults. Adv Ther. 2022;39(7):3378–91.
Constantinides C, Landis SH, Jarrett J, Quinn J, Ireland PJ. Quality of life, physical functioning, and psychosocial function among patients with achondroplasia: a targeted literature review. Disabil Rehabil. 2021. https://doi.org/10.1080/09638288.2021.1963853.
European Medicines Agency. Voxzogo 2022 [updated 2022 February]. https://www.ema.europa.eu/en/medicines/human/EPAR/voxzogo. Accessed 13 Mar 2023.
Graham S, Auyeung V, Weinman J. Exploring potentially modifiable factors that influence treatment non-adherence amongst pediatric growth hormone deficiency: a qualitative study. Patient Prefer Adherence. 2020;14:1889–99.
Brod M, Højbjerre L, Alolga SL, Beck JF, Wilkinson L, Rasmussen MH. Understanding treatment burden for children treated for growth hormone deficiency. Patient-Centered Outcomes Res. 2017;10:653–66.
Coutant R, Tauber M, Demaret B, et al. Treatment burden, adherence and quality of life in children with daily GH treatment in France. Endocr Connect. 2023. https://doi.org/10.1530/EC-22-0464.
Bagnasco F, Di Iorgi N, Roveda A, et al. Prevalence and correlates of adherence in children and adolescents treated with growth hormone: a multicenter Italian study. Endocr Pract. 2017;23(8):929–41.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
European Medicines Agency. Vosoritide Summary of Product Characteristics 2021 [updated 2021 December]. https://www.ema.europa.eu/en/documents/product-information/voxzogo-epar-product-information_en.pdf. Accessed 13 Mar 2023.
Acknowledgements
The authors would like to thank the parents who gave their time to share their experience for this study. Thank you to the Patient Advocacy Associations in France (Association des Personnes de Petitie Taille [APPT]) and Germany (Bundesverband Kleinwüchsige Menschen und ihre Familien [BKMF]), for support in inviting participants to participate in this study. Thank you to Global Perspectives for managing the scheduling and interviewing the participants in their local language and transcribing and translating the audio recordings. We are grateful to Emily O’Keeffe and John Doyle for their contributions to the design and method of this study.
Funding
Sponsorship for this study was funded by BioMarin Pharmaceutical, Inc, including funding the journal’s Rapid Service and Open Access Fees.
Author Contributions
S. NiMhurchadha, K. Butler, R. Argent, K. Mohnike, K. Palm, V. Cormier Daire, and G. Baujat contributed to the design and method of the study and design of interview questions. S. NiMhurchadha and K. Butler conducted the data analysis and interpretation of results and drafted the manuscripts. R. Argent, K. Mohnike, K. Palm, V. Cormier Daire, and G. Baujat contributed to a critical review of the manuscript.
Disclosures
Sinead Ni Mhurchadha and Karen Butler are employees of S3 Connected Health. Rob Ardent, Katja Palm, Genevieve Baujat, Valerie Cormier-Daire, and Klaus Mohnike have nothing to disclose.
Compliance with Ethics Guidelines
Ethical approval for this study was obtained from Royal College of Surgeons, Ireland Ethical Review Board (Record ID 212587255). Written informed consent was obtained from all participants. This study is in accordance with the Declaration of Helsinki 1964. Participants provided written consent to have the data published (including verbatim quotes) that were de-identified.
Data Availability
The data sets generated during and/or analysed during the current study are not publicly available as the full set of qualitative data is potentially identifiable, particularly given that this is rare disease and only a limited number of patients are on the treatment. In addition, participants did not consent to making their full data publicly available. The authors have provided supplementary quotes for each of the themes to provide additional context and information.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
NiMhurchadha, S., Butler, K., Argent, R. et al. Parents’ Experience of Administering Vosoritide: A Daily Injectable for Children with Achondroplasia. Adv Ther 40, 2457–2470 (2023). https://doi.org/10.1007/s12325-023-02496-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02496-z